
Every year, surgeons do over 200,000 brain surgeries in the United States. Many of these surgeries are in very delicate parts of the brain. To help, we use a key method called intraoperative brain mapping. It helps us find and keep safe the most important brain functions during surgery.
This method lets neurosurgeons find and protect the most vital areas. It lowers the chance of problems after surgery. By using functional brain mapping surgery, we make sure patients get the best results from their surgeries.
Key Takeaways
- Intraoperative brain mapping is a key tool in neurosurgery.
- It helps find and keep safe the most important brain functions during surgery.
- The method cuts down the risk of problems after surgery.
- Functional brain mapping surgery helps patients get the best results.
- Neurosurgeons use neurosurgical mapping techniques for complex surgeries.
Understanding Intraoperative Brain Mapping
Intraoperative brain mapping is a key tool in neurosurgery today. It helps surgeons understand the brain’s complex layout better. This method gives feedback in real-time, making surgeries safer and more effective.
Definition and Basic Principles
Intraoperative brain mapping is about finding and keeping safe important brain parts during surgery. It uses direct cortical stimulation and other methods to map brain functions live. The goal is to avoid harming areas that control important functions like movement, language, and feeling.
A team of neurosurgeons, neurophysiologists, and sometimes neuropsychologists work together. They watch and map brain activity during surgery. This teamwork helps the team make quick, informed decisions, balancing removing bad tissue with keeping brain function safe.
Historical Development of Brain Mapping Techniques
Brain mapping has a long history, starting in the early 20th century. At first, it relied on anatomical landmarks and pre-op images. Later, it evolved to include functional mapping, like awake craniotomy brain mapping. This method keeps patients awake during surgery to check their brain function live.
New technology has greatly helped brain mapping grow. Today, we have intraoperative cortical stimulation and advanced imaging. These tools give detailed maps of brain functions and structures.
Importance in Modern Neurosurgery
Intraoperative brain mapping is vital in today’s neurosurgery, like in brain tumor mapping surgery and cortical mapping surgery. It helps surgeons remove bad tissue while protecting important brain areas.
This method’s value is in its ability to enhance surgery results and patient care. It gives surgeons real-time feedback. This allows them to make accurate decisions during surgery, lowering the chance of neurological problems after surgery.
The Science Behind Brain Mapping
Brain mapping starts with understanding the brain’s structure and how it works. Neurosurgeons need to know the brain’s layout and function to safely operate during surgery.
Neuroanatomy Fundamentals
Neuroanatomy studies the brain’s structure and how it’s organized. It helps us see how different parts of the brain connect and work. Knowing the brain’s anatomy well is key to finding areas that control important functions like movement and language.
Functional Organization of the Brain
The brain’s organization is about how different parts work together. This is vital for effective brain mapping. Neuroscientists say, “The brain’s organization is complex and changes, needing precise mapping to protect important areas.”
“The brain is a highly interconnected organ, and its function cannot be understood by examining its parts in isolation.”
Eloquent Brain Areas and Their Significance
Eloquent brain areas are key for functions like movement, language, and feeling. Finding and keeping these areas safe during surgery is essential. Motor cortex mapping and language cortex mapping help locate these areas, avoiding damage.
The role of mapping these brain areas is huge. It helps neurosurgeons work more precisely, lowering the chance of harming important brain functions. As surgery methods improve, the need for accurate brain mapping will grow even more.
Indications for Intraoperative Brain Mapping
Intraoperative brain mapping is key in making neurosurgery safer and more effective. It’s used in many complex surgeries to help patients get the best results.
Brain Tumor Resection
Removing brain tumors is a big reason for using intraoperative brain mapping. It helps doctors find and keep important brain parts safe during surgery. This way, they can remove more tumors and cause less harm to the brain.
Epilepsy Surgery
It’s also vital in epilepsy surgery. It helps find where seizures start and important brain spots. This lets neurosurgeons remove the problem area without harming other parts of the brain.
Vascular Lesions
Vascular lesions, like AVMs, need careful planning and surgery. Intraoperative brain mapping helps spot important brain areas near these lesions.
