
Did you know millions of surgeries happen worldwide every year? The time during these surgeries, called intraoperative, is key for patient care and success. Learn what is intraoperative definition. Understand the precise meaning of the term clearly.
Knowing what intraoperative means is important for doctors and patients. It’s the time from the first cut to the last stitch during surgery.
This critical phase needs clear medical terms and teamwork. It’s all about keeping patients safe and getting the best results.
Key Takeaways
- Intraoperative refers to the period during a surgical operation.
- Understanding intraoperative terminology is important for doctors and patients.
- The intraoperative phase is critical for patient care and surgical success.
- Clear communication during this phase is essential for patient safety.
- Medical terminology plays a vital role in the intraoperative period.
Intraoperative Definition: Medical Terminology Explained
Understanding ‘intraoperative’ is key to understanding surgery. The intraoperative period is a critical part of surgery. It’s when the surgical team does the operation.
Etymology and Origin of the Term “Intraoperative”
The word “intraoperative” comes from Latin. “Intra” means “within” or “during,” and “operatio” means “operation” or “work.” So, “intraoperative” means “during the operation” or “within the operation.”
In medical texts, this term is used to talk about things that happen during surgery. For example, “intraoperative complications” are problems that come up during the surgery.
“The intraoperative period is a dynamic phase where the surgical team’s actions are critical for the success of the operation.”
— Surgical Care Team
Clinical Context and Usage in Medical Literature
In medical settings, “intraoperative” points to the time when certain actions are taken or events happen. It’s important for doctors to talk clearly about when things happen during surgery.
|
Term |
Definition |
Example |
|---|---|---|
|
Intraoperative |
Occurring during surgery |
Intraoperative bleeding |
|
Intraoperative care |
Care provided during surgery |
Intraoperative monitoring |
|
Intraoperative complications |
Complications arising during surgery |
Intraoperative hemorrhage |
Knowing what “intraoperative” means is very important for good surgery and patient care. It helps doctors work together better during surgery.
The Three Phases of Surgical Care: Where Intraoperative Fits
Recognizing the three phases of surgical care is vital for improving patient outcomes. These phases work together, giving patients full care from start to finish.
Preoperative Phase Overview
The preoperative phase starts the surgical care journey. It’s where we get ready for surgery. This includes checks and steps to make the patient ready.
- Medical checks to spot any risks or issues.
- Guidance for patients on fasting, meds, and more.
- Getting the patient’s consent, explaining the surgery’s risks and benefits.
Intraoperative Period Explained
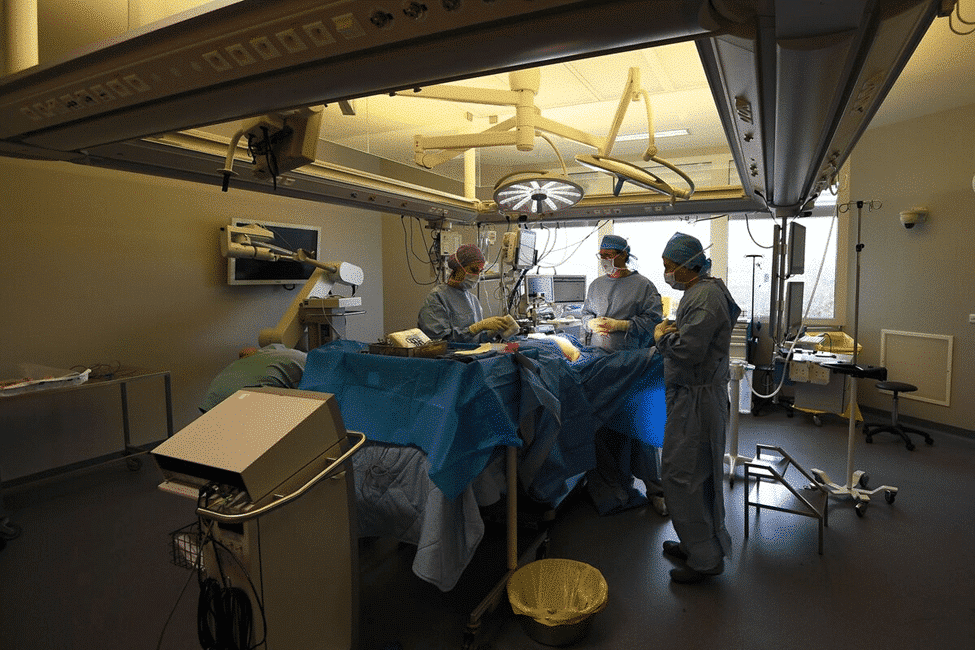
The intraoperative phase is when the surgery happens. It’s a time of great focus and teamwork. Key parts include:
- Keeping an eye on the patient’s health.
