Idiopathic intracranial hypertension (IIH) is a condition where the skull’s pressure goes up without a known reason. It mainly hits obese women who are of childbearing age.
Knowing the basics of IIH is key to understanding how it’s diagnosed. This condition happens when there’s too much cerebrospinal fluid around the brain. This leads to higher pressure.
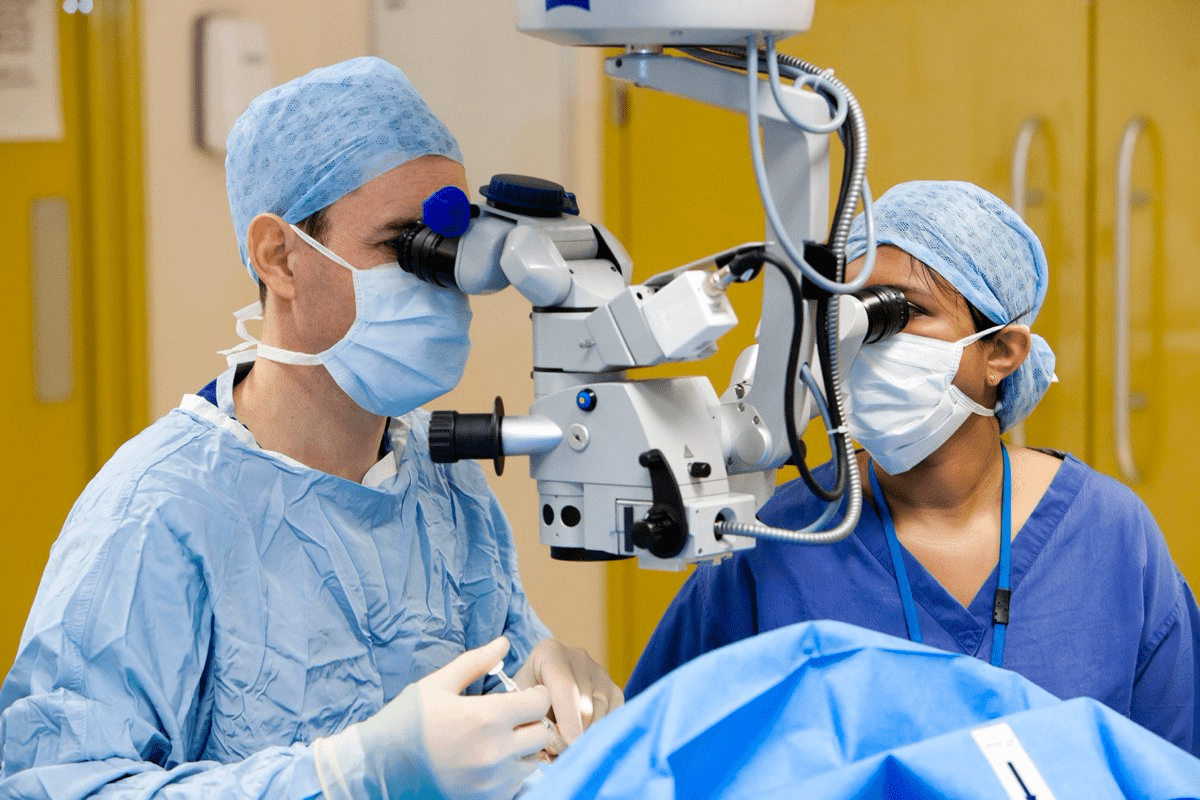
At Liv Hospital, we focus on the patient and use the latest medical standards to spot IIH. We use a mix of clinical checks, special brain scans, and lumbar punctures to see if the pressure is high.
Learn the intracranial hypertension diagnostic criteria. This essential guide covers the key signs for a definitive diagnosis.
Key Takeaways
- IIH is a condition of unknown cause characterized by increased intracranial pressure.
- It mainly affects obese women of childbearing age.
- Diagnosis involves clinical evaluation, neuroimaging, and lumbar puncture findings.
- Liv Hospital follows a patient-centered approach for accurate diagnosis.
- Early diagnosis is key to protect vision and manage the condition well.
