What is the role of immunotherapy pediatric cancer treatment? Discover the positive and powerful advancements in how we fight childhood cancer. Crucial facts.
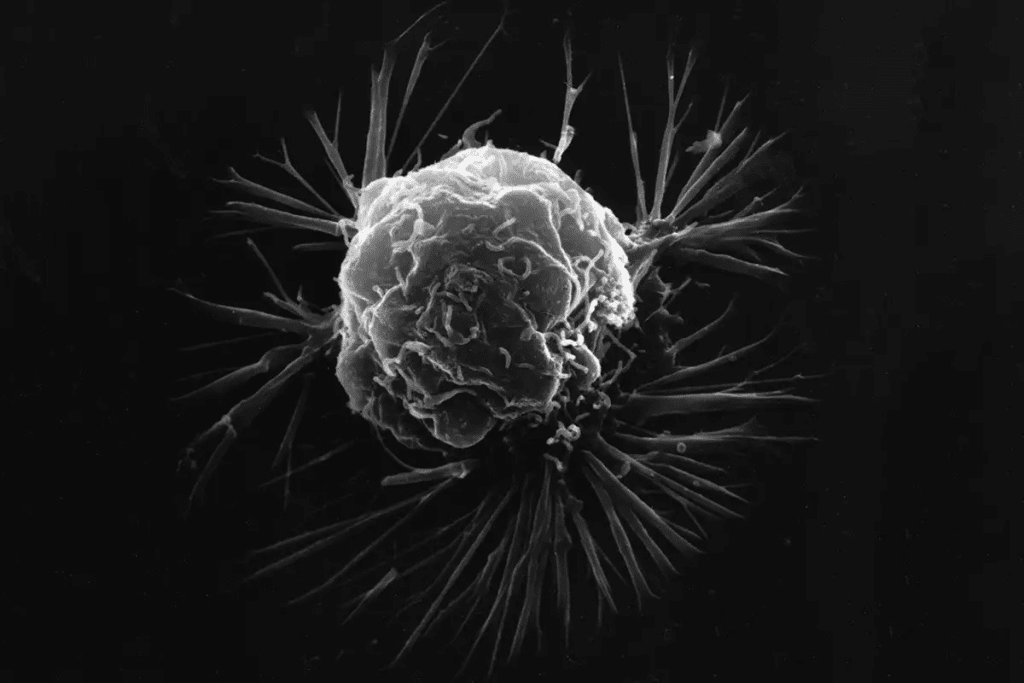
We are seeing a big change in pediatric cancer care with immunotherapy. This new method uses the immune system to fight and kill cancer cells. It brings hope for better survival rates and less harm in the long run.
One example is CAR T-cell therapy, which is very promising for some childhood leukemias. Tisagenlecleucel (Kymriah) targets the CD19 protein on leukemia cells. This gives kids with acute lymphoblastic leukemia (ALL) a new treatment option.
As we keep working on new immunotherapies, we’re seeing better results and less harm. This is changing how we treat pediatric cancer. It makes care more focused and effective.
Key Takeaways
- Immunotherapy is changing pediatric cancer care by using the immune system to fight cancer.
- CAR T-cell therapy is showing great promise in treating some childhood leukemia.
- Tisagenlecleucel (Kymriah) is a CAR T-cell therapy that targets CD19 protein on leukemia cells.
- Immunotherapy offers new hope for higher survival rates and fewer long-term side effects.
- New immunotherapies are being developed to improve treatment outcomes and reduce long-term toxicity.
The Current Landscape of Pediatric Cancer
Pediatric cancer is a big problem, with over 300,000 new cases every year worldwide. It affects not just the kids but also their families and communities.

Global and US Prevalence Statistics
Pediatric cancer is a big issue globally, with different rates in different places. In the US, thousands of kids get cancer every year. The need for better treatments, like immunotherapy, is clear.
The 85% Five-Year Survival Rate Achievement
There’s been a lot of progress in treating pediatric cancer. Now, about 85% of kids survive five years after diagnosis. This shows how far medical care has come. But 15% of kids are not as lucky, showing we need to keep working on treatments like CAR T-cell therapy.
Persistent Challenges in High-Risk and Refractory Cases
Even with the progress, some cases are harder to treat. Kids with cancers that don’t respond well need new treatments. Pediatric cancer immunotherapy advancements are key to helping these kids.
We’ve made big steps in fighting pediatric cancer, but there’s more to do. Using new treatments, like immunotherapy, is essential. It can help more kids survive and live better lives.
Traditional Treatment Approaches and Their Limitations
Pediatric cancer treatment has relied on chemotherapy, radiation, and surgery for a long time. These methods have boosted survival rates. Yet, they also have big drawbacks and long-term side effects.
