Hematology patients face a high risk of infections because their immune system is weak. This is true for those getting chemotherapy or undergoing stem cell transplants. At Liv Hospital, we know how serious these infections can be. We’re dedicated to giving them the best care possible.
Opportunistic infections are a big worry for these patients. Their weak immune systems make them open to many illnesses, from pneumonia to serious viral diseases. Studies show that infections are a major cause of sickness in them. This highlights the need for good prevention and treatment plans.
Key Takeaways
- Hematology patients are at high risk of developing infections due to immunosuppression.
- Effective prevention and treatment strategies are key for better care and results.
- Liv Hospital is committed to providing top-notch care to hematology patients.
- Understanding the prevalence and impact of infections is vital for better patient outcomes.
- Compromised immune systems make hematology patients vulnerable to many illnesses.
The Compromised Immune System in Hematology Patients
Blood cancers and treatments like chemotherapy and radiation greatly affect hematology patients’ immune systems. These treatments are needed to fight cancer but can weaken the body’s defenses. This makes patients more likely to get infections.
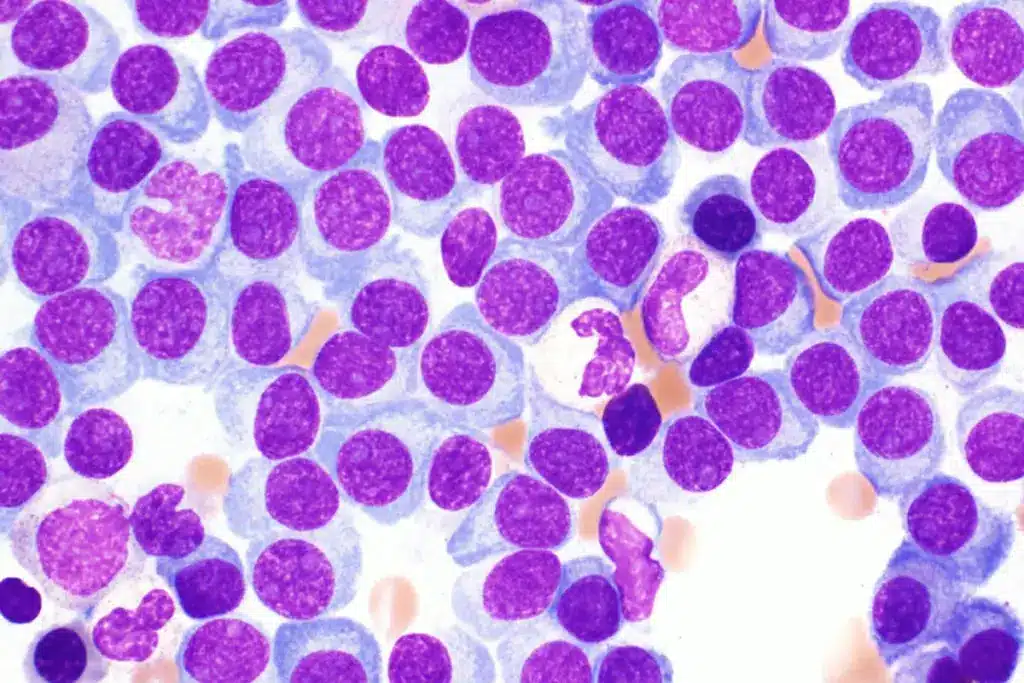
Impact of Blood Cancers on Immunity
Blood cancers, like leukemia, lymphoma, and multiple myeloma, harm the immune system. They cause the body to make abnormal white blood cells. These cells are key in fighting off infections. So, the immune system can’t fight off pathogens well.
- Leukemia: Affects the blood and bone marrow, leading to an overproduction of abnormal white blood cells.
- Lymphoma: Originates in the lymphatic system, compromising the body’s ability to fight infections.
- Multiple Myeloma: Affects plasma cells in the bone marrow, leading to a decrease in the production of normal antibodies.
Effects of Chemotherapy and Radiation

Chemotherapy and radiation therapy are common treatments for blood cancers. They are effective against cancer cells but can harm healthy cells too. This includes cells of the immune system.
