Bisphosphonate treatment is key in fighting bone loss and preventing fractures in both men and women.Comprehensive guide on bisphosphonate therapy, including treatment length, common drugs, and monitoring requirements.
Bisphosphonates are medicines for osteopenia and osteoporosis. These conditions make bones thin and fragile, leading to fractures.
For over 30 years, bisphosphonate therapy has been the top choice for treating osteoporosis management.
At Liv Hospital, we use this effective treatment. We also focus on patient care to lower the risk of fractures.
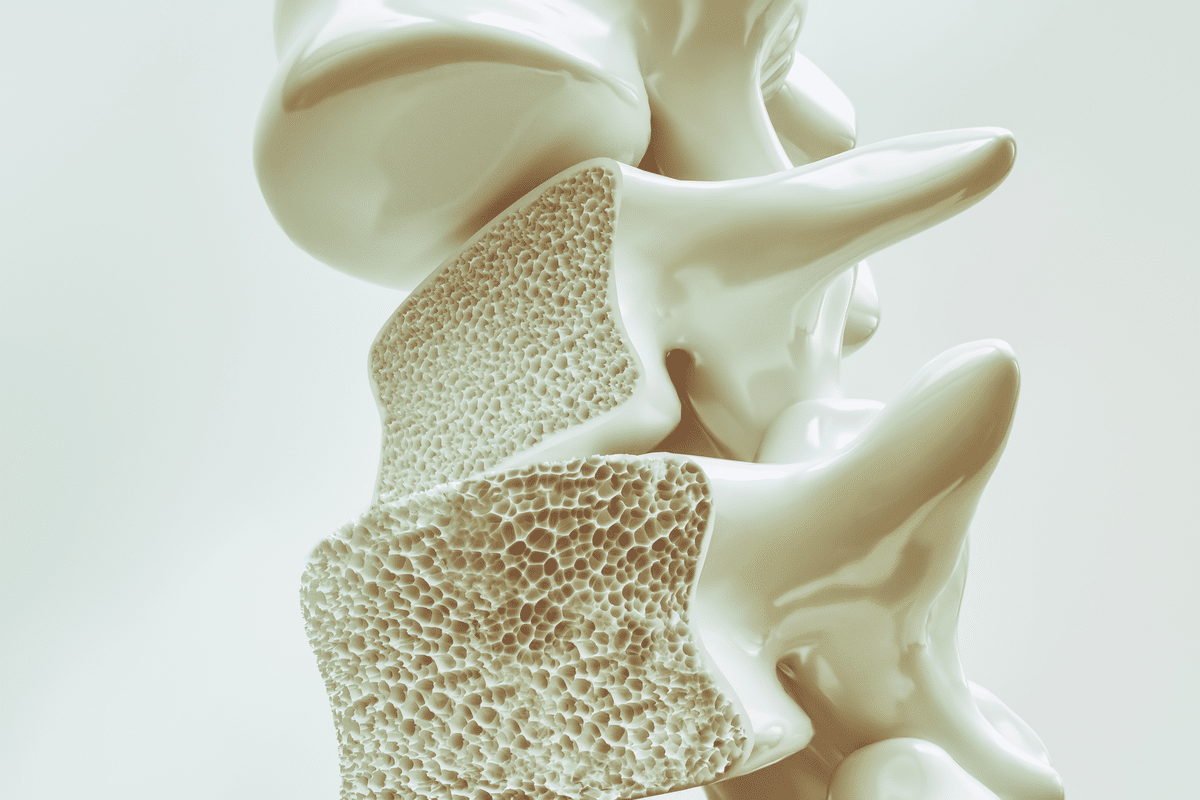
Knowing how bones work is key to fighting osteoporosis and osteopenia. These conditions are linked to how bones are made and how dense they are. This is important for keeping bones strong.