Conventional Therapies: Chemotherapy, Radiation, and Surgery
Chemotherapy, radiation, and surgery are key in fighting pediatric cancer. Chemotherapy kills cancer cells with drugs. Radiation therapy uses rays to target cancer. Surgery removes tumors. But, these treatments can harm a child’s growing body.
Many kids need a stem cell transplant after CAR T-cell therapy. This shows how complex treatment can be and how much care is needed.
Long-Term Side Effects of Traditional Treatments
Traditional treatments can cause lasting harm. This includes organ damage, growth problems, and a higher risk of new cancers. These issues can really affect a child’s life after cancer.
- Organ damage from chemotherapy and radiation
- Growth and developmental issues
- Higher risk of secondary cancers
- Cognitive and emotional challenges
We need new treatments that lessen these side effects. We want to improve life for kids who have beaten cancer.
The 10-15% Relapse Rate and Treatment Resistance
Even with better treatments, 10-15% of kids with cancer don’t respond well. This shows we need new, better ways to fight cancer.
Immunotherapy, like checkpoint inhibitors in pediatric cancer, is a hopeful solution. It uses the body’s defenses to fight cancer more effectively.

Immunotherapy could lead to treatments that are more precise and less harmful. This could lower the chance of long-term side effects and boost survival rates.
Fundamentals of Immunotherapy Pediatric Cancer Treatment
Immunotherapy pediatric cancer treatment offers new hope by enhancing the body’s natural defenses to fight tumors. Immunotherapy is a new hope in fighting pediatric cancer. It boosts the body’s natural defense against tumors. This treatment is getting more attention, showing promise in treating various cancers in kids.
How Immunotherapy Harnesses the Body’s Natural Defenses
Immunotherapy uses the body’s immune system to fight cancer cells. It’s different from chemotherapy and radiation, which can harm healthy cells. Monoclonal antibodies and CAR T-cell therapy are two promising methods for treating pediatric cancers.
Differences Between Adult and Pediatric Immune Responses
Children’s immune systems are different from adults’, which is both good and challenging for immunotherapy. Kids’ immune systems are more flexible and responsive, helping in cancer treatment. But, this unpredictability makes it harder to tailor treatments. Researchers are working to understand these differences to better treat kids.
Mechanisms of Action in Various Immunotherapeutic Approaches
Immunotherapies work in different ways to fight cancer. For example, CAR T-cell therapy changes T-cells to attack cancer cells. Monoclonal antibodies target specific proteins on cancer cells for destruction. The Pediatric Immunotherapy Network (PIN) is leading the way in developing new treatments for pediatric solid tumors.
Immunotherapy in pediatric cancer treatment is showing great promise. It uses the body’s defenses and is tailored for kids. This could lead to better survival rates and fewer side effects from traditional treatments.
FDA-Approved Immunotherapies Transforming Pediatric Oncology
The FDA has changed pediatric oncology with new immunotherapies. These treatments have shown great promise in trials. They offer hope to kids with cancers that were hard to treat before.
CD19 CAR T-Cell Therapy for Acute Lymphoblastic Leukemia
Tisagenlecleucel (Kymriah) is a big step forward. It’s a CD19 CAR T-cell therapy for some Acute Lymphoblastic Leukemia (ALL). It works by taking a patient’s T-cells, changing them to attack cancer, and putting them back in.
Studies have shown it can cure patients who didn’t respond to other treatments.
It’s made a big difference for kids with ALL. It gives them a chance to be cured even when other treatments failed.
Monoclonal Antibodies for High-Risk Neuroblastoma
Monoclonal antibodies are also making a big impact. Dinutuximab (Unituxin) targets the GD2 antigen on neuroblastoma cells. It’s used with other treatments to help kids with high-risk neuroblastoma live longer.
- Targets GD2 antigen on neuroblastoma cells
- Used in combination with other therapies
- Improves survival rates in high-risk neuroblastoma
Implementation of Academic Protocols in Clinical Practice
Using these immunotherapies in real-world care depends on research. Doctors and researchers work together to make treatment plans better. This ensures kids get the best and safest care.
As we keep moving forward in pediatric oncology, using FDA-approved treatments is key. More research and trials will help us understand these therapies better. This will open up more possibilities for treating kids’ cancers.
Types of Immunotherapeutic Approaches for Childhood Cancers
Immunotherapy is a new hope for kids with cancer. It uses the body’s immune system to fight cancer. This approach is changing how we treat childhood cancers.
Several new ways to use immunotherapy are being tested. These include treatments that use cells, antibodies, and vaccines. Each method works differently to help the immune system fight cancer.