Chemotherapy-induced Neutropenia: Chemotherapy can greatly lower neutrophils, a key white blood cell for fighting bacterial infections. Neutropenia is a common side effect, making patients more prone to infections.
- Chemotherapy drugs can destroy rapidly dividing cells, including those in the bone marrow.
- Radiation therapy can also suppress bone marrow function, leading to a decrease in blood cells.
It’s important to understand how blood cancers and treatments affect the immune system. This knowledge helps manage the risk of infections in hematology patients. Healthcare providers can take steps to prevent these risks and improve patient outcomes.
Risk Factors for Infection in Hematology Patients
Hematology patients face a higher risk of infections because their immune systems are weakened. This is due to several key factors. Understanding these risks is key to providing effective care and reducing the chance of infections.
Neutropenia and Its Consequences
Neutropenia, or low neutrophil levels, is a big risk for infections in these patients. Neutrophils are vital in fighting off infections. Without enough, patients are more likely to get sick from bacteria and fungi.
We try to manage neutropenia by using granulocyte-colony stimulating factor (G-CSF). This helps make more neutrophils. But, neutropenia is a serious risk that needs constant watching and quick action.
Stem Cell Transplantation Risks
Stem cell transplantation is a common treatment for blood cancers and disorders. But, it raises the risk of infections because of the conditioning regimen. This regimen includes high-dose chemotherapy and/or radiation, leading to long-lasting neutropenia and damage to mucosal barriers.
Also, the immunosuppressive state needed to prevent GVHD after transplant increases infection risk. We keep a close eye on these patients for signs of infection and take steps to prevent them.
Immunosuppressive Medications
Immunosuppressive medications are used to treat various blood conditions and prevent GVHD in transplant patients. While they are essential, they also weaken the immune system, raising the risk of infections.
Corticosteroids, in particular, increase infection risk because of their broad immunosuppressive effects. We aim to use the least amount of these medications necessary while closely watching for signs of infection.
|
Risk Factor |
Description |
Consequence |
|---|---|---|
|
Neutropenia |
Low levels of neutrophils |
Increased risk of bacterial and fungal infections |
|
Stem Cell Transplantation |
Conditioning regimen and immunosuppression |
Prolonged neutropenia and increased infection risk |
|
Immunosuppressive Medications |
Suppression of the immune system |
Increased risk of various infections |
Common Bacterial Infections
Hematology patients face a higher risk of bacterial infections. This is due to neutropenia and immunosuppression. Quick diagnosis and treatment are key to better outcomes.
Pneumonia in Hematology Patients
Pneumonia is a big problem for hematology patients. Their weakened immune system makes them more likely to get infections.
Common Causes and Symptoms: Gram-negative and Gram-positive bacteria are common culprits. Symptoms include fever, cough, and trouble breathing.
“Pneumonia is a big challenge for hematology patients. We need to be quick to suspect it and start treatment.”
— Expert Opinion
Bloodstream Infections
Bloodstream infections, or bacteremia, are serious in hematology patients. They can come from catheters or the gut.
- Sources of Infection: Catheters, mucositis, and the gut are common sources.
- Common Pathogens: Coagulase-negative staphylococci, Escherichia coli, and Klebsiella pneumoniae are often found.
Catheter-Related Infections
Catheter infections are a big worry for hematology patients. These can lead to serious blood infections and sepsis.
|
Type of Infection |
Common Pathogens |
Prevention Strategies |
|---|---|---|
|
Catheter-Related Bloodstream Infections |
Coagulase-negative staphylococci, Staphylococcus aureus |
Proper catheter insertion and maintenance, antimicrobial lock therapy |
|
Exit-Site Infections |
Staphylococcus aureus, Pseudomonas aeruginosa |
Regular exit-site care, antimicrobial ointments |
It’s important to know about these infections to manage hematology patients well. By understanding the risks and taking steps to prevent them, we can help patients get better.
Opportunistic Infections in Immunocompromised Hosts
In hematology, opportunistic infections are a big problem for those with weak immune systems. These infections take advantage of a weakened host, leading to serious health issues.