Other Neurosurgical Applications
Intraoperative brain mapping is also used in other neurosurgery cases. This includes surgeries for cavernous malformations and some functional neurosurgery.
|
Neurosurgical Procedure |
Role of Intraoperative Brain Mapping |
Benefits |
|---|---|---|
|
Brain Tumor Resection |
Identification and preservation of eloquent brain areas |
Maximizes tumor removal, minimizes neurological deficits |
|
Epilepsy Surgery |
Identification of seizure foci and critical brain areas |
Effective removal of epileptogenic zone, preservation of brain function |
|
Vascular Lesions |
Identification of critical brain areas surrounding lesions |
Precise surgical planning and execution |
Types of Intraoperative Brain Mapping Techniques
Neurosurgeons use many intraoperative brain mapping techniques during surgery. These methods help them find and keep important brain areas. This is key to getting the best results for patients with neurosurgical needs.
Direct Cortical Stimulation
Direct Cortical Stimulation is a common method in brain mapping. It uses electrical stimulation on the brain’s surface. This helps find areas that control things like movement or language.
By doing this, surgeons can make a map of the brain’s functions. This map helps them avoid harming important brain parts during surgery.
This method is very helpful in surgeries for brain tumors or epilepsy. It’s used to keep important brain areas safe.
The stimulation is done with a bipolar electrode. The surgical team watches the brain’s responses closely.
Subcortical Stimulation
Subcortical Stimulation is another important technique. It stimulates the brain’s white matter tracts. This is below the brain’s surface.
This is key when dealing with deep-seated tumors. It helps avoid harming vital pathways.
By using this method, surgeons can see how close they are to important fiber tracts. This reduces the chance of neurological problems after surgery.
Intraoperative EEG Mapping
Intraoperative EEG Mapping uses electroencephalography (EEG) during surgery. It watches brain activity in real-time. This helps find seizure foci or watch for signs of irritation or ischemia.
EEG mapping is very useful in epilepsy surgery. It helps pinpoint the area causing seizures. It also checks how anesthesia affects the brain and overall activity during surgery.
Evoked Potentials
Evoked Potentials are electrical signals from the nervous system. In brain mapping, they check the health of sensory and motor pathways.
Recording these potentials lets surgeons see how these pathways are doing in real-time. This allows them to adjust the surgery plan if needed.
Awake Craniotomy Brain Mapping
Awake craniotomy brain mapping is a complex surgery. It requires skill and care for the patient. The surgery removes part of the skull while the patient is awake. This helps map brain functions accurately.
Patient Selection Criteria
Choosing the right patients for awake craniotomy is key. Patients with tumors or lesions near important brain areas are best. We check each patient’s health, brain status, and ability to follow instructions during surgery.
A team of neurosurgeons, anesthesiologists, and sometimes psychologists review each patient. They decide if the patient is right for the awake procedure.
Anesthesia Considerations
Managing anesthesia in awake craniotomy is tough. We mix local anesthesia with conscious sedation. This keeps the patient comfortable but alert when needed.
“The goal is to balance comfort with the need for the patient to stay awake,” say experts.
Surgical Procedure Steps
The surgery has several important steps. First, we do a craniotomy under local anesthesia. Then, we map brain functions with electrical stimulation.
- Patient preparation and positioning
- Craniotomy and exposure
- Brain mapping and tumor resection
- Closure
Patient Experience and Management
Managing the patient’s experience is critical. We make sure patients are informed and supported. This helps the surgery go smoothly.
Patients might feel anxious before surgery. But with the right support, they can stay calm and cooperate.
Motor Cortex Mapping
Neurosurgeons use motor cortex mapping to navigate the brain’s complex anatomy during surgery. This method is key to keeping motor function safe in patients.
Anatomical Considerations
The motor cortex is in the precentral gyrus of the frontal lobe. Knowing its anatomy is vital for mapping. The primary motor cortex controls voluntary movements, making its exact location critical during surgery.
The motor cortex is organized by body parts, like a homunculus. This shows how different areas control different parts of the body.
Stimulation Parameters
Stimulation parameters are key for motor cortex mapping. The intensity, frequency, and duration of the stimulation affect the response. A bipolar electrode is used to stimulate the cortex directly.
The stimulation starts at a low intensity and increases until a motor response is seen. Adjusting the frequency can also help in getting a response.
Response Interpretation
Understanding the responses from motor cortex mapping is complex. The type and characteristics of the response give insights into the neural structures.
Accurate interpretation needs a deep understanding of neurophysiology and the stimulation used. The patient’s clinical context and any preoperative data are also important.