Cellular Therapies: CAR T-Cells and Beyond
Cellular therapies, like CAR T-cell therapy, are showing great promise. They modify T-cells to attack cancer cells. This has helped kids with certain types of leukemia.
A study in the New England Journal of Medicine showed CAR T-cell therapy’s success in kids with ALL. The expert said, “We’re seeing amazing results in kids with leukemia who have tried many treatments.”
“The advent of CAR T-cell therapy has revolutionized the treatment landscape for certain childhood cancers, giving families hope.”
Antibody-Based Treatments and Immunoconjugates
Antibody-based treatments are also important. Monoclonal antibodies, like dinutuximab for neuroblastoma, target cancer cells. This helps the immune system destroy them.
- Dinutuximab targets the GD2 antigen on neuroblastoma cells.
- Other monoclonal antibodies are being explored for various pediatric cancers.
- Immunoconjugates, which link antibodies to toxic substances, are also being investigated.
Checkpoint Inhibitors in Pediatric Applications
Checkpoint inhibitors help the immune system fight cancer. They are being tested in kids, but more research is needed. This is because kids’ bodies react differently to these treatments.
A recent study said, “Checkpoint inhibitors could boost the immune system’s fight against cancer. But, we need to think carefully about their use in kids.”
Cancer Vaccines and Emerging Approaches
Cancer vaccines are being researched to prevent cancer or treat it. They help the immune system recognize and attack cancer cells. These vaccines are in the early stages but show promise.
New ideas, like combining treatments and using genetic information, are also being explored. Leading Researcher said, “The future of treating childhood cancer is about making treatments fit each child’s unique needs.”
As we learn more about immunotherapy for kids with cancer, we can hope for better treatments. More research and trials are needed to make these treatments work best for kids.
Clinical Outcomes and Quality of Life Improvements
Pediatric cancer treatment has entered a new era with immunotherapy. This brings better survival rates and less long-term harm. We’re seeing big benefits for young patients and their families.
Survival Benefits in Previously Untreatable Cases
Immunotherapy has made a big difference for kids with cancers that were hard to treat. It uses the body’s immune system to fight cancer cells better. CD19 CAR T-cell therapy has shown great success in treating acute lymphoblastic leukemia (ALL), with better results than old treatments.
Reduction in Long-Term Treatment Toxicity
Immunotherapy is also good because it can lower long-term harm from treatment. Unlike old treatments, it’s more precise and doesn’t harm healthy tissues as much. This leads to fewer side effects and a better life for survivors.
Impact on Growth, Development, and Future Fertility
Immunotherapy is also helping kids grow and develop better. It reduces the need for harmful treatments, which helps avoid long-term problems. This is key for kids, as it lets them grow up healthy and have a normal life as adults.
The Half-Million Long-Term Survivors in the US
The progress we’ve made is clear with over half a million long-term survivors in the US. This shows the success of our efforts to improve treatment. As we keep working on immunotherapy and other treatments, we expect even more survivors.
Immunotherapy will be more important in treating pediatric cancer. By investing in research, we can keep improving survival rates and quality of life for kids with cancer.
Challenges and Considerations in Pediatric Immunotherapy
Pediatric immunotherapy is a game-changer, but it comes with its own set of challenges. We must tackle these complexities head-on as we use the immune system to fight cancer in kids.
Managing Unique Side Effects in Children
One big challenge is dealing with side effects in kids. CAR T-cell therapy, for example, is very effective but can cause severe issues like cytokine release syndrome (CRS) and neurological problems. It’s vital to manage these side effects well to keep young patients safe.
To tackle these risks, experts are working on better ways to monitor and treat side effects. They’re using advanced tools and creating guidelines for early detection and treatment.
Access and Availability of Advanced Treatments
Another hurdle is making sure all kids have access to these treatments. It’s not just about having them at specialized centers. We also need to overcome the logistical and financial hurdles families face.
- Improving insurance coverage for innovative therapies
- Reducing the financial burden on families through support programs
- Enhancing infrastructure at treatment centers to accommodate complex therapies
Financial Considerations for Families
The cost of pediatric immunotherapy is a huge burden for families. The expenses for treatment, hospital stays, and managing side effects can be overwhelming. It’s critical to offer financial and emotional support to help families cope.
Psychosocial Impact on Patients and Families
Pediatric immunotherapy also affects kids’ and families’ mental health. The stress of a life-threatening illness and the uncertainty of treatment outcomes can be very hard to handle.
- Providing psychological support services for patients and families
- Creating support groups for families to share experiences and advice
- Ensuring that healthcare teams are trained to address psychosocial needs
By facing these challenges head-on, we can make pediatric immunotherapy more effective and supportive for kids with cancer.