These infections are caused by pathogens that don’t usually harm healthy people but can in those with weak immunity. This is a big worry for hematology patients, as their immune systems are often weakened by their conditions or treatments like chemotherapy.
Definition and Significance
Opportunistic infections are infections caused by organisms that usually don’t harm healthy people but can in those with weak immune systems. These infections can cause serious illness and even death in people with weakened immune systems.
A study in a medical journal found that opportunistic infections are a big cause of illness and death in people with weak immune systems. This shows the need for good prevention and treatment strategies.
“The prevention and management of opportunistic infections are critical components of care for immunocompromised patients.”
– Expert Opinion
Most Common Opportunistic Pathogens
The most common opportunistic pathogens include bacteria, viruses, and fungi. Some of the notable pathogens are:
- Bacteria: Pseudomonas aeruginosa, Staphylococcus aureus
- Viruses: Cytomegalovirus (CMV), Herpes Simplex Virus (HSV)
- Fungi: Candida species, Aspergillus species
|
Pathogen Type |
Examples |
Common Infections |
|---|---|---|
|
Bacteria |
Pseudomonas aeruginosa, Staphylococcus aureus |
Pneumonia, Bloodstream infections |
|
Viruses |
Cytomegalovirus (CMV), Herpes Simplex Virus (HSV) |
CMV retinitis, HSV encephalitis |
|
Fungi |
Candida species, Aspergillus species |
Candidiasis, Invasive aspergillosis |
Knowing about these pathogens and their infections is key to managing opportunistic infections in people with weak immune systems.
Viral Infections and Reactivations
Hematology patients face a higher risk of viral infections and reactivations. These infections can cause severe problems, making quick diagnosis and treatment essential.
Herpes Zoster (Shingles)
Herpes zoster, or shingles, happens when the varicella-zoster virus reactivates. Immunocompromised patients, like those with blood cancers, are more likely to get it. It brings a painful rash, often on one side of the body.
We advise hematology patients to start antiviral therapy quickly if they get shingles. This can help avoid complications like postherpetic neuralgia.
Cytomegalovirus (CMV)
Cytomegalovirus (CMV) is a big concern for hematology patients, mainly those who have had stem cell transplants. Reactivation can cause serious issues, like pneumonia and gastrointestinal disease.
Monitoring for CMV reactivation is key in high-risk patients. Preemptive antiviral therapy is a mainstay of treatment. Regular CMV viral load checks are vital.
Respiratory Viruses: Influenza, RSV, and Metapneumovirus
Respiratory viruses, like influenza, RSV, and human metapneumovirus, are a big threat to hematology patients. These can lead to severe respiratory illnesses, often needing hospital care.
We emphasize the need for preventive measures, such as flu vaccines. Antiviral treatments should be used when needed. Early detection and isolation are also key in controlling outbreaks.
Hepatitis Reactivation in Hematology Patients
Patients with blood cancers face a high risk of hepatitis reactivation. This is because their immune systems are weak. Reactivation can cause severe hepatitis, which might stop their cancer treatment and harm their health.
Hepatitis B Reactivation
Hepatitis B reactivation is a big worry for those with blood cancers, mainly when they’re on treatments that weaken the immune system. Certain drugs can wake up the hepatitis B virus, causing a flare-up. It’s key to test for HBV before starting these treatments to spot those at risk.
Recent guidelines say patients with past HBV should get antiviral drugs to stop reactivation. The right drug and how long to take it depend on the treatment and the patient’s HBV status.
Hepatitis C Considerations
Hepatitis C reactivation is also a concern, though not as well-known as HBV. New treatments have made fighting HCV infections much better. It’s important to check for HCV in patients getting blood stem cell transplants or other treatments that weaken the immune system.
“The management of HCV infection in hematology patients involves careful consideration of the timing and choice of antiviral therapy, taking into account the patient’s underlying hematological condition and treatment plan.”
Screening and Monitoring Protocols
Good screening and monitoring are key to lowering the risk of hepatitis reactivation. All patients should be tested for HBV and HCV before starting treatments that weaken the immune system. Those with past or current HBV should have their liver function and HBV DNA levels checked regularly.
