Macular edema is a condition where fluid builds up in the macula. The macula is key for sharp vision. This buildup can blur your vision and make reading hard eyeball leaking fluid.
Diabetic retinopathy often leads to macular edema, mainly in diabetics. If not treated, it can cause permanent vision loss. But, catching it early and treating it right can save your vision.
We know how vital it is to tackle macular edema well. In this article, we’ll dive into its causes, symptoms, and treatments. We aim to help you keep your eyes healthy.
Key Takeaways
- Macular edema involves fluid accumulation in the macula, causing vision distortion.
- Diabetic retinopathy is a primary cause of macular edema.
- Early detection and treatment are key to avoiding permanent vision loss.
- Proper treatment can help preserve vision and eye health.
- Understanding the causes and symptoms is essential for effective management.
Understanding Macular Edema
It’s important to know about macular edema to fight vision loss. This condition happens when fluid builds up in the macula. The macula is key for sharp, central vision.
What Happens in the Retina
The retina is at the back of the eye. It turns light into signals for the brain, helping us see. When it gets swollen from fluid, vision gets worse.
The retina’s cells work together to capture light. In macular edema, fluid messes with this process. It causes vision to get distorted.
The Role of the Macula in Vision
The macula is at the retina’s center. It’s vital for seeing details, colors, and things right in front of us. When it’s affected by edema, vision gets blurry.
This can make everyday tasks hard, like reading or driving. Keeping the macula healthy is key for clear vision. Any problem, like retinal swelling causes by fluid, can mess with our sight.
Fluid Balance Mechanisms
The eye has special ways to keep fluid in balance. It uses the blood-retinal barrier and fluid drainage. But in macular edema, these fail, causing fluid to build up.
Knowing how these work is vital for treating macular edema. By fixing the fluid buildup, doctors can help patients see better again.
Recognizing the Signs and Symptoms
The signs of macular edema can be hard to spot at first. But catching them early is key to treating them well. Macular edema can make your vision blurry, but these changes can get worse if not treated.
Visual Disturbances
Blurred vision is a big sign of macular edema. This blurriness can happen in one or both eyes and can change during the day. Other signs include:
- Distorted vision, where straight lines appear wavy or bent
- Difficulty reading or performing other daily tasks that require clear vision
- Changes in color vision, making colors appear less vibrant
These symptoms happen because fluid builds up in the macula. This makes it swell and causes vision problems.
Progression of Symptoms
If macular edema isn’t treated, symptoms can get worse. The changes can include:
- Increased blurriness or distortion
- Significant difficulty with daily activities due to vision impairment
- Potential development of blind spots or other severe visual impairments
It’s important to watch for any changes in your vision. If symptoms don’t go away or get worse, see a doctor.
When to Seek Medical Attention
Getting macular edema treated early is key to saving your vision. We suggest seeing a doctor if you notice:
- Sudden changes in vision
- Persistent blurred vision or distortion
- Difficulty with daily tasks due to vision problems
Seeing an eye care professional quickly can help find the problem and start treatment.
Common Causes of Eyeball Leaking Fluid
Knowing why macular edema happens is key to treating it. This condition is when fluid builds up in the macula. The macula is the part of the retina that helps us see clearly. It can be caused by diabetes, age-related diseases, blocked blood vessels, and surgery problems.
Diabetic Macular Edema (DME)
Diabetic macular edema is a big problem for people with diabetes. High blood sugar can harm the retina’s blood vessels. This leads to fluid buildup in the macula. It’s a top reason for vision loss in diabetics. Keeping diabetes under control is important to avoid DME.
Age-Related Macular Degeneration (AMD)
AMD is another major cause of macular edema. It happens when the macula wears out with age. There are two types: dry and wet. Wet AMD is more likely to cause fluid buildup because of new, leaky blood vessels under the macula.
Retinal Vein Occlusion
Retinal vein occlusion happens when veins in the retina get blocked. This blockage can cause fluid and blood to leak into the retina. It’s a big risk factor for macular edema, mainly in older people.