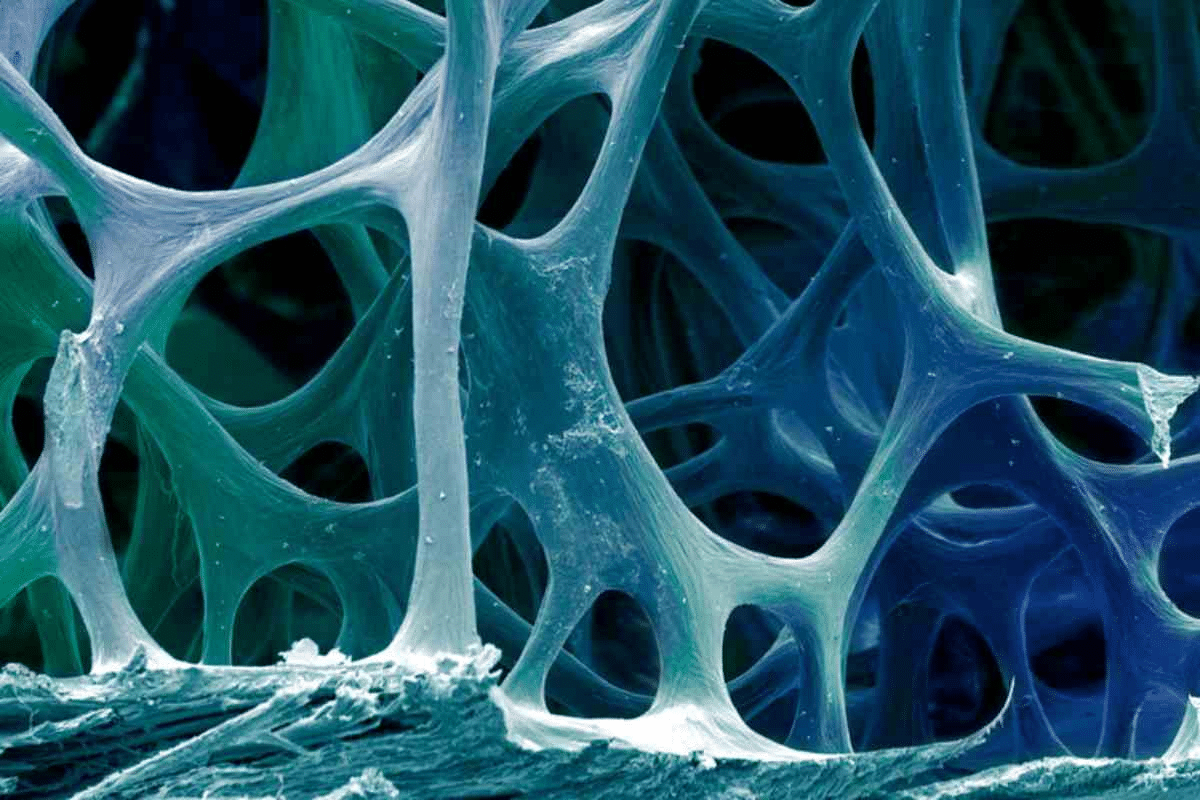
Bones are always being remade through a balance of two types of cells. Osteoclasts break down bone, while osteoblasts build it up. This cycle is vital for fixing small cracks and adjusting to stress.
Bone density is how much minerals like calcium are in your bones. It’s a big factor in how strong your bones are.
Bisphosphonates help by stopping osteoclasts from breaking down bone. This slows down bone loss and keeps bone density up. Over time, bones can get denser, which is good.
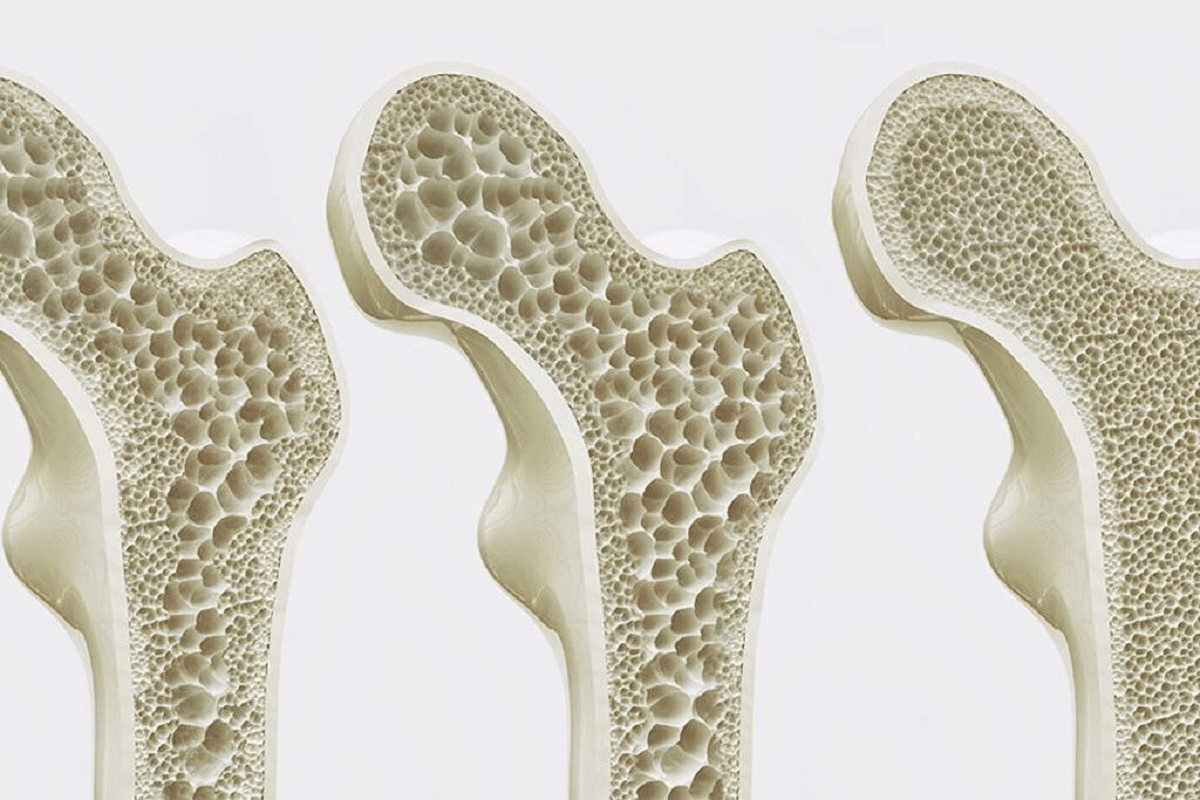
Osteoporosis and osteopenia happen when bone breakdown outpaces building. This leads to a loss of bone mass and density. Osteoporosis makes bones so weak they can break easily.
Osteopenia is when bones are less dense than normal but not as weak as in osteoporosis. It’s seen as a step before osteoporosis.
These conditions are caused by a mix of genetics, hormones, and environment. Knowing this helps doctors diagnose and treat early. Early treatment can lower the chance of fractures and keep bones healthy.
It takes time for bones to renew, but treatment like bisphosphonates can show results in five years. This shows why long-term care and checks are important for people with these conditions.
Bisphosphonates are important for keeping bones healthy. They are used to treat osteoporosis and other bone diseases. These conditions are caused by bone loss.
Definition and Classification of Bisphosphonates
Bisphosphonates are man-made compounds similar to something found naturally in our bodies. They stick well to bone minerals, like hydroxyapatite, which is a big part of bones.
They are sorted into two groups based on their structure and strength. The first group includes etidronate and clodronate. The second and third groups are stronger and include alendronate, risedronate, ibandronate, and zoledronic acid.