- Screening for HBV and HCV before immunosuppressive therapy
- Antiviral prophylaxis for patients at risk of HBV reactivation
- Regular monitoring of liver function and viral load
By following these steps, we can lower the risk of hepatitis reactivation in blood cancer patients. This helps them keep their cancer treatment going without interruptions.
Fungal Infections in Hematology
Hematology patients face a high risk of fungal infections. These infections can greatly affect their treatment success. Their weakened immune systems make them more susceptible.
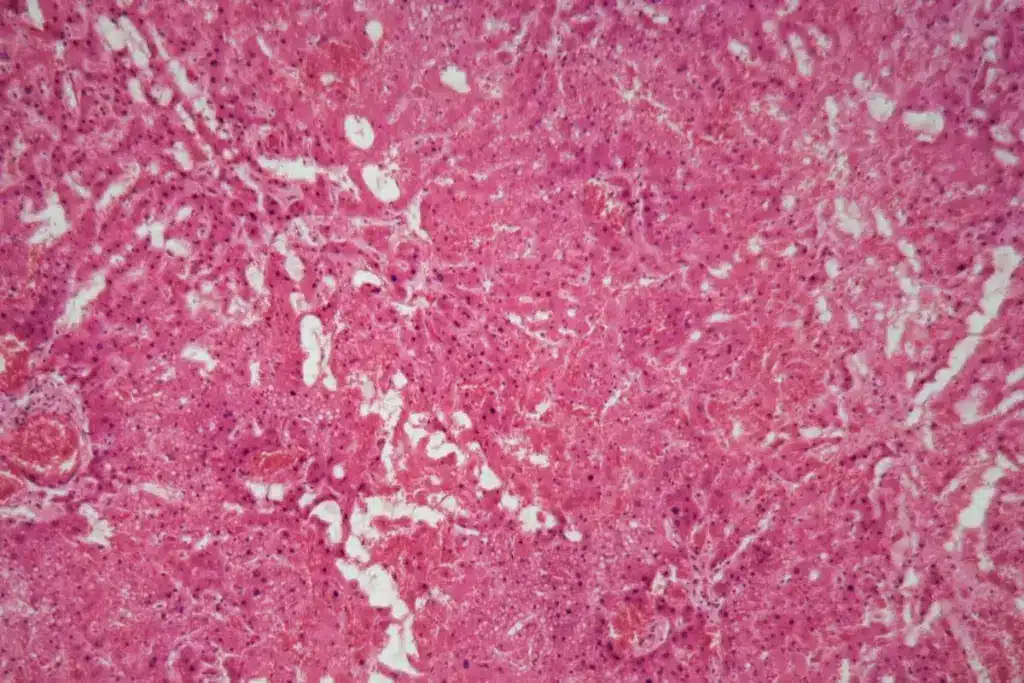
Invasive Aspergillosis
Invasive aspergillosis is a dangerous fungal infection caused by Aspergillus species. It mainly hits the lungs but can spread to other areas. We’ll cover the main points about invasive aspergillosis, including:
- Causes: Usually caught by breathing in Aspergillus spores.
- Symptoms: Symptoms include fever, cough, chest pain, and trouble breathing.
- Treatment: The main treatment is antifungal drugs like voriconazole.
Candidiasis
Candidiasis, caused by Candida species, is common in hematology patients. It can show up as skin or body infections. Key points to remember include:
- Risk Factors: Factors like neutropenia, broad-spectrum antibiotics, and central venous catheters increase risk.
- Clinical Presentation: It can appear as oral thrush, esophagitis, or candidemia.
- Management: Treatment includes antifungal drugs like fluconazole.
Pneumocystis Jirovecii Pneumonia
Pneumocystis jirovecii pneumonia (PCP) is a serious infection for those with weak immune systems. We’ll look at its:
- Pathogenesis: It can be a reactivation or a new infection.
- Symptoms: Symptoms include shortness of breath, cough, and fever.
- Prophylaxis and Treatment: Trimethoprim-sulfamethoxazole is used for prevention and treatment.