Post-Surgical Complications
Eye surgery, like cataract surgery, can also lead to macular edema. This is often due to inflammation and chemicals that make blood vessels leak. It’s important to watch for macular edema after surgery to treat it early.
Understanding these causes helps us diagnose and manage macular edema better. This can help save vision for those affected.
Secondary Causes and Risk Factors
It’s important to know the secondary causes and risk factors for macular edema. Primary causes like diabetic macular edema and age-related macular degeneration are well-known. But, secondary factors can also greatly affect the condition’s development and growth.
Hypertension and Cardiovascular Disease
Hypertension and cardiovascular disease are big risks for macular edema. High blood pressure can harm the retina’s blood vessels, causing fluid leakage and edema. We’ll talk about why controlling blood pressure is key to preventing macular edema.
- Hypertension can damage the retinal vessels.
- Cardiovascular disease increases the risk of macular edema.
- Managing blood pressure is key to preventing complications.
Inflammatory Eye Conditions
Certain inflammatory eye conditions can lead to macular edema. For example, uveitis causes eye inflammation, leading to fluid buildup in the macula. We’ll look at how treating these conditions can help manage macular edema.
Medication-Induced Macular Edema
Some medications can cause macular edema as a side effect. For example, certain corticosteroids and other medications can cause fluid retention in the retina. We’ll discuss why it’s important to watch patients on long-term medications closely.
- Corticosteroids can cause fluid retention.
- Other medications may have similar side effects.
- Regular eye exams are key for patients on long-term medications.
Genetic Predispositions
Genetic predispositions also play a role in macular edema. People with a family history of retinal diseases are more likely to get macular edema. We’ll look at the latest research on genetics and how it affects prevention and treatment.
Diagnostic Procedures for Macular Edema
To find out if someone has macular edema, doctors use several tests. These tests help figure out how bad it is and what treatment to use.
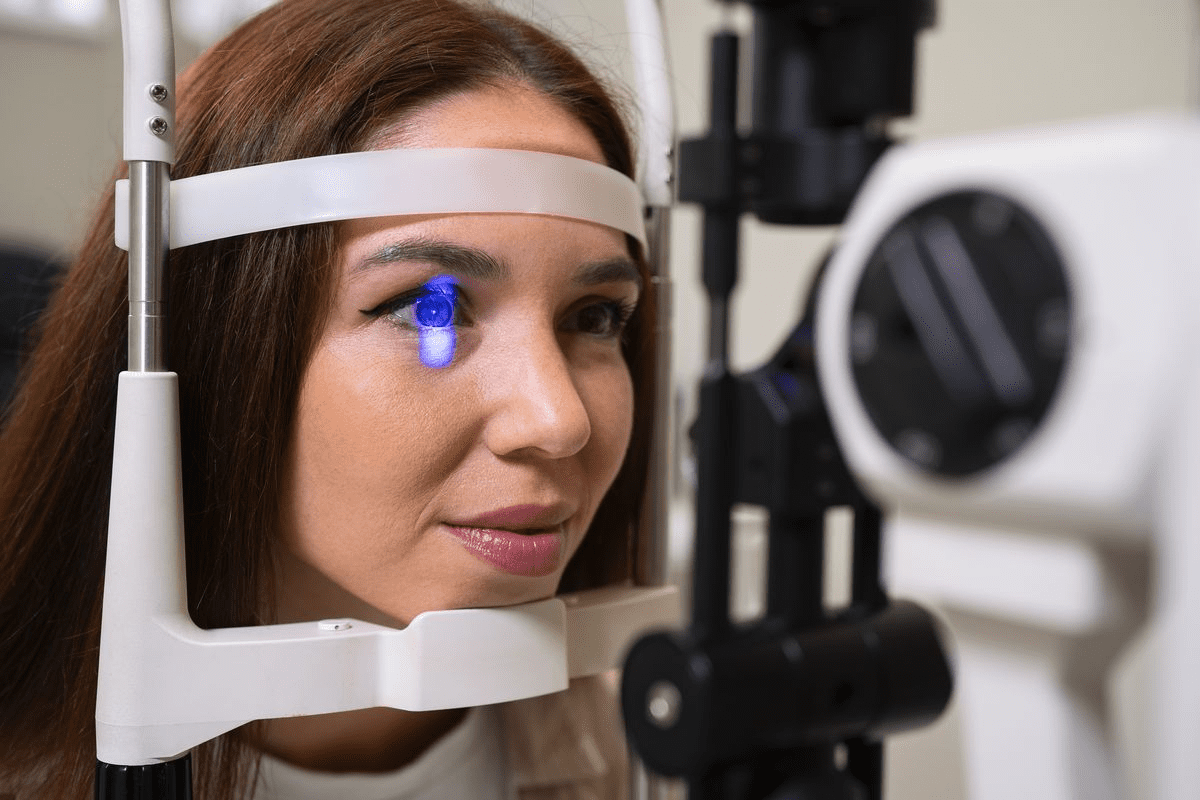
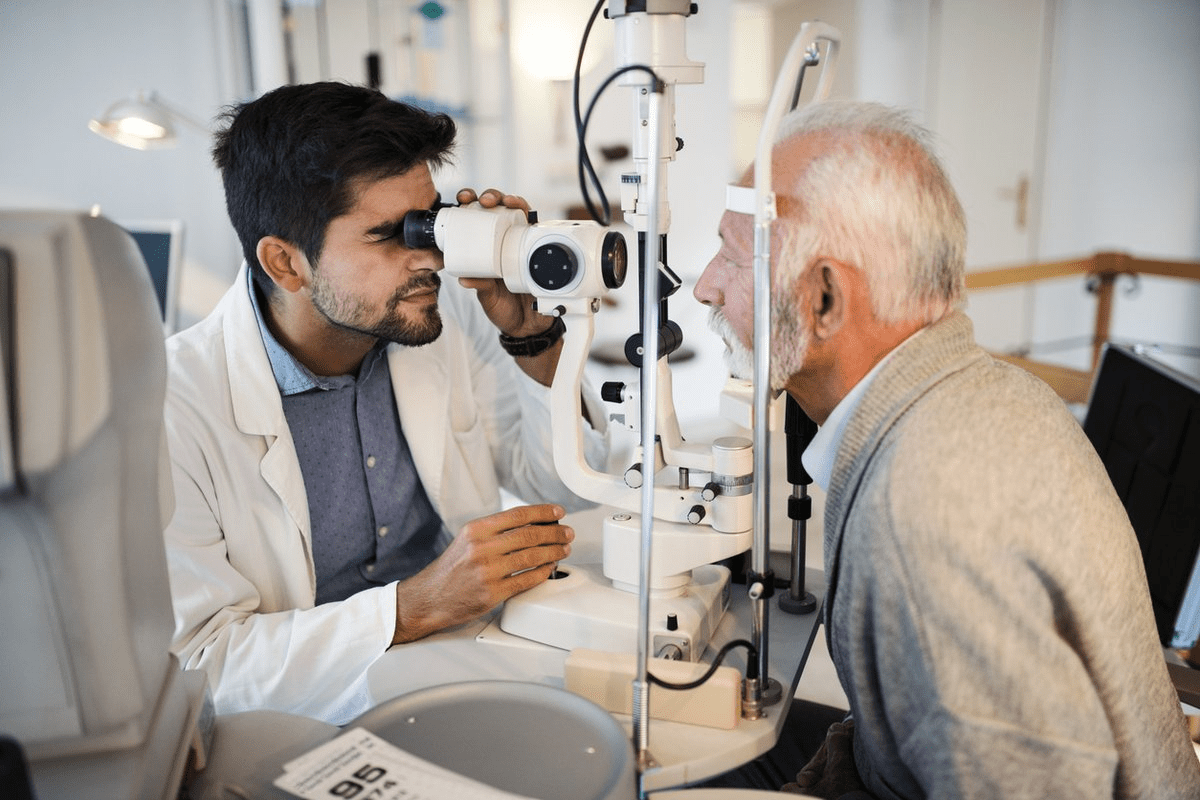