Understanding Idiopathic Intracranial Hypertension
Idiopathic intracranial hypertension (IIH) is a complex condition. It happens when there’s high pressure in the skull without a known cause. This condition, also known as pseudotumor cerebri, can cause serious problems if not treated right.
IIH happens when too much cerebrospinal fluid (CSF) builds up in the skull. This puts pressure on the brain and optic nerve. Doctors check for IIH by looking at the CSF pressure during a lumbar puncture. If it’s over 25 cm CSF, they know it’s there.
Definition and Pathophysiology
The buildup of CSF leads to high pressure in the skull in IIH. This pressure can cause headaches and vision problems. Knowing how CSF builds up is key to treating IIH well.
The exact reason for IIH is not known. But it’s thought to be linked to how the body handles CSF. Things that mess with this balance can cause IIH.
Prevalence and Demographics
IIH mostly affects women of childbearing age, and those who are obese. It’s less common in men and non-obese people. This makes it a big health concern for certain groups.
Research shows IIH is becoming more common. This is likely because more people are becoming obese. Knowing who is at risk helps doctors give better care.
Risk Factors for Idiopathic Intracranial Hypertension
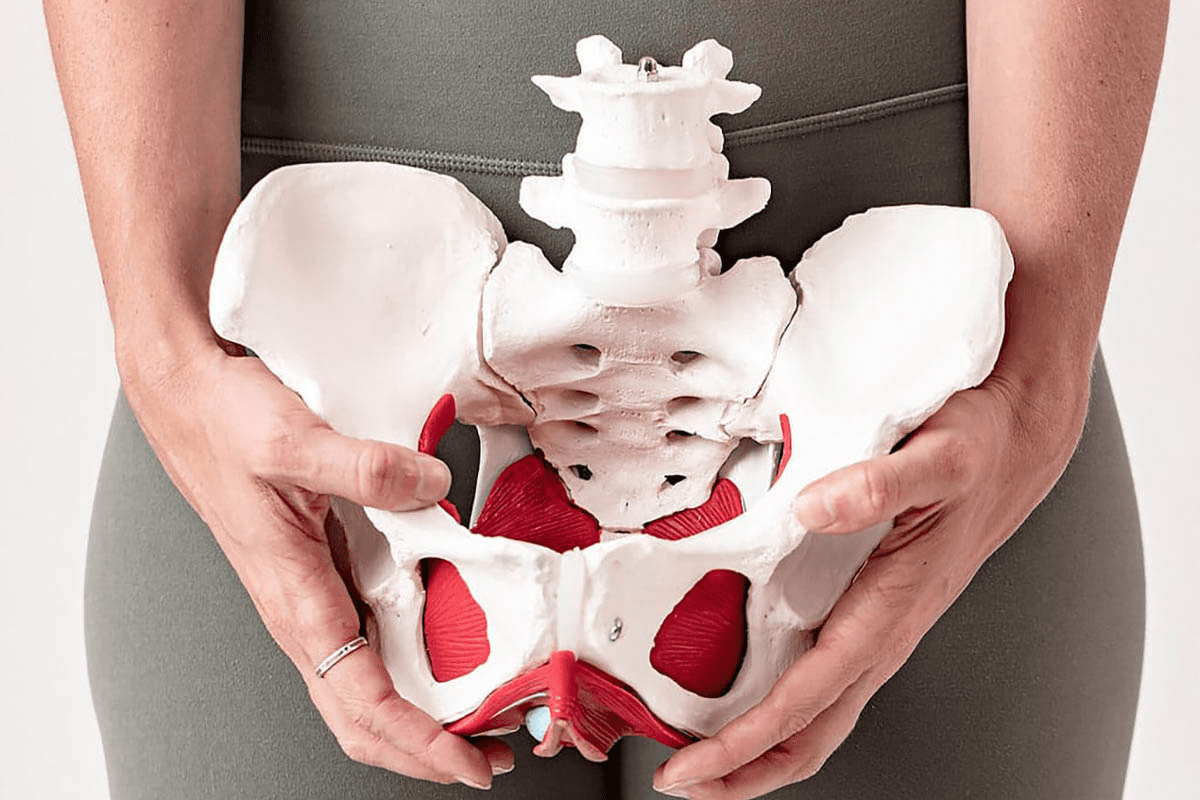
Knowing the risk factors for idiopathic intracranial hypertension (IIH) is key to early diagnosis and treatment. We will look at the main factors that lead to IIH. These include obesity, hormonal changes, and other health conditions.