Cryptococcosis
Cryptococcosis, caused by Cryptococcus neoformans, is a serious infection. It can affect the lungs and brain. Important points include:
- Risk Factors: It’s a big risk for those with HIV/AIDS or on long-term steroids.
- Clinical Manifestations: It can cause pneumonia or meningitis.
- Treatment: Treatment starts with amphotericin B and flucytosine, followed by other steps.
In conclusion, fungal infections like invasive aspergillosis, candidiasis, pneumocystis jirovecii pneumonia, and cryptococcosis are big risks for hematology patients. Knowing about these infections is key to managing them well and improving patient care.
Infection Risk in Multiple Myeloma Patients
People with multiple myeloma face a higher risk of getting infections. This is because their immune system is weakened. Multiple myeloma is a blood cancer that harms the immune system in many ways.
Specific Vulnerabilities
There are several reasons why multiple myeloma patients are more likely to get infections. These include:
- Immunosuppression: The disease and treatments like chemotherapy weaken the immune system.
- Neutropenia: They often have low levels of neutrophils, which fight infections.
- Hypogammaglobulinemia: They also have fewer antibodies, which are key to fighting off infections.
Common Infectious Complications
Patients with multiple myeloma are at risk for many infections. These include:
- Bacterial infections: Like pneumonia and bloodstream infections, which can be very dangerous.
- Viral infections: They often see a comeback of viruses like herpes zoster (shingles).
- Fungal infections: They are more likely to get serious fungal infections, mainly when they have low neutrophils or are on corticosteroids.
Preventive Approaches
To lower the risk of infections, several steps can be taken:
- Prophylactic antibiotics: Giving antibiotics to prevent bacterial infections, mainly when neutrophil levels are low.
- Vaccinations: Vaccines against flu, pneumococcus, and other pathogens help boost the immune system.
- Immunoglobulin replacement: For those with very low antibodies, getting intravenous immunoglobulin can help.
By knowing the risks and taking steps to prevent them, we can help reduce infections in multiple myeloma patients. This can lead to better health outcomes for them.
Infections in Chronic Lymphocytic Leukemia
Infections are a big worry for people with chronic lymphocytic leukemia (CLL). CLL weakens the immune system. It happens when the body makes too many lymphocytes, which are immune cells.
Immune Dysfunction in CLL
CLL patients often have a weak immune system. This is because of the disease and treatments. They might not have enough antibodies to fight off infections.
The disease makes more leukemic cells, which harm the immune system. Treatments like chemotherapy also weaken the immune system. This makes infections more likely.
Hypogammaglobulinemia and Infection Risk
Hypogammaglobulinemia makes CLL patients more likely to get infections. They have fewer antibodies, so they can’t fight off infections well. This is true for bacterial, viral, and fungal infections.
CLL patients often get infections in the respiratory tract, urinary tract, and skin. How often and how severe these infections are depends on the CLL stage and how weak the immune system is.
Preventive Strategies
Stopping infections is key in managing CLL. This includes using medicines to prevent infections, getting vaccinated, and watching for early signs of infection.
Using medicines to prevent infections is important. Vaccines are also key, even though CLL patients might not respond as well. It’s vital to catch infections early and treat them quickly to keep patients safe.
By knowing the risks and using preventive steps, we can help CLL patients live better lives. This improves their quality of life and outcomes.
Stem Cell Transplant-Related Infections
Stem cell transplantation is key for treating blood cancers. But it makes patients more likely to get infections. Knowing about these risks helps doctors give better care and improve results.
Pre-Engraftment Phase Infections
The first weeks after a stem cell transplant are risky for infections. This is because of low white blood cells and mouth sores. Patients are more likely to get bacterial and fungal infections.
Gram-negative bacteria like Escherichia coli and Pseudomonas aeruginosa are common. So are Gram-positive bacteria, like Staphylococcus epidermidis. Fungal infections, often from Candida species, are also common.
Post-Engraftment Infections
After the transplant, the risk of infections changes. Viral infections become more common. This includes viruses like cytomegalovirus (CMV) and herpes simplex virus (HSV).