Bisphosphonates mainly work by stopping osteoclasts from breaking down bones. Osteoclasts are cells that break down bones, which is important for bone health but can be bad if too much happens.
They bind to bone minerals and get taken in by osteoclasts. Inside these cells, they stop a key process needed for cell function. This leads to the death of these cells.
This action helps reduce bone loss, makes bones denser, and lowers the chance of fractures. It’s good for people with osteoporosis and other bone diseases.
It’s important for doctors to know when to use bisphosphonates. These medicines help with bone problems like osteoporosis and osteopenia.
The American College of Physicians suggests bisphosphonates for the first treatment of osteoporosis. Bisphosphonate treatment lowers the chance of hip and spine fractures.
Bisphosphonates stop bone loss by slowing down bone resorption. This helps increase bone density, which is key in fighting osteoporosis.
Osteopenia means bones are denser than osteoporosis but not normal. Doctors decide to treat it with bisphosphonates based on risk factors like age and family history.
This approach helps pick the right people for treatment. It makes sure the treatment works best.
Bisphosphonates are also used for Paget’s disease of bone and bone metastases from cancer.
This shows bisphosphonates are good for many bone issues. They are effective and versatile.
Bisphosphonates are key in treating osteoporosis. They come in oral and intravenous forms, each with its own use and side effects. This variety helps meet different patient needs.
Oral bisphosphonates are often used to treat osteoporosis. Alendronate, risedronate, and ibandronate are among them. They help lower the risk of fractures in people with osteoporosis.