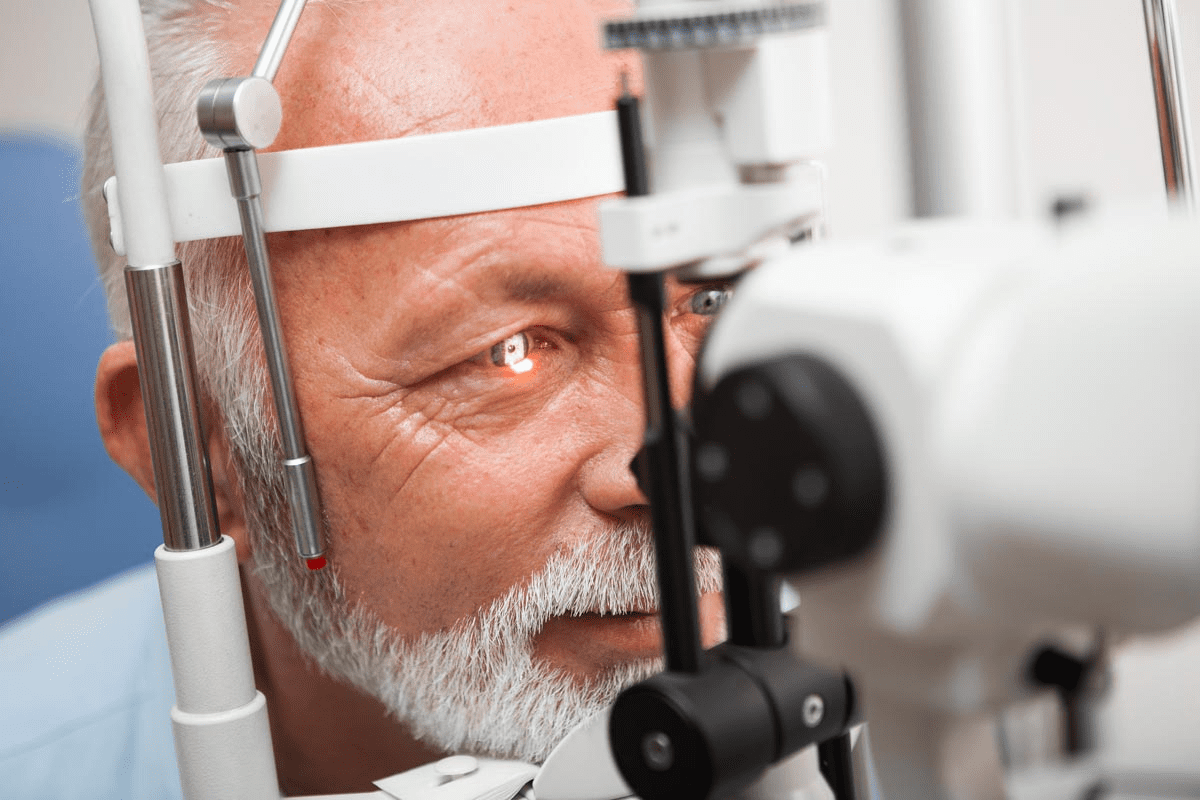
Comprehensive Eye Examination
A complete eye check is the first step to find macular edema. It includes looking at the patient’s health history, checking how well they can see, and a detailed look at the retina. Spotting it early can really help treatment work better.
Optical Coherence Tomography (OCT)
OCT is a test that takes pictures of the retina without hurting it. It shows how thick the retina is and if there’s fluid, which is a sign of macular edema. OCT helps doctors see how the retina changes over time, helping them decide on treatment.
A leading ophthalmology journal says, “OCT has changed how we diagnose and manage macular edema. It gives us detailed pictures of the retina.”
“The use of OCT is key in diagnosing and tracking macular edema. It lets us measure retinal thickness and spot small changes.”
Fluorescein Angiography
Fluorescein angiography is another important test for macular edema. It involves putting a dye into the blood to see the blood vessels in the retina. It can show if there’s leakage, which means macular edema. This test helps doctors see if the retina’s blood vessels are working right.