Patients also face a higher risk of graft-versus-host disease (GVHD). GVHD can harm the skin, liver, and gut. This makes infections harder to manage.
Late Infections After SCT
Infections that happen more than 100 days after the transplant are tough to deal with. These often come from chronic GVHD and the need for ongoing immune suppression.
Common late infections include herpes zoster (shingles) from varicella-zoster virus (VZV). Encapsulated bacteria, like Streptococcus pneumoniae, also cause infections.
Graft-Versus-Host Disease and Infection Risk
Graft-versus-host disease is a big problem after stem cell transplants. It makes infections more likely and severe. To treat GVHD, doctors use drugs that weaken the immune system.
|
Phase |
Common Infections |
Pathogens |
|---|---|---|
|
Pre-Engraftment |
Bacterial, Fungal |
E. coli, P. aeruginosa, Candida spp. |
|
Post-Engraftment |
Viral |
CMV, HSV |
|
Late |
Viral, Bacterial |
VZV, S. pneumoniae |
Knowing about infections after stem cell transplants is key for good care. Recognizing the risks and how GVHD affects them helps doctors. This way, they can use better prevention and treatments to help patients.
Sepsis in Hematology Patients
Hematology patients face a higher risk of sepsis, a serious condition that needs quick action. Sepsis is when the body’s response to infection goes wrong, leading to organ failure. Patients with hematological conditions are more at risk due to weakened immune systems and other factors.
Early Recognition and Assessment
Spotting sepsis early is key for hematology patients. We need to watch for signs like fever, chills, and low blood pressure. The qSOFA score helps quickly spot those at risk. It looks at breathing rate, mental state, and blood pressure.
Assessing the patient involves looking at their medical history, lab results, and any infections found. Prompt imaging studies might also be needed to find the infection source.
Emergency Management Protocols
When sepsis is suspected, we start emergency protocols right away. This includes giving empirical antibiotic therapy and supportive care like fluids and oxygen. We also consider the patient’s specific hematological condition when treating.
In some cases, source control is needed, like draining abscesses or removing infected devices. Keeping a close eye on how the patient responds to treatment is vital. We adjust treatment as needed.
Outcomes and Prognostic Factors
The outcome of sepsis in hematology patients can vary a lot. It depends on how severe the sepsis is, the patient’s underlying condition, and their overall health.
Mortality rates are high for those with severe sepsis or septic shock, and even higher for those with cancer or other serious health issues. We must think about these factors when talking about prognosis and treatment with patients and their families.
Diagnosis of Infections in Hematology Patients
Diagnosing infections in hematology patients is complex. These patients often have weakened immune systems. This makes diagnosing infections a big challenge.
Clinical Evaluation Challenges
Diagnosing starts with a clinical evaluation. But, these patients often show non-specific symptoms. For example, fever might be the only sign of a serious infection.
We need to look at the patient’s medical history. This includes past infections, current treatments, and underlying conditions. This helps guide our diagnosis.
Neutropenia is a big risk for infections in these patients. It’s important to recognize infection signs in neutropenia patients. Even without typical signs like pus, an infection could be present.
Laboratory Diagnostics
Laboratory tests are key in diagnosing infections. We use:
- Complete Blood Counts (CBC) to check white blood cell counts.
- Blood cultures to find bacteria or fungi.
- Molecular diagnostic tests, like PCR, to find specific pathogens.
- Serological tests to diagnose viruses or monitor for reactivation.
These tests help us find the infection cause. This guides our treatment.
Imaging Studies
Imaging studies are vital for diagnosing infections. We use:
- Chest X-rays or CT scans for pneumonia.
- Ultrasound or CT scans for abscesses or collections.
- MRI for infections in the brain or muscles.
Imaging helps diagnose infections. It also shows how widespread they are. This guides our treatment plans.
Novel Diagnostic Approaches
New technologies are changing diagnostics. We’re seeing:
- Next-generation sequencing (NGS) to find pathogens and resistance genes.
- Biomarkers, like procalcitonin, to guide antibiotics.
- Point-of-care diagnostics for quick bedside tests.
These new methods could change how we diagnose infections. They promise faster and more accurate treatments.