Clinical Applications
Motor cortex mapping is vital in neurosurgery. It’s most useful in surgeries near or within the motor cortex, like brain tumors or vascular malformations.
|
Clinical Scenario |
Role of Motor Cortex Mapping |
|---|---|
|
Brain Tumor Surgery |
Helps in maximizing tumor resection while preserving motor function |
|
Epilepsy Surgery |
Aids in identifying and preserving eloquent cortex |
|
Vascular Lesion Surgery |
Assists in navigating complex anatomy to avoid motor deficits |
By using motor cortex mapping in neurosurgery, we can greatly improve patient outcomes. This method, along with advanced imaging and monitoring, helps us safely remove lesions while keeping important brain functions intact.
Language Function Mapping
Language function mapping is key in neurosurgery, focusing on brain areas for speech and understanding. Neurosurgeons aim to keep language skills safe during surgery. This is a big challenge that needs exact mapping of language functions.
Language Network Anatomy
The brain’s language network is complex, with many regions and paths. Broca’s area and Wernicke’s area are vital, handling speech and understanding. Knowing these areas and their links is key for good language mapping.
Intraoperative Language Testing Methods
We test language during surgery to find brain areas for language. We use direct cortical stimulation to briefly stop language function and see how the patient reacts. This helps us make a detailed map of the patient’s language network.
Interpretation of Language Responses
Understanding language responses during testing is important. We look at speech, understanding, and reading. By studying these, we find out which areas are key for language and try not to harm them during surgery.
Preserving Language Function
Our main goal is to keep language function safe during mapping. By finding and avoiding important language areas, we lower the chance of language problems after surgery. We also work with speech-language pathologists to help patients recover or keep their language skills.
With careful planning, precise testing, and a focus on the patient, we aim to improve language results for those having neurosurgery.
Sensory Cortex Mapping
Sensory cortex mapping is key in neurosurgery. It helps keep important sensory functions safe. The sensory cortex handles touch, temperature, and pain from the body. It’s vital for neurosurgeons to map this area well to protect it during surgery.
Somatosensory Mapping Techniques
Somatosensory mapping finds brain spots for body sensory info. Direct cortical stimulation is one method. It uses a small electrical current to pinpoint sensory areas. This helps neurosurgeons make detailed maps of the sensory cortex.
Another method is somatosensory evoked potentials (SSEPs). They record brain electrical activity from sensory stimulation. SSEPs show how well sensory pathways work, helping neurosurgeons during surgery.
Visual Pathway Mapping
Visual pathway mapping is key for surgeries near the visual paths. Visual evoked potentials (VEPs) check visual pathway function. VEPs record brain activity from visual stimuli, giving feedback on visual pathway health.
Intraoperative visual pathway mapping helps avoid damage to visual areas. This is critical for surgeries near the optic nerves and tracts. It reduces the chance of vision problems after surgery.
Auditory Function Mapping
Auditory function mapping is vital for surgeries near the hearing paths. Auditory brainstem responses (ABRs) and cortical auditory evoked potentials (CAEPs) check hearing during surgery. These tests show if the hearing paths are working, helping to protect hearing.
By mapping hearing functions well, neurosurgeons can lower the risk of hearing loss. This improves patient outcomes and quality of life.
Cognitive Function Assessment During Surgery
Intraoperative cognitive function assessment is key in neurosurgery. It helps keep the brain safe and ensures the best results for patients. We use many methods to check different parts of brain function. This helps us make smart choices during surgery.
Memory Testing
Memory tests during surgery check if patients can remember things. We use simple tasks like remembering words or pictures. Intraoperative memory testing shows us where in the brain memory happens. This helps us avoid harming these areas during surgery.
Executive Function Evaluation
Executive functions are high-level brain tasks like planning and solving problems. We test these during surgery with complex tasks. Intraoperative evaluation of executive functions is key to keeping patients independent and able to do daily tasks.
Attention and Concentration Assessment
Testing attention and concentration during surgery checks if patients can focus. We use tasks like simple math or spotting visual cues. Attention and concentration assessment shows how surgery might affect how patients interact with their world.
Emotional and Behavioral Monitoring
Monitoring emotions and behavior during surgery is vital. It helps us see how patients react to surgery. Emotional and behavioral monitoring is very important when surgery affects emotional areas of the brain.
By fully checking brain function during surgery, we can make surgery better. This is a big step forward in neurosurgery. It lets us do surgery more precisely and effectively.