Obesity and Weight-Related Factors
Obesity is a big risk for IIH, mainly in young women. Research shows that IIH is 20 times more common in overweight young women than in those at a normal weight. This shows that weight issues play a big part in IIH.
The exact ways obesity leads to IIH are not fully known. But, it’s thought that increased pressure in the brain might be due to several factors. These include higher venous pressure, hormonal changes, and metabolic issues linked to obesity.
Risk Factor | Description | Association with IIH |
Obesity | Excess body weight, mainly in young women | Strongly linked to higher IIH risk |
Hormonal Influences | Hormonal level changes, mainly in women of childbearing age | May trigger IIH symptoms |
Associated Medical Conditions | Other health issues like sleep apnea, polycystic ovary syndrome (PCOS) | Can help cause or worsen IIH |
Hormonal Influences
Hormonal changes are also a risk factor for IIH, mainly in women. Hormonal shifts, like those during menstruation, pregnancy, or with hormonal birth control, might lead to IIH symptoms.
Associated Medical Conditions
Some medical conditions raise the risk of IIH. These include sleep apnea, polycystic ovary syndrome (PCOS), and other issues that can cause hormonal or metabolic problems.
Knowing these risk factors helps spot people at higher risk of IIH. It also guides how to diagnose and treat the condition. Key signs include papilledema or cranial nerve problems, which are key for diagnosing IIH.
Clinical Presentation of IIH
IIH shows a range of symptoms like headaches, visual issues, and other signs. These symptoms can really affect a person’s life and lead to seeing a doctor.
Headache Characteristics
Headaches are a big sign of IIH, happening in most people. These headaches are often daily, very severe, and may make you feel sick. The type of headache can vary, but it usually gets worse when you do things that raise your chest pressure, like coughing.
Visual Disturbances
Visual problems are also a big part of IIH. People might see things get blurry or dark for a few seconds, called transient visual obscurations. This can happen when you change how you’re sitting or standing. Long-term vision loss can also happen because of swelling in the optic nerve, which is a key sign of IIH.
Other Common Symptoms
People with IIH might also have other symptoms. Hearing noises in your head, called tinnitus, is common. It might sound like your heartbeat. You might also feel sick to your stomach and throw up, often when you have a headache. These symptoms, while not specific, help doctors understand what’s going on and how to help you.
Knowing how IIH presents is key to getting the right treatment. Doctors can spot the symptoms and start the right treatment early. This helps improve how patients feel and live with IIH.
Initial Clinical Evaluation
To diagnose IIH, a detailed initial evaluation is needed. This includes a thorough medical history and physical exam. It’s key to find IIH signs and rule out other pressure causes.
Medical History Assessment
The medical history assessment is the first step in diagnosing IIH. We start by asking about symptoms like headaches and vision problems. We also look into risk factors like obesity and hormonal changes.
Looking for pulsatile tinnitus and transient visual obscurations is important. This helps us understand if IIH might be present.
Physical Examination Findings
The physical examination is vital in diagnosing IIH. We do a detailed neurological check. This usually shows normal results, except for IIH signs.
Papilledema, or optic disc swelling, is a key IIH indicator. We also check for cranial nerve issues, like abducens nerve palsy.
We also do a general physical exam to check for obesity or other factors. By combining medical history and physical exam results, we can better understand the patient’s condition. This helps us decide on further tests like MRI or CT scans and spinal taps.
Neurological Examination in IIH Diagnosis
A detailed neurological exam is key to diagnosing IIH and understanding its effects. This exam helps us spot important signs that guide our diagnosis.
Normal Findings Expected in IIH
Often, IIH patients show normal results in their neurological exams. This can make diagnosis tricky. Yet, some parts of the exam are very important.
- Checking cognitive function, which is usually fine in IIH patients.
- Looking at motor and sensory functions, which are usually normal.
- Examining cranial nerves for any issues.