But, these drugs are not well absorbed by the body. They can irritate the esophagus, causing heartburn and other issues. It’s important to follow the right way to take them to avoid these problems.
|
Oral Bisphosphonate |
Dosing Frequency |
Common Side Effects |
|---|---|---|
|
Alendronate |
Once weekly |
Esophageal irritation, abdominal pain |
|
Risedronate |
Once weekly or once monthly |
Gastrointestinal upset, musculoskeletal pain |
|
Ibandronate |
Once monthly (oral) or every 3 months (IV) |
Dyspepsia, diarrhea |
For those who can’t take oral bisphosphonates or need stronger treatment, intravenous bisphosphonates are an option. Zoledronic acid and pamidronate are given directly into the blood. This skips the stomach.
Zoledronic acid is known for its strong effect in preventing fractures. It’s given once a year. Pamidronate is used less often but helps with bone pain in some cases.
Intravenous bisphosphonates are mainly for severe osteoporosis or when other treatments fail. They can have serious side effects like kidney problems and jaw damage.
Choosing the right patients for bisphosphonate therapy is key. It’s all about looking at who’s most likely to benefit. This way, we get the best results and avoid unwanted side effects.
Figuring out who might break a bone is vital. The FRAX calculator helps predict this risk. Bone mineral density (BMD) testing is also important. It checks bone health at different spots, like the hip and spine.
Women going through menopause lose bone fast. It’s important to check their fracture risk and BMD. For women over 65 with low bone density, treatment plans must be tailored. This includes looking at family history, past fractures, and other health issues.
Bisphosphonates help many, including men and those with secondary osteoporosis. Men with hypogonadism or other bone loss causes might need treatment. Each person’s situation is unique, so a careful look at their health is needed.
Pre-treatment assessment is key in getting patients ready for bisphosphonate treatment. It helps reduce risks and improve results. This step involves a detailed check-up to make sure patients are well-prepared for therapy.
Healthcare providers must do lab tests and imaging before starting bisphosphonate therapy. These steps help find any issues and make sure the treatment fits the patient’s needs.
Laboratory tests may include:
Imaging studies like Dual-Energy X-ray Absorptiometry (DXA) scans are important. They check bone density and fracture risk.
It’s important to check vitamin D and calcium levels before starting bisphosphonate therapy. Patients with low levels might need supplements to get the best results.
Children and young people should have their vitamin D checked before their first bisphosphonate infusion. The goal is to keep levels above 50 nmol/l.
|
Nutrient |
Recommended Level |
Action for Deficiency |
|---|---|---|
|
Vitamin D |
>50 nmol/l |
Supplementation |
|
Calcium |
Adequate dietary intake |
Dietary counseling or supplementation |
By focusing on these important factors, doctors can ensure bisphosphonate therapy is safe and effective.
To get the most out of oral bisphosphonates, patients need to know how to take them right. These medicines are key in fighting osteoporosis. How well they work depends on how they are taken.
Oral bisphosphonates should be taken first thing in the morning on an empty stomach. Make sure to drink a full 8 oz glass of water. This helps the medicine work better and keeps your throat safe.
Proper administration technique is vital to prevent complications and ensure the medication’s efficacy.
To help patients stick to their oral bisphosphonate treatment, several strategies can be used:
|
Administration Tips |
Benefits |
|---|---|
|
Take on an empty stomach |
Enhances absorption |
|
Stay upright for 30 minutes |
Reduces esophageal irritation |
|
Use a full glass of water |
Helps the tablet move into the stomach |
By sticking to these tips and strategies, doctors can help patients get the most out of their oral bisphosphonate treatment. This way, they can enjoy the benefits while avoiding unwanted side effects.
Administering intravenous bisphosphonates needs careful thought. This method is good for those who can’t take oral bisphosphonates or need a direct way to get the medicine.
Following specific guidelines is key when preparing intravenous bisphosphonates. Zoledronic acid, a common choice, is given as a single dose yearly. The infusion should last at least 15 to 20 minutes.
To prepare zoledronic acid, mix it with a solution like 100 mL of normal saline or 5% dextrose. The exact steps may change based on the product and patient needs.
After the infusion, watch for any bad reactions, like flu-like symptoms. These are common with these medicines. It’s also important to check kidney function, as bisphosphonates can impact it.
|
Monitoring Parameter |
Pre-Infusion |
Post-Infusion |
|---|---|---|
|
Renal Function |
Assess serum creatinine |
Monitor for changes |
|
Calcium Levels |
Check for hypocalcemia |
Monitor for changes |
|
Patient Symptoms |
Assess for flu-like symptoms |
Manage symptoms as needed |
Good post-infusion care includes telling patients about possible side effects and how to handle them. This might mean suggesting over-the-counter meds for flu-like symptoms. It’s also important to remind them about follow-up visits to check on their bone health and kidney function.