- Managing pain and anesthesia for comfort.
- Following the surgery plan, adjusting as needed.
Postoperative Phase Characteristics
The postoperative phase starts after surgery and goes until the patient is ready to go home. It’s about:
- Watching the patient’s recovery, managing pain and complications.
- Teaching wound care and post-op instructions.
- Planning follow-up care and rehab for a smooth recovery.
By managing these three phases well, healthcare can improve patient outcomes and care quality.
Key Components of the Intraoperative Period
Understanding the essential aspects of the intraoperative period is crucial for providing excellent patient care. This phase is a critical part of surgery. It includes important elements that help make sure the surgery goes well.
Timeframe and Boundaries
The intraoperative period has its own start and end times. It starts when the patient goes into the operating room. It ends when they move to the recovery room or intensive care unit. Knowing the medical procedure timing helps the care team work better together.
The length of the intraoperative period can change a lot. It depends on the surgery’s complexity, the patient’s health, and the team’s experience. Managing the surgery duration phase well is important to keep risks low and improve patient results.
Critical Events During the Intraoperative Phase
Many important events happen during the intraoperative phase. These include starting the anesthesia, making the surgical incision, and finishing the surgery. Watching and handling these events carefully is key to keeping the patient safe and the surgery a success.
Intraoperative monitoring meaning is about watching the patient’s vital signs and how their body reacts during surgery. This watching is very important. It helps catch any bad reactions or problems early, so we can act fast.
Transition Points in Surgical Care
Transition points in the intraoperative period are very important. They are when the patient’s care moves from one person to another or from one place to another. Making sure these transitions go smoothly is vital. It helps keep the care going without breaks and prevents mistakes that could harm the patient.
Good communication among the surgical team is essential for smooth transitions. By working together and talking clearly, we can make sure our patients get the best care during the intraoperative period.
Intraoperative Patient Management
The intraoperative phase is all about careful patient management for the best results. It’s key to keep patients safe, avoid complications, and help them recover well.
Vital Signs Monitoring
Monitoring vital signs is vital in the operating room. We watch heart rate, blood pressure, oxygen levels, and breathing rate closely. This helps us catch any problems early.
With constant monitoring, the anesthesiologist and surgical team can make smart decisions. They use advanced tools to get real-time data. This helps them manage the patient’s health during surgery.
|
Vital Sign |
Normal Range |
Intraoperative Considerations |
|---|---|---|
|
Heart Rate |
60-100 bpm |
Monitor for tachycardia or bradycardia |
|
Blood Pressure |
90-140/60-90 mmHg |
Maintain within target range to ensure adequate perfusion |
|
Oxygen Saturation |
95-100% |
Ensure adequate oxygenation |
Fluid and Electrolyte Balance
Keeping fluid and electrolyte balance right is key during surgery. We manage fluids to replace what’s lost and keep blood pressure stable. We also check and adjust electrolytes to avoid problems like irregular heartbeats.
We use different types of fluids based on the patient’s needs and the surgery. We also think about the patient’s fluid status before surgery and any losses during it.
Temperature Regulation
Keeping the patient’s temperature stable is very important. Low body temperature can cause problems like bleeding issues and infections. We use warm devices and fluids to keep the body at a normal temperature.
By watching the patient’s temperature, we can adjust as needed. This helps avoid temperature-related issues and keeps the patient safe and comfortable.