Additional Testing Methods
There are more tests used to check for macular edema. These include fundus photography, which takes detailed retina pictures, and microperimetry, which checks how sensitive the retina is. These tests help doctors understand the condition better and how it affects vision.
By using these tests, doctors can accurately diagnose macular edema. They can then figure out how severe it is and plan the best treatment for each patient.
Medical Treatments and Interventions
Several medical treatments can help with macular edema. These treatments aim to reduce fluid buildup and improve vision. The right treatment depends on the cause, how severe it is, and the patient’s health.
Anti-VEGF Injections
Anti-VEGF injections are key in treating macular edema, mainly for diabetic retinopathy and age-related macular degeneration. They stop new blood vessels from growing and leaking. This helps reduce fluid in the macula.
Benefits: These injections can greatly improve vision. Many patients see quick improvements in just a few weeks.
- Patients usually need injections every month to keep seeing improvements.
- While rare, risks include eye infections and retinal detachment.
Corticosteroid Treatments
Corticosteroids are another option for macular edema, often for those not helped by anti-VEGF or with uveitis. They can be given as injections or implants for long-lasting effects.
Benefits: Corticosteroids help reduce inflammation and fluid. They’re good for those with ongoing or chronic macular edema.
- Side effects can include cataracts and high eye pressure.
- It’s important to watch for these side effects closely.
Laser Photocoagulation
Laser photocoagulation uses a laser to make small burns in the retina. It aims to seal leaking blood vessels and lessen edema. It’s often used with other treatments.
Benefits: It can help stop fluid leakage and prevent vision loss.
- It might not work for all types of macular edema.
- There’s a risk of damaging nearby retinal tissue.
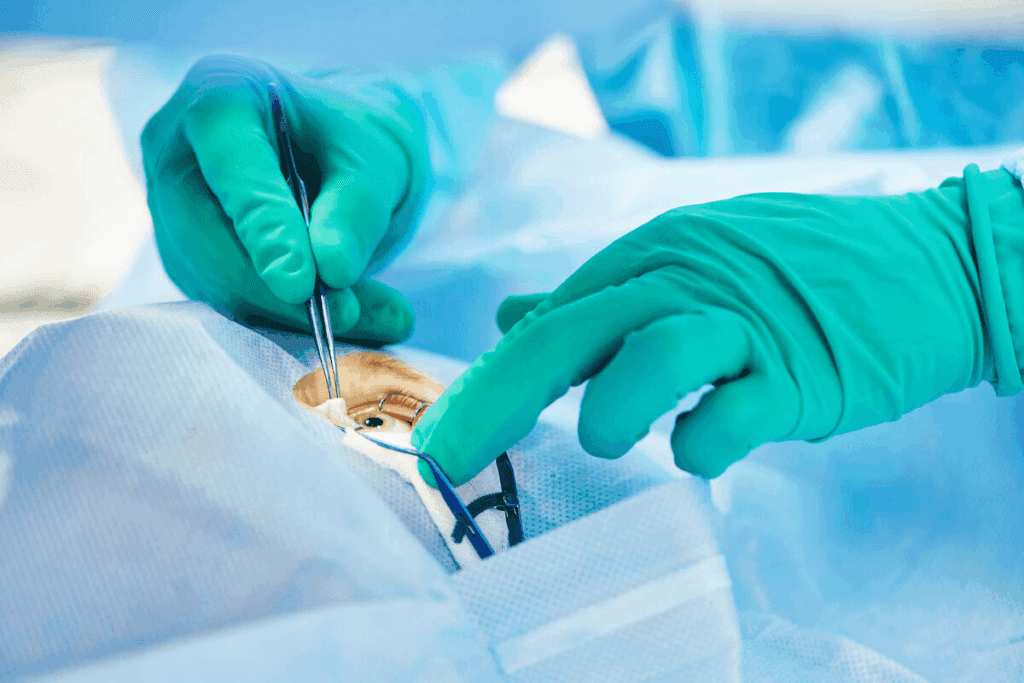
Vitrectomy Surgery
Vitrectomy surgery removes the vitreous gel from the eye. It’s often for macular edema caused by vitreomacular traction or other issues. This surgery can relieve traction on the retina and reduce edema.