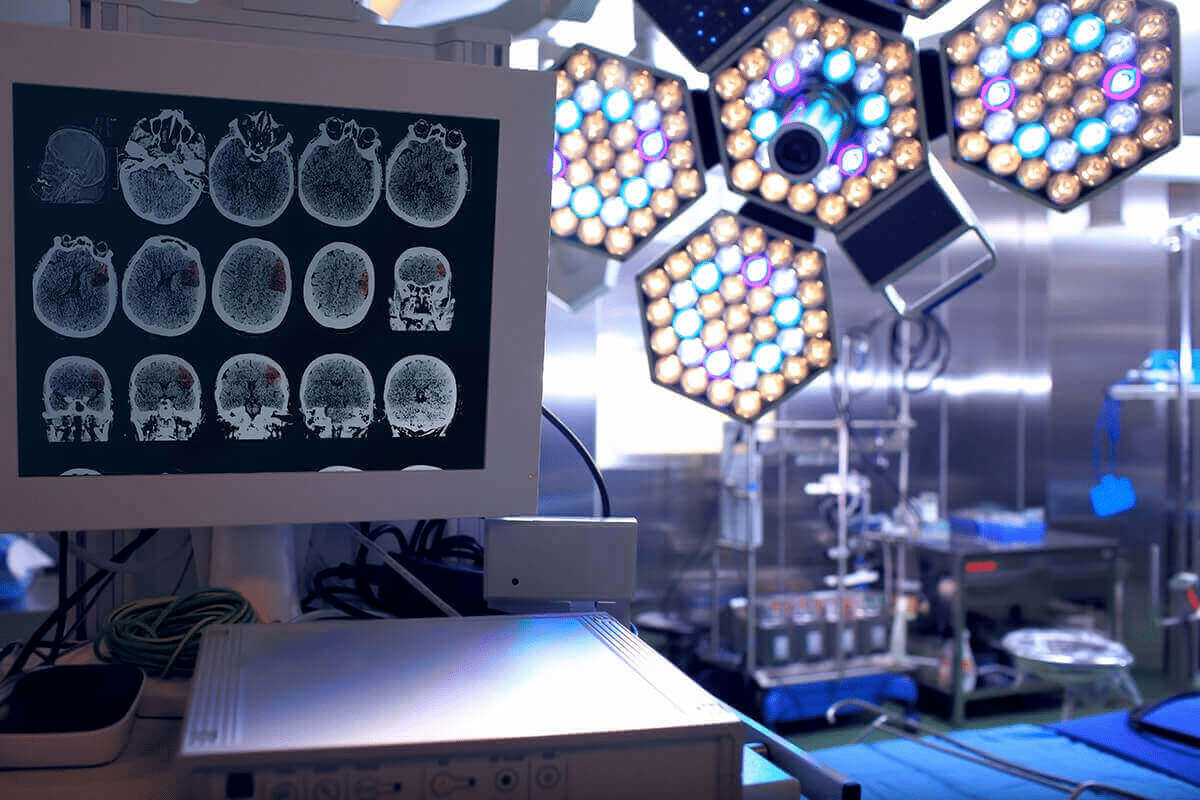
Technology and Equipment for Intraoperative Brain Mapping
The success of intraoperative brain mapping depends on advanced technology and specialized equipment. These tools help neurosurgeons accurately identify and preserve critical brain areas during surgery.
Stimulation Devices
Stimulation devices are key for intraoperative brain mapping. They allow surgeons to directly stimulate brain areas to check their function. Direct cortical stimulation is a method used to find out what different brain regions do by applying electrical impulses.
These devices are made to be precise and safe. They have features like adjustable intensity and frequency. This meets different patient needs and surgical requirements.
Monitoring Equipment
Monitoring equipment is vital for intraoperative brain mapping. It continuously checks the patient’s neurological function during surgery. This includes electroencephalography (EEG) and evoked potentials, which monitor the brain’s electrical activity and response to stimuli.
Advanced monitoring systems give real-time data. This allows for immediate adjustments to the surgical approach if needed. It enhances patient safety and outcomes.
Neuronavigation Systems
Neuronavigation systems are advanced tools that guide surgeons during brain surgery. They use preoperative imaging data to create a detailed brain map. This helps surgeons navigate complex anatomy with greater precision.
By combining neuronavigation with intraoperative brain mapping, surgeons can accurately identify and preserve critical brain structures. This improves the safety and effectiveness of the procedure.