Cranial Nerve Abnormalities
Cranial nerve problems are a big deal in IIH diagnosis. The sixth cranial nerve, or abducens nerve, is often affected. This can cause diplopia (double vision).
Important things to note include:
- The presence of papilledema, a sign of increased intracranial pressure.
- Checking pupillary function, which is usually normal but needs checking.
- Doing visual field tests to spot any IIH-related defects.
It’s vital to treat IIH quickly to avoid losing vision. Neuroimaging is also key to rule out other conditions like tumors or brain problems.
Ophthalmologic Evaluation
To diagnose Idiopathic Intracranial Hypertension (IIH) accurately, a detailed ophthalmologic evaluation is necessary. This assessment is key for identifying the impact of IIH on the eyes. It helps in detecting and managing symptoms related to vision.
Detecting and Grading Papilledema
Papilledema, or the swelling of the optic disc, is a hallmark sign of IIH. Detecting and grading papilledema is essential for diagnosing and monitoring the condition. We use a detailed eye examination to assess the severity of papilledema. This helps in determining the appropriate treatment plan.
If you notice changes in your vision, it’s essential to consult with your eye doctor. Early detection and management can significantly impact the outcome.
Grade | Description | Clinical Implication |
0 | Normal | No papilledema detected |
1 | Mild swelling | Early signs of IIH |
2 | Moderate swelling | Established IIH, monitor closely |
3 | Severe swelling | High risk of vision loss, urgent treatment needed |
Visual Field Testing
Visual field testing is another critical component of the ophthalmologic evaluation in IIH. This test assesses the patient’s field of vision. It detects any defects or blind spots that may have developed due to the condition. Advanced visual field testing can help in monitoring the progression of IIH and the effectiveness of the treatment.
Optical Coherence Tomography (OCT)
Optical Coherence Tomography (OCT) is a non-invasive imaging test. It provides detailed pictures of the optic nerve and retina. In the context of IIH, OCT is used to detect changes in the optic nerve head and retinal thickness. This indicates the presence and severity of papilledema.
Advanced imaging techniques, including OCT, allow for non-invasive documentation and monitoring of optic nerve head changes. This enables healthcare providers to make informed decisions regarding the management of IIH.
Intracranial Hypertension Diagnostic Criteria
To diagnose IIH, doctors use specific criteria. These criteria help ensure accurate and consistent diagnosis of this complex condition.
Modified Dandy Criteria
The Modified Dandy Criteria are key for diagnosing IIH. They include:
- Symptoms of raised intracranial pressure (headache, nausea, vomiting, pulsatile tinnitus, visual disturbances)
- No localizing neurological signs except for sixth nerve palsy
- Normal neuroimaging (MRI or CT scan)
- Normal cerebrospinal fluid (CSF) composition
- Elevated CSF pressure (≥ 250 mmCSF in adults)
These criteria have helped standardize IIH diagnosis. They have also been updated to reflect new evidence and clinical findings.
Current Diagnostic Standards
Today, diagnosing IIH involves a detailed clinical evaluation. This includes a thorough medical history, physical exam, and diagnostic tests like neuroimaging and lumbar puncture. The presence of papilledema, visual field defects, and elevated CSF pressure supports the diagnosis.
Recent studies show that about 5-10 percent of IIH patients don’t have papilledema. This makes diagnosis more difficult in these cases.
IIH Without Papilledema (5-10% of Cases)
IIH without papilledema is a recognized variant, affecting 5-10% of patients. Diagnosing this form relies on other clinical features and diagnostic tests, including:
- Headache characteristics and other symptoms of raised intracranial pressure
- Visual field testing to detect subtle visual disturbances
- Optical coherence tomography (OCT) to assess the optic nerve head
- Lumbar puncture to measure CSF pressure
Idiopathic intracranial hypertension is rare, affecting about 1 in 100,000 people. It mainly affects women during their reproductive years. A high suspicion and thorough diagnostic evaluation are essential for identifying IIH, even in atypical cases.
Lumbar Puncture Procedure
A lumbar puncture is done to check the cerebrospinal fluid’s opening pressure. This is key for diagnosing Idiopathic Intracranial Hypertension (IIH). The procedure involves inserting a needle between two vertebrae in the lower back to reach the spinal canal.