Benefits: Vitrectomy can improve vision for certain types of macular edema.
- Like any surgery, there are risks such as infection, retinal detachment, and cataracts.
- Choosing the right patients is key for success.
In conclusion, treating macular edema requires various medical approaches. Each treatment is chosen based on the patient’s specific needs. Knowing the benefits and risks of these treatments helps make informed decisions about care.
Managing Underlying Conditions
Managing health conditions is key to preventing and treating macular edema. We’ll look at how controlling diabetes, managing high blood pressure, and treating inflammation can lower macular edema risk.
Diabetes Control and Management
Diabetes is a big risk for macular edema, like diabetic macular edema (DME). Keeping blood sugar in check is vital to stop diabetic retinopathy and lower macular edema risk. This means making healthy lifestyle choices and sticking to your medication.
It’s also important to regularly check your blood sugar and HbA1c levels. This helps see if your diabetes management is working well.
Hypertension Treatment
Hypertension can also lead to macular edema. Keeping blood pressure under control through diet, exercise, and medication is key. It’s important to check your blood pressure often and adjust your treatment as needed.
Addressing Inflammatory Disorders
Inflammatory disorders, like uveitis, can also raise macular edema risk. Treating inflammation quickly with anti-inflammatory drugs can help. Sometimes, corticosteroids are used to manage inflammation and prevent macular edema.
By effectively managing these conditions, people can greatly lower their risk of macular edema. We stress the need for a complete health management plan. Regular visits to healthcare providers are essential to monitor and adjust treatments as needed.
Lifestyle Modifications and Home Care
Making lifestyle changes and using home care strategies is key to managing macular edema. Healthy habits and smart choices can greatly impact your condition. This can also improve your life quality.
Dietary Considerations
Eating a balanced diet is essential for eye health. Foods rich in antioxidants, like leafy greens and berries, protect your eyes. Omega-3 fatty acids in fish like salmon are also good. Try to avoid processed foods and sugars.
- Incorporate leafy greens like spinach and kale into your diet.
- Enjoy berries and nuts as healthy snack options.
- Consume fish rich in omega-3 fatty acids at least twice a week.
Drinking plenty of water is also important. It helps keep your eyes healthy.
Exercise and Physical Activity
Regular exercise is good for those with macular edema. It improves circulation and overall health. This can lower the risk of complications. Walking, swimming, and cycling are great choices.
Benefits of Regular Exercise:
- Improved cardiovascular health.
- Enhanced circulation, which can benefit eye health.
- Better management of related conditions like diabetes and hypertension.
Smoking Cessation
Smoking increases the risk of eye problems, including macular edema. Quitting can greatly reduce these risks and improve your health. There are many resources to help you stop smoking, like counseling and nicotine replacement therapy.
“Quitting smoking is one of the most important steps you can take to protect your eye health and overall well-being.”
Vision Aids and Adaptations
Vision aids and adaptations can greatly help those with macular edema. Tools like magnifying glasses and adaptive technology can make a big difference. They improve daily life.
Seeing a low vision specialist can help find the right vision aids and adaptations for you.
Potential Complications of Untreated Macular Edema
Not treating macular edema can lead to severe vision problems. It can also affect your quality of life. Untreated, macular edema can cause permanent damage to your vision.
Permanent Vision Loss
Permanent vision loss is a major risk if macular edema is not treated. Fluid buildup in the macula can damage photoreceptors. This damage can make it hard to read, drive, and recognize faces.
Such vision loss can make you less independent. It can affect your daily activities and overall well-being.
Impact on Quality of Life
Untreated macular edema can greatly reduce your quality of life. Losing central vision makes everyday tasks harder. This can lead to less mobility and more dependency on others.
It can cause feelings of frustration, isolation, and a lower sense of well-being. This is why treating macular edema is so important.