It’s important to check how well bisphosphonate therapy is working. These drugs help a lot with osteoporosis by lowering the chance of fractures. But, we need to watch them closely to make sure they’re doing their job.
Checking bone density regularly is key when using bisphosphonates. How often you get tested depends on your health. Usually, it’s every 1 to 2 years. This helps doctors see if your bones are getting stronger and adjust your treatment if needed.
Table: Recommended Schedule for Bone Density Testing
|
Patient Group |
Initial BMD Test |
Follow-Up BMD Test |
|---|---|---|
|
Postmenopausal Women |
At diagnosis |
1-2 years after starting bisphosphonate therapy |
|
Men with Osteoporosis |
At diagnosis |
1-2 years after starting bisphosphonate therapy |
|
Patients with Secondary Osteoporosis |
At diagnosis |
1 year after starting bisphosphonate therapy |
Biochemical markers also help see if bisphosphonates are working. Tests like serum C-telopeptide (CTX) and N-terminal propeptide of type 1 collagen (P1NP) show how fast bones are changing. If these markers go down, it means treatment is working well.
The main goal of bisphosphonates is to lower the risk of fractures. Doctors look at your bone density, your medical history, and use tools like the Fracture Risk Assessment Tool (FRAX) to check this. This helps them see if your risk is going down.
By using all these methods, doctors can really check if bisphosphonates are helping. They can then make the best choices for your treatment.
Bisphosphonate therapy is effective but needs careful side effect management for patient safety. Like any medicine, bisphosphonates can cause various reactions, from mild to severe.
The most common side effects include dyspepsia, nausea, and esophagitis in the stomach. To lessen these, patients should:
Other common side effects are musculoskeletal pain and flu-like symptoms. These are usually mild and often go away on their own.
Though rare, bisphosphonates can lead to serious issues like osteonecrosis of the jaw (ONJ) and atypical femoral fractures (AFF). ONJ is when jaw bone is exposed for over 8 weeks. Risk factors include:
Atypical femoral fractures happen with little or no trauma. Patients on long-term therapy should watch for signs of these issues.
Long-term safety of bisphosphonates is key. These drugs can work for years but may have long-term side effects. Patients on long-term therapy should:
A drug holiday might be suggested after 3-5 years, based on individual risk and response.
Bisphosphonate therapy is key in managing osteoporosis. It helps patients at risk of fractures. Knowing about bone health and osteoporosis helps doctors use bisphosphonates well.
Studies show bisphosphonates lower fracture risk in osteoporosis patients. They stop bone loss by slowing down bone resorption. This keeps bones strong and reduces fracture chances.
Managing osteoporosis well means choosing the right patients and monitoring them closely. Following guidelines helps doctors use bisphosphonates safely and effectively.
In short, bisphosphonates are essential for treating osteoporosis and osteopenia. Understanding their benefits and risks helps doctors give the best care. This way, they can help patients avoid osteoporotic fractures.
Bisphosphonate therapy helps manage osteoporosis and osteopenia. It works by stopping bone breakdown and improving bone health.
Bisphosphonates stop bone breakdown. This helps keep bones strong and healthy.
There are many bisphosphonate medications. Oral options include alendronate, risedronate, and ibandronate. Intravenous choices are zoledronic acid and pamidronate.
Take oral bisphosphonates with a full glass of water. Stay upright for 30 minutes after to avoid side effects.
Side effects include stomach problems like esophagitis and dyspepsia. Musculoskeletal pain is also common.
Effectiveness is checked with bone density tests and biochemical markers. Fracture risk is also assessed.
Serious complications include osteonecrosis of the jaw (ONJ) and atypical fractures.
Therapy length varies based on individual needs and fracture risk. It should be reviewed regularly.
Yes, men with osteoporosis or osteopenia can use bisphosphonates. Treatment is tailored to each patient’s risk.
Postmenopausal women should have their fracture risk and bone density checked. Treatment is customized based on these factors.
Vitamin D and calcium levels are important before starting therapy. They help ensure treatment works well.
Intravenous bisphosphonates are given through a controlled infusion. Patients are watched for side effects and complications.
National Center for Biotechnology Information. Evidence-Based Medical Guidance. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK470248/
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!