Antimicrobial Prophylaxis Strategies
Antimicrobial prophylaxis is key in stopping infections in hematology patients. These patients, like those on chemotherapy or getting stem cell transplants, face a big risk of severe infections. This is because their immune systems are weak.
Antibacterial Prophylaxis
Antibacterial prophylaxis is used for patients at risk of bacterial infections, like those with low white blood cells. Fluoroquinolones are often chosen because they fight many types of bacteria. But, we must think about the risk of making bacteria resistant to antibiotics.
- Find out who needs antibacterial prophylaxis the most.
- Watch for signs of infection and change treatment if needed.
- Look at the local antibiotic resistance patterns.
Antifungal Prophylaxis
Antifungal prophylaxis is vital to stop fungal infections in hematology patients, like those with long-lasting low white blood cells or getting stem cell transplants. Triazoles like posaconazole and voriconazole are good choices because they work well against many fungi.
- Check if the patient is at risk for fungal infections.
- Pick the right antifungal based on the patient’s risk and local fungal patterns.
- Watch for infections that come back and change treatment if needed.
Antiviral Prophylaxis
Antiviral prophylaxis helps prevent viral infections and reactivations in hematology patients. Acyclovir and its prodrug valacyclovir are used to stop herpes simplex virus (HSV) and varicella-zoster virus (VZV) from coming back. For those at risk of cytomegalovirus (CMV), valganciclovir or letermovir might be used.
Balancing Benefits and Risks
Antimicrobial prophylaxis can greatly lower infection risk in hematology patients. But, it’s not without risks. We must think about side effects, drug interactions, and resistance. A careful approach, considering each patient’s risk and local resistance, is key for effective treatment.
By choosing and watching antimicrobial prophylaxis carefully, we can better care for hematology patients. This helps lower the chance of serious infections.
Vaccination Recommendations
Hematology patients need special vaccination plans to fight off infections. Vaccines are key in keeping these patients safe. They often have weakened immune systems because of their health issues or treatments.
Pre-Treatment Vaccination
Getting vaccinated before treatment is very important for hematology patients. Vaccines should be given before starting treatments that weaken the immune system. This way, the body can better fight off the vaccine.
Doctors should check if the patient has had all needed vaccines before starting treatment. This helps prevent sickness and lowers the chance of serious problems.
Post-Treatment Vaccination Schedule
After treatment, the right vaccines and when to get them depend on how well the immune system is working. Live vaccines are not safe for people with weakened immune systems. But, inactivated vaccines might not work as well.
Patients who have had chemotherapy or a stem cell transplant need to get vaccinated again. The type of vaccine and when to get it can change based on the transplant type and how well the immune system is recovering.
Special Considerations for Transplant Recipients
Transplant patients have special vaccination needs. For those who have had a stem cell transplant, getting vaccinated against common diseases is usually needed. This starts 6-12 months after the transplant. Inactivated vaccines are preferred, and the schedule can change based on the immune system’s strength.
It’s very important for hematologists, infectious disease doctors, and primary care doctors to work together. This ensures transplant patients get the right vaccines. This teamwork helps keep these patients safe from infections they can prevent.
Emerging Resistant Pathogens in Hematology
Emerging resistant pathogens are a big worry for hematology patients. These patients have weak immune systems. This makes them more likely to get sick from hard-to-treat bacteria and fungi.
Multidrug-Resistant Bacteria
Multidrug-resistant bacteria are a big threat to hematology patients. These bacteria don’t respond to many antibiotics. This makes treating infections hard. Common culprits include Escherichia coli, Klebsiella pneumoniae, and Pseudomonas aeruginosa.
A recent study found that these resistant bacteria are becoming more common worldwide. This makes treating patients even harder as noted in a study.
- Risk Factors: Long hospital stays, too much use of broad-spectrum antibiotics, and invasive devices.
- Prevention Strategies: Strict infection control, like hand hygiene and isolation.
Azole-Resistant Fungi
Azole-resistant fungi are also a growing worry. Aspergillus species, like Aspergillus fumigatus, have become resistant to azole antifungals. This makes treating fungal infections harder for hematology patients.