Opening Pressure Measurement Technique
Measuring the opening pressure is a key part of the lumbar puncture. We use a manometer to check the cerebrospinal fluid’s pressure. The patient lies on their side, and we measure the pressure before draining any fluid.
Accurate measurement of the opening pressure is vital for diagnosing IIH. It’s important that the patient is relaxed and not straining or holding their breath. These actions can change the pressure reading.
Diagnostic Thresholds and the “Grey Zone” (250-300 mmCSF)
For diagnosing IIH, the lumbar puncture opening pressure must be over 25 cm CSF. But, there’s a “grey zone” between 250-300 mmCSF where diagnosis is tricky. We look at this range closely, considering the patient’s overall health.
When the opening pressure is close to the “grey zone,” we need to think about other signs and symptoms. This helps us confirm if the patient has IIH.
Cerebrospinal Fluid Analysis
During the lumbar puncture, we measure the opening pressure and collect cerebrospinal fluid for analysis. We check the cell count, protein levels, glucose levels, and more. This helps us rule out other conditions that might cause high pressure in the brain.
The cerebrospinal fluid analysis is a big part of diagnosing IIH. It helps us tell IIH apart from other causes of high pressure in the brain. It also helps us find any other conditions that might need special treatment.
Neuroimaging in IIH Diagnosis
Diagnosing Idiopathic Intracranial Hypertension (IIH) starts with neuroimaging. This step is key to rule out other issues like masses or brain blockages. It helps confirm IIH by checking for other causes of high pressure in the brain.
MRI Findings and Characteristics
Magnetic Resonance Imaging (MRI) is essential for IIH diagnosis. Even though MRI scans for IIH often show nothing out of the ordinary, they are vital. They help us check for other possible causes of high pressure.
Some MRI signs of IIH include:
- Normal or slit-like ventricles
- Empty sella turcica
- Distension of the optic nerve sheath
- Tortuosity of the optic nerve
MR Venography and Venous Sinus Assessment
MR Venography (MRV) helps us look at the brain’s venous sinuses. In IIH, MRV can spot problems like stenosis or thrombosis. These issues can add to the brain’s pressure. MRV is key to check for these problems and rule out other causes.
MRV Finding | Clinical Significance |
Normal Venous Sinuses | Supports IIH diagnosis if other causes are excluded |
Venous Sinus Stenosis | May be associated with IIH; further evaluation needed |
Cerebral Venous Sinus Thrombosis | Alternative diagnosis to IIH; requires anticoagulation therapy |
Excluding Alternative Diagnoses
Neuroimaging is key to rule out other conditions that might look like IIH. We use MRI or CT scans to check for things like tumors or brain blockages. By doing this, we can make sure it’s really IIH.
In conclusion, neuroimaging is vital for diagnosing IIH. MRI and MRV help us find IIH by looking for specific signs and ruling out other causes.
Differential Diagnosis Considerations
When diagnosing idiopathic intracranial hypertension, it’s key to look at many possible causes. This ensures we treat the right condition. Signs like papilledema and cranial nerve issues help tell IIH apart from other problems.
Conditions Mimicking IIH
Some conditions can look like IIH, making diagnosis tough. These include:
- Sinusitis and other causes of headache: Headaches from sinusitis or other reasons can be mistaken for IIH.
- Multiple sclerosis: Some with multiple sclerosis might show symptoms like IIH.
- Chronic meningitis: This can also cause high pressure inside the skull.
Secondary Causes of Intracranial Hypertension
It’s also vital to find out why intracranial pressure might be high. This can be due to:
- Medication side effects: Some meds, like tetracyclines and vitamin A, can raise pressure.
- Endocrine disorders: Issues like hypothyroidism and Addison’s disease can also cause high pressure.
- Sleep apnea: This condition has been linked to increased pressure inside the skull.
Cerebral Venous Sinus Thrombosis
Cerebral venous sinus thrombosis (CVST) is another condition to consider. It can cause high pressure and symptoms like IIH.
For IIH, treatments like losing weight, using diuretics, and spinal taps are options. These should be considered after a correct diagnosis.