Integration with Imaging Modalities
The integration of intraoperative brain mapping with advanced imaging modalities like functional MRI (fMRI) and diffusion tensor imaging (DTI) has greatly improved neurosurgical procedures.
These imaging techniques give detailed information about brain anatomy and function. This information guides stimulation and monitoring during surgery. It leads to better patient outcomes.
Preoperative Planning for Brain Mapping Procedures
Brain mapping procedures need careful planning before surgery. This step helps neurosurgeons understand the brain’s complex structures. It prepares them for the surgery.
Functional MRI and Tractography
Functional MRI (fMRI) and tractography are key in planning. fMRI shows brain areas for important functions like moving, speaking, and seeing. Tractography maps the brain’s connections.
Together, these tools create a detailed brain map. This map is essential for planning the surgery. It helps avoid harming important brain areas.
Patient Counseling and Preparation
Talking to patients is a big part of planning. They need to know the surgery’s risks, benefits, and other options. We answer their questions and help them feel ready for the surgery.
Multidisciplinary Team Approach
A team of experts is essential for planning. Our team includes neurosurgeons, neuroradiologists, and neuropsychologists. They work together to plan the surgery.
|
Team Member |
Role in Preoperative Planning |
|---|---|
|
Neurosurgeon |
Develops the surgical plan and identifies the optimal approach. |
|
Neuroradiologist |
Interprets imaging studies, including fMRI and tractography. |
|
Neuropsychologist |
Assesses the patient’s cognitive function and identifies possible concerns. |
Our team’s collaboration ensures a well-rounded plan. This leads to a safer and more effective surgery.
Challenges and Limitations of Intraoperative Brain Mapping
Intraoperative brain mapping has many benefits but also faces challenges. Neurosurgeons must overcome these hurdles to improve patient care. Knowing these limitations helps us refine the technique and better serve our patients.
Technical Challenges
One big challenge is the need for precise mapping. This requires advanced tools and skilled people to read the data right. Technical issues like broken equipment or software problems can ruin the procedure.
- Ensuring the accuracy of neuronavigation systems
- Managing the complexity of data from various imaging modalities
- Maintaining sterility and safety during the procedure
Patient-Related Factors
Patients’ unique factors also affect intraoperative brain mapping. Differences in brain anatomy and pathological conditions can make mapping harder. The patient’s age, health, and past treatments also matter.
- Assessing patient suitability for awake craniotomy
- Managing patient comfort and anxiety during the procedure
- Adapting to unexpected patient responses during mapping
Interpretation Difficulties
Understanding the data from intraoperative brain mapping is tough. The brain’s complexity and the changing surgical environment make it hard. Neurosurgeons must quickly sort out what’s important to make good decisions.
- Distinguishing between different types of brain signals
- Correlating mapping data with preoperative imaging
- Making real-time decisions based on mapping results
Surgical Time Constraints
Time is a big challenge in intraoperative brain mapping. Finding the right balance between thoroughness and speed is hard. Too long a surgery can lead to complications. Managing time well is key to accurate and timely mapping.
By tackling these challenges, we can make intraoperative brain mapping safer and more effective. This will help us give better care to our patients.
Outcomes and Benefits of Intraoperative Brain Mapping
Intraoperative brain mapping has significantly transformed the field of neurosurgery. It gives feedback in real time during complex surgeries. This makes surgeries more precise and safe.
Extent of Tumor Resection
This method helps remove more of the tumor. It shows where the tumor starts and ends. This way, doctors can remove more of it.
Studies show that using this method leads to better results. Patients do better when more of the tumor is removed.
Functional Preservation Rates
This method also helps keep important brain areas safe. Doctors can see and check brain function during surgery. This helps avoid harming areas that control movement, feeling, and language.
Because of this, patients can keep more of their brain function. They can move better and talk better after surgery.
Quality of Life Outcomes
Keeping brain function helps patients live better lives. They recover faster and can do things they love again. This is a big plus of using this method.
Long-term Survival Benefits
Removing more of the tumor and keeping brain function also helps patients live longer. For people with brain tumors, removing as much as possible is key. This method helps doctors do that.
In summary, intraoperative brain mapping brings many benefits. It helps remove more tumor, keeps brain function, improves life quality, and helps patients live longer. As it gets better, it will be even more important in neurosurgery.
Future Directions in Intraoperative Brain Mapping
Intraoperative brain mapping is on the verge of a big change. This is thanks to technological advancements. New areas are showing great promise for future growth.