- It’s important to watch for antifungal resistance.
- Use other antifungals if resistance is suspected.
- Take steps to prevent infections in high-risk patients.
Management Strategies
Managing emerging resistant pathogens needs a team effort. This includes:
- Surveillance: Always watch for changes in resistance patterns.
- Antimicrobial Stewardship: Use antibiotics wisely to slow down resistance.
- Infection Control: Improve practices to stop resistant pathogens from spreading.
- Research and Development: Work on new treatments and tests.
By using these strategies, we can help hematology patients more. And we can fight against emerging resistant pathogens.
Conclusion: Advancing Infection Management in Hematology
Improving infection management is key to better care for hematology patients. We’ve talked about different infections like bacterial, viral, and fungal ones. We also looked at why these patients are at higher risk, like neutropenia and certain meds.
To manage infections well in hematology, we need a few strategies. These include using antibiotics wisely, getting vaccines, and treating infections early. By understanding these needs, we can improve care for these patients. This way, we can make their lives better and their outcomes better too.
FAQ
What are the most common infections in hematology patients?
Hematology patients face many infections. These include bacterial, viral, and fungal types. Common ones are pneumonia, bloodstream infections, and infections from catheters. They also face opportunistic infections like pneumocystis jirovecii pneumonia and invasive aspergillosis.
How does chemotherapy affect the immune system?
Chemotherapy weakens the immune system. It lowers the production of white blood cells, like neutrophils. This makes patients more likely to get sick. The impact depends on the type and strength of the chemotherapy.
What is the risk of infection after stem cell transplantation?
Stem cell transplantation raises the risk of infection. This is due to the conditioning regimen and immunosuppression. Patients are at risk during the pre-engraftment, post-engraftment, and late phases after SCT.
How can hepatitis reactivation be prevented in hematology patients?
To prevent hepatitis reactivation, screen patients for hepatitis B and C before treatment. Monitor liver function tests and use antiviral prophylaxis in high-risk patients.
What are the symptoms of sepsis in hematology patients?
Sepsis in hematology patients can show as fever, fast heart rate, and breathing issues. It’s important to recognize and treat it early.
How can infections be diagnosed in hematology patients?
Diagnosing infections in hematology patients is hard. Symptoms are often vague, and the immune system is weak. Tests like lab diagnostics, imaging, and molecular tests help diagnose infections.
What is the role of antimicrobial prophylaxis in hematology patients?
Antimicrobial prophylaxis helps prevent infections in hematology patients. It’s key for those with neutropenia or undergoing stem cell transplantation. The type of prophylaxis depends on the patient’s risk factors.
Are vaccinations recommended for hematology patients?
Yes, vaccinations are recommended for hematology patients. They help prevent infections. Vaccination schedules should be followed before and after treatment, with special care for transplant recipients.
How can emerging resistant pathogens be managed in hematology patients?
Emerging resistant pathogens can be managed by using alternative treatments. Infection control measures and antimicrobial stewardship are also important.
What is the importance of balancing benefits and risks of antimicrobial prophylaxis?
It’s important to balance the benefits and risks of antimicrobial prophylaxis. This helps prevent infections while avoiding resistance, side effects, and high costs.
References
- Tazi, I., et al. (2020). Infections in hematology patients: a retrospective study. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC7121965/
- Wiley Online Library. (2025). Infections in patients with hematologic malignancies. Retrieved from https://onlinelibrary.wiley.com/doi/10.1002/ajh.27565
- Nature. (2025). Respiratory viral infections in patients with hematological malignancies. Retrieved from https://www.nature.com/articles/s41598-025-05796-2
- Blood. (2024). Incidence of Infections and Survival Outcomes in Patients with Hematologic Malignancies. Retrieved from https://ashpublications.org/blood/article/144/Supplement%201/1857/528976/Incidence-of-Infections-and-Survival-Outcomes-in
- Clinical Infectious Diseases. (2011). Reactivation of hepatitis B virus in patients with hematologic malignancies. Retrieved from https://academic.oup.com/cid/article/53/8/798/386237