Pain Management Strategies
Managing pain well is important for the patient’s comfort and recovery. We use different methods, like regional anesthesia and pain medicines, to control pain during and after surgery.
By customizing pain management for each patient, we can reduce pain and lower the chance of long-term pain. This also helps patients move around sooner and recover better.
Anesthesia in the Intraoperative Setting
In the intraoperative setting, anesthesia is key for patient care. It helps patients avoid pain and distress during surgery.
Types of Anesthesia
There are different types of anesthesia for surgeries. General anesthesia makes patients unconscious for major surgeries. Regional anesthesia numbs a body part, and local anesthesia numbs just the surgery area.
The Anesthesiologist’s Role
Anesthesiologists are vital in surgery. They give anesthesia, watch vital signs, and handle surgery issues. They work with the surgical team for the best patient care.
Monitoring Anesthetic Depth
It’s important to check anesthesia levels to keep patients safe and comfortable. We use EEG and BIS monitoring to see how awake the patient is. This helps us adjust the anesthesia.
Regional Anesthesia Techniques
Regional anesthesia involves injecting medication around nerves to numb a body part. Techniques like epidural anesthesia and nerve blocks manage pain well without general anesthesia risks.
We’ve looked at anesthesia in surgery, including types, the anesthesiologist’s role, and monitoring. Understanding these helps us see the complexity of patient care in surgery.
Intraoperative Monitoring Techniques
Keeping patients safe during surgery is key. Intraoperative monitoring uses different methods to watch the patient’s health closely during surgery.
Cardiovascular Monitoring
Watching the heart and blood pressure is vital. Techniques like ECG and invasive blood pressure monitoring give real-time data. This helps doctors and surgeons make quick decisions.
Neurological Monitoring
For surgeries that might harm the nervous system, like brain surgeries, neurological monitoring is a must. Tools like EEG and SSEP check the brain’s activity and nerve pathways.
Respiratory Monitoring
It’s important to keep the patient’s breathing and oxygen levels safe during surgery. Monitoring end-tidal CO2, pulse oximetry, and ventilator settings helps achieve this.
Advanced Monitoring Technologies
Technologies like NIRS for brain oxygen levels and TEE offer more detailed insights. They help spot and handle any surgery problems quickly.
Using these monitoring methods, doctors can greatly improve patient care and lower the chance of surgery complications.
The Surgical Team and Their Intraoperative Responsibilities
The success of surgeries depends on the teamwork during the operation. This team includes many healthcare professionals. Each one has a specific role that helps the surgery go well.
Surgeon and Assistant Surgeons
The surgeon and their assistants do the surgery. They make cuts, separate tissues, and close the wound. The main surgeon leads the team, and the assistants help as needed.
Scrub Nurses and Circulating Nurses
Scrub nurses keep the area clean and handle tools. They also help the team during the surgery. Circulating nurses manage the room, take care of the patient, and make sure everything is ready.
Anesthesia Providers
Anesthesia providers give anesthesia, watch the patient’s health, and manage pain. They are key to keeping the patient safe during surgery.
Other Specialized Personnel
Other important people in the OR include surgical technologists and radiologic technologists. They help with different parts of the surgery. Each one is vital for the surgery’s success.
|
Team Member |
Primary Responsibilities |
|---|---|
|
Surgeon and Assistant Surgeons |
Perform the surgical procedure, coordinate the surgical process |
|
Scrub Nurses |
Maintain sterile field, handle surgical instruments, assist surgical team |
|
Circulating Nurses |
Manage operating room environment, coordinate patient care, ensure equipment availability |
|
Anesthesia Providers |
Administer anesthesia, monitor vital signs, manage pain |
|
Other Specialized Personnel |
Support surgical procedure with specialized skills (e.g., surgical technologists, radiologic technologists) |
Patient Positioning and Preparation in the Operating Room
Getting patients in the right position in the operating room is key. It affects how well the surgery goes and how the patient feels. We need to think about many things to make sure patients are set up right for their surgeries.
Common Surgical Positions
Patients are put in different positions for different surgeries. Here are some common ones:
- Supine position: The patient lies on their back, often used for abdominal surgeries.