Diagnostic Challenges and Special Populations
Diagnosing idiopathic intracranial hypertension (IIH) is tough, mainly in special groups. With more obesity, we face the challenge of spotting IIH in different patients.
New imaging tools help us see changes in the optic nerve without surgery. But, some groups are harder to diagnose.
Pediatric IIH Diagnosis
It’s hard to spot IIH in kids because they don’t always show symptoms like adults do. They might not say they have a headache or can’t explain their feelings well.
- Kids might show signs like being irritable or sleepy instead.
- Doctors must use their best guess, eye exams, and scans to diagnose.
We should think of IIH when kids have headaches or vision problems.
Diagnosis in Men and Non-Obese Patients
IIH is often linked to obesity, mainly in women. But, men and those who aren’t obese can also get it. This makes diagnosing them tricky.
Demographic | Diagnostic Considerations |
Men | Lower index of suspicion due to lower prevalence; careful evaluation of symptoms necessary |
Non-obese patients | Consider alternative causes of intracranial hypertension; thorough medical history essential |
Atypical Presentations and Diagnostic Pitfalls
IIH can show up in different ways, making diagnosis tricky. For example, some patients might not have swelling in the optic nerve or normal pressure in their spinal fluid.
We need to watch out for these unusual signs to avoid missing the diagnosis. A careful and thorough check-up is key to treating IIH in all patients right.
Conclusion
Diagnosing Idiopathic Intracranial Hypertension (IIH) needs a detailed approach. This includes looking at symptoms, risk factors, and specific criteria. We’ve talked about what IIH is, how it works, and how common it is.
Understanding IIH’s causes, like obesity and hormones, is key. A full check-up is vital for diagnosing IIH. This includes looking at your medical history and doing a physical exam.
Neurological and eye exams are also important. They help spot signs like swelling in the eyes and check your vision. The modified Dandy criteria and current standards help doctors diagnose IIH. Neuroimaging tests rule out other conditions.
In conclusion, diagnosing IIH requires a detailed process. Managing IIH involves losing weight, using diuretics, and getting spinal taps. Sometimes, surgery is needed. By understanding how to diagnose IIH, doctors can give top-notch care to those affected.
FAQ
What is Idiopathic Intracranial Hypertension (IIH)?
Idiopathic Intracranial Hypertension (IIH) is a condition where the brain’s pressure goes up without a known reason. It mainly affects obese women who are of childbearing age.
What are the diagnostic criteria for IIH?
To diagnose IIH, doctors look at several things. These include the Modified Dandy Criteria and current standards. They check the patient’s symptoms, do a neurological exam, and look at the eyes. They also do a lumbar puncture and use neuroimaging.
How is opening pressure measured during a lumbar puncture?
During a lumbar puncture, doctors use a manometer to check the cerebrospinal fluid pressure. If it’s over 250 mmCSF, it might mean IIH.
What is the role of neuroimaging in diagnosing IIH?
Neuroimaging, like MRI and MR venography, is key in diagnosing IIH. It helps rule out other conditions and checks if the veins in the brain are open.
Can IIH occur without papilledema?
Yes, some people with IIH don’t have papilledema. This is true for about 5-10% of cases. It makes diagnosing IIH harder.
What are the common clinical presentations of IIH?
People with IIH often have headaches, vision problems, tinnitus, and nausea. These symptoms help doctors diagnose and manage IIH.
How do risk factors contribute to the development of IIH?
Several factors can lead to IIH. These include being overweight, hormonal changes, and other health conditions. These are more common in women of childbearing age.
What is the significance of ophthalmologic evaluation in IIH diagnosis?
Eye exams are very important in diagnosing IIH. They check for papilledema, do visual field tests, and use Optical Coherence Tomography (OCT). This helps see how IIH affects the eyes.
How is IIH diagnosed in special populations, such as children and men?
Diagnosing IIH in children and men needs a special approach. They might not show symptoms in the same way as women. This makes diagnosis tricky.
What are the differential diagnoses to consider when evaluating a patient for IIH?
When checking for IIH, doctors also look at other conditions. These can mimic IIH or cause similar symptoms. They also consider cerebral venous sinus thrombosis.
References
National Center for Biotechnology Information. Diagnosing Idiopathic Intracranial Hypertension in Women. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7385768/