Psychological Effects
The psychological effects of untreated macular edema are significant. Losing vision and facing daily challenges can cause psychological distress. This includes anxiety and depression.
It’s vital for those with macular edema to get both medical and emotional support. This helps them cope with the condition’s psychological impact.
We stress the need for early treatment to avoid these complications. Treating macular edema promptly can prevent permanent vision loss. It helps maintain your quality of life.
Emerging Treatments and Research
New treatments for macular edema are coming, thanks to advanced therapies and tech. Scientists are always looking for ways to help patients live better lives.
Novel drug therapies are a big hope. These drugs aim to fix the problems that cause macular edema. They might be safer and work better than what we have now.
Novel Drug Therapies
New drugs are being made to fight macular edema. For example, some target VEGF, which helps reduce swelling and improve sight. Others aim to stop inflammation and damage caused by free radicals.
Clinical trials are testing these drugs. Early signs are good, showing they might help more people than current treatments.
Sustained-Release Devices
Sustained-release devices are another big step forward. They release medicine slowly, so you don’t need to get injections as often. This makes treatment easier for patients.
These devices are implanted in the eye. They slowly release medicine, keeping levels steady for months. This method is safer and more comfortable for patients.
Regenerative Medicine Approaches
Regenerative medicine is also being explored. It uses stem cells or other materials to fix damaged eye tissue.
This field is very promising but is just starting. Scientists are working hard to make it safe and effective. They face many challenges, but the hope is high.
As research keeps going, we’ll see even more new treatments for macular edema. These could greatly improve how patients feel and live.
Conclusion
Macular edema is a big reason for vision loss, but it can be managed. We’ve looked at the causes, like diabetic macular edema and age-related macular degeneration. We also talked about symptoms and how doctors diagnose it.
Managing macular edema well means using medicine and changing your lifestyle. This includes eating right and quitting smoking. Getting help quickly is key to keeping your vision.
Knowing about macular edema and getting help fast can help keep your eyes healthy. It’s important to take care of your eyes and manage any health issues. This way, you can fight macular edema and keep your vision sharp.
FAQ
What is macular edema?
Macular edema is when fluid builds up in the macula. This part of the retina handles central vision. It can cause vision problems.
What are the symptoms of macular edema?
Symptoms include blurred vision and distorted lines. These can worsen if not treated.
What causes macular edema?
It can be caused by diabetic retinopathy, age-related macular degeneration, and more. Even surgery can lead to it.
How is macular edema diagnosed?
Doctors use eye exams, Optical Coherence Tomography (OCT), and fluorescein angiography. These tests help diagnose it.
What are the treatment options for macular edema?
Treatments include anti-VEGF injections and laser photocoagulation. Vitrectomy surgery is also an option.
Can macular edema be prevented?
Some risk factors can’t be avoided. But managing diabetes and hypertension can help prevent it.
What is the impact of untreated macular edema?
Without treatment, it can cause permanent vision loss. It also affects quality of life and mental health.
Are there any lifestyle changes that can help manage macular edema?
Yes, eating well, exercising, and quitting smoking help. Using vision aids is also beneficial.
What is diabetic macular edema?
It’s a diabetes complication. Fluid builds up in the macula, causing vision loss.
How does hypertension affect macular edema?
High blood pressure can damage retina blood vessels. This increases macular edema risk.
What are the emerging treatments for macular edema?
New treatments include drugs and devices. Regenerative medicine is also being explored.
What is the role of genetic predispositions in macular edema?
Genetics can play a part, mainly in those with a family history. It increases risk.
Can inflammatory eye conditions cause macular edema?
Yes, they can. Inflammation leads to fluid buildup in the macula.
How does age-related macular degeneration relate to macular edema?
It raises the risk, mainly in older adults. Age-related macular degeneration can lead to it.
What is the significance of fluid balance in the retina?
Fluid balance is key. Too much fluid can cause macular edema and vision issues.
Can certain medications cause macular edema?
Yes, some medications can cause it. It’s important to watch for side effects.
References
National Center for Biotechnology Information. Evidence-Based Medical Guidance. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK576396/