Technological Advancements
Technological innovation is driving progress in brain mapping. Advances in neuroimaging, neuromonitoring, and surgical tools are making procedures more precise. For example, using high-field MRI and intraoperative ultrasound improves tumor removal and reduces damage risks.
- Improved imaging modalities for better visualization
- Advanced neuromonitoring techniques for enhanced safety
- Innovative surgical tools for more precise interventions
Novel Mapping Approaches
New methods in brain mapping are also being explored. Techniques like transcranial magnetic stimulation (TMS) and diffusion tensor imaging (DTI)-guided mapping offer better detail and safety.
- TMS for non-invasive cortical mapping
- DTI for detailed white matter tractography
- Functional MRI for preoperative planning and intraoperative guidance
Artificial Intelligence Applications
The use of artificial intelligence (AI) in brain mapping is exciting. AI can analyze data from neuroimaging and electrophysiology to guide surgery in real-time. This leads to more accurate mapping and shorter surgery times.
Personalized Mapping Protocols
Creating personalized mapping protocols is also key. Tailoring strategies to each patient’s unique anatomy and condition improves outcomes and reduces risks. This involves combining data from various tests to create a detailed, patient-specific plan.
- Customized stimulation parameters based on patient-specific anatomy
- Integration of preoperative and intraoperative data for personalized mapping
- Adaptive mapping protocols to adjust to changing surgical conditions
Looking ahead, these advancements will change neurosurgery. They will make surgeries more precise, safe, and effective.
Conclusion
Intraoperative brain mapping has significantly transformed the field of neurosurgery. It helps surgeons find and remove tumors carefully. This way, they can save important brain functions.
We’ve talked about how complex this method is. It uses direct stimulation and advanced imaging. These tools have made surgeries better and helped the field grow.
This technology has changed how we do neurosurgery. By improving these methods, we can help patients even more. We can do more in neurosurgery than ever before.
Looking ahead, we need new ideas and tech to keep improving. We must also make these methods fit each patient better. This will lead to better results and a better life for patients.
FAQ
What is intraoperative brain mapping?
Intraoperative brain mapping is a technique used in brain surgery. It helps identify and protect important brain areas. This reduces the risk of problems after surgery.
Why is intraoperative brain mapping important in neurosurgery?
It’s key in neurosurgery because it helps locate and protect vital brain areas. This improves surgical results and patient care.
What are the different types of intraoperative brain mapping techniques?
There are several techniques. These include direct cortical stimulation, subcortical stimulation, intraoperative EEG mapping, and evoked potentials.
What is awake craniotomy brain mapping?
Awake craniotomy brain mapping is a surgery where the patient stays awake. It allows for real-time monitoring of brain function and precise mapping of critical areas.
How is motor cortex mapping performed?
Motor cortex mapping uses direct cortical stimulation. It identifies motor areas of the brain. Careful consideration of anatomical landmarks and response interpretation is key.
What is the significance of language function mapping during surgery?
Language function mapping is vital during surgery. It helps identify and preserve language areas. This minimizes the risk of language problems after surgery.
How is sensory cortex mapping performed?
Sensory cortex mapping uses techniques like somatosensory mapping and visual pathway mapping. It identifies and preserves sensory areas of the brain.
What is the role of cognitive function assessment during surgery?
Cognitive function assessment during surgery evaluates memory, executive function, attention, and concentration. It ensures critical cognitive areas are preserved.
What technology and equipment are used in intraoperative brain mapping?
Various technologies are used, including stimulation devices and monitoring equipment. Neuronavigation systems and imaging modalities are also integrated.
What are the challenges and limitations of intraoperative brain mapping?
Challenges include technical difficulties and patient-related factors. Interpretation difficulties and time constraints during surgery are also limitations.
What are the benefits of intraoperative brain mapping?
It improves tumor resection rates and functional preservation. It also enhances quality of life and long-term survival benefits.
What are the future directions in intraoperative brain mapping?
Future directions include technological advancements and novel mapping approaches. Artificial intelligence applications and personalized protocols are also on the horizon.
How does preoperative planning contribute to successful brain mapping?
Preoperative planning is essential. It includes functional MRI, tractography, patient counseling, and a multidisciplinary team approach. These steps lead to successful brain mapping and optimal surgical outcomes.
References
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://pubmed.ncbi.nlm.nih.gov/19795953/