Current Research and Future Directions
Recent breakthroughs in immunotherapy have changed how we treat pediatric cancers. Research is ongoing, building on these advances. The field of pediatric cancer immunotherapy is growing fast.
Ongoing Clinical Trials for Pediatric Cancers
Many clinical trials are testing new immunotherapies for pediatric cancers. For example, the Pediatric Cancer Immunotherapy Consortium is studying new targets and treatments for solid tumors. These trials help find new treatments for cancers that don’t respond to usual therapies.
Combination Therapy Approaches
Researchers are looking into combining immunotherapy with traditional treatments like chemotherapy and radiation. This mix aims to make treatments more effective and reduce side effects. By using different treatments together, doctors hope to improve outcomes for kids with cancer.
Personalized Immunotherapy Based on Genetic Profiling
Genetic profiling has led to personalized immunotherapy in pediatric oncology. It lets researchers target specific mutations in a child’s cancer with tailored treatments. This approach could lead to better treatment results and lower relapse rates.
Potential for Treating Currently Incurable Childhood Cancers
One exciting area of research is treating cancers that are currently incurable. Immunotherapy advances offer new hope for kids with high-risk or resistant cancers. A top researcher said,
“The future of pediatric cancer treatment lies in our ability to harness the power of the immune system to target cancer cells with precision and potency.”
Continued research and trials are key to making this vision a reality. They aim to change the treatment landscape for childhood cancers.
Conclusion: The Evolving Role of Immunotherapy in Pediatric Cancer Care
Immunotherapy is changing how we treat pediatric cancer, bringing new hope to families. It includes CAR T-cell therapy, which is making treatments better and safer. This is a big step forward in fighting cancer in kids.
New ways to fight cancer, like cellular therapies and vaccines, are being developed. These advancements are not just helping kids live longer. They’re also making their lives better while they’re fighting cancer.
We’re working hard to make these new treatments available to all who need them. We aim to give kids with cancer the best care possible. We want to help create a brighter future for them.
FAQ
What is immunotherapy, and how does it work in treating pediatric cancer?
Immunotherapy uses the body’s defenses to fight cancer. It boosts the immune system to attack cancer cells. This method is tailored for different cancers, including those in children.
What are the different types of immunotherapeutic approaches being used for childhood cancers?
There are many immunotherapies for childhood cancers. These include CAR T-cell therapy, antibody treatments, checkpoint inhibitors, and cancer vaccines.
How does CAR T-cell therapy work in treating pediatric cancer?
CAR T-cell therapy takes T-cells from the blood. It makes them recognize cancer cells. Then, these T-cells are put back into the body to fight cancer.
What are the benefits of immunotherapy in pediatric cancer treatment?
Immunotherapy has many benefits for kids with cancer. It can improve survival rates and reduce side effects. It also helps survivors live better lives.
What are the challenges and considerations in pediatric immunotherapy?
Pediatric immunotherapy faces unique challenges. These include managing side effects and ensuring access to treatments. Financial and psychosocial impacts on families are also concerns.
Are there any FDA-approved immunotherapies for pediatric cancer?
Yes, the FDA has approved some immunotherapies for kids with cancer. These include CAR T-cell therapies and monoclonal antibodies. They show great promise in treatment.
What is the current state of research in pediatric immunotherapy?
Research in pediatric immunotherapy is ongoing. It includes clinical trials on new treatments. These focus on combination therapy and personalized treatments based on genetic profiles.
How does immunotherapy impact the quality of life for pediatric cancer survivors?
Immunotherapy can greatly improve the lives of cancer survivors. It reduces long-term side effects. It also helps in healthy growth and development.
Can immunotherapy be used in combination with traditional treatments for pediatric cancer?
Yes, immunotherapy can be combined with traditional treatments. This combination can improve treatment outcomes. It also reduces side effects.
What is the future of immunotherapy in pediatric cancer care?
The future of immunotherapy in pediatric cancer care looks promising. Ongoing research and new treatments hold great promise. They aim to improve outcomes and quality of life for patients.
References
- World Health Organization. (2024). Cancer in Children. Retrieved fromhttps://www.who.int/news-room/fact-sheets/detail/cancer-in-children
- American Cancer Society. (2024). Key Statistics for Childhood Cancers. Retrieved fromhttps://www.cancer.org/cancer/types/childhood-cancers/key-statistics.html
- U.S. National Library of Medicine. (2023). Immunotherapy in Pediatric Cancers: A Review. Journal of Translational Medicine, 21(1), 125.https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8943543/