- Prone position: The patient lies on their stomach, commonly used for spinal surgeries.
- Lithotomy position: The patient’s legs are elevated and supported in stirrups, typically used for gynecological and urological procedures.
Each position needs careful thought to avoid discomfort and injury.
Preventing Positioning Injuries
Positioning injuries can happen because of too much pressure on certain body parts. To stop these injuries, we:
- Use the right padding and supports to spread out the pressure.
- Make sure the patient’s limbs aren’t too bent or straight.
- Keep an eye on the patient’s position during surgery.
Skin Preparation and Draping
Before surgery starts, the patient’s skin is prepped and draped to keep things clean. This means:
- Cleaning the skin with antiseptic solutions to lower infection risk.
- Putting on sterile drapes around the surgery area to keep it clean.
By managing patient positioning and prep well, we make surgeries safer and more effective.
Common Intraoperative Procedures and Techniques
Surgical techniques used during surgery are many and very specialized. They are key to the success of surgeries and the health of patients. We will look at common procedures and techniques, like making incisions, handling tissues, stopping bleeding, and closing wounds.
Incision and Access Methods
The first cut is very important in surgery, letting the surgeon get to the area they need to work on. The type of cut made depends on the surgery, the patient’s body, and the surgeon’s style. Common cuts include straight lines, curved lines, and crosswise cuts.
There are different ways to get to the surgical area, like open surgery and less invasive methods. Less invasive surgery uses smaller cuts and special tools to cause less damage.
Tissue Handling and Dissection
Handling tissues right and dissecting them carefully are key to avoid damage and help healing. Surgeons use tools like forceps, retractors, and electrocautery to handle tissues gently. Dissecting means carefully separating tissues to see the area they need to work on.
Hemostasis Techniques
Hemostasis is stopping bleeding during surgery. It’s very important to keep the area clear and avoid problems. Surgeons use ligatures, electrocautery, and special agents to stop bleeding.
Closure Methods
After surgery, surgeons use techniques to close the cut. The method chosen depends on the surgery, the size and where the cut is, and the patient’s health. Common methods include stitching, stapling, and using adhesives.
|
Technique |
Description |
Advantages |
|---|---|---|
|
Suturing |
Using threads to close incisions |
Flexible, can be used for various tissue types |
|
Stapling |
Using staples to close incisions |
Quick, secure, and efficient |
|
Adhesive Materials |
Using adhesives to close incisions |
Minimally invasive, reduces scarring |
In conclusion, the procedures and techniques used in surgery are vital for success. Knowing these is key for healthcare workers to give the best care to their patients.
Minimally Invasive and Advanced Surgical Approaches
The world of surgery is changing fast. Now, we use new methods that are less invasive. These methods help patients heal faster, feel less pain, and have smaller scars. It’s key to know about these new ways of surgery.
Laparoscopic Techniques
Laparoscopic surgery is a type of minimally invasive surgery. It uses small cuts for a camera and tools. This method is popular because it makes patients recover quicker and feel less pain.
“Laparoscopic surgery has changed how we treat many health issues,” says a top surgeon. “It’s a better choice than old-school open surgery.”
Endoscopic Procedures
Endoscopic procedures are another way to do surgery without big cuts. A tube with a camera and light is used to see inside the body. These are used for many surgeries, like in the stomach, lungs, and kidneys.
Endoscopy lets doctors do tests and treatments without hurting the patient much.
Robotic-Assisted Surgery
Robotic-assisted surgery is a big step forward. It lets surgeons do complex tasks with more control and precision. This can lead to better results for patients.
“Robotic surgery is changing what’s possible in surgery,” says a robotic surgery expert. “It lets us do things we couldn’t before.”
Hybrid Operating Rooms
Hybrid operating rooms mix advanced imaging with traditional surgery setups. They have tools like X-rays and MRI for live images during surgery. This helps surgeons do detailed work.
In short, new surgical methods are making a big difference. They help patients and doctors a lot. As we keep using new tech, we’ll see even better care for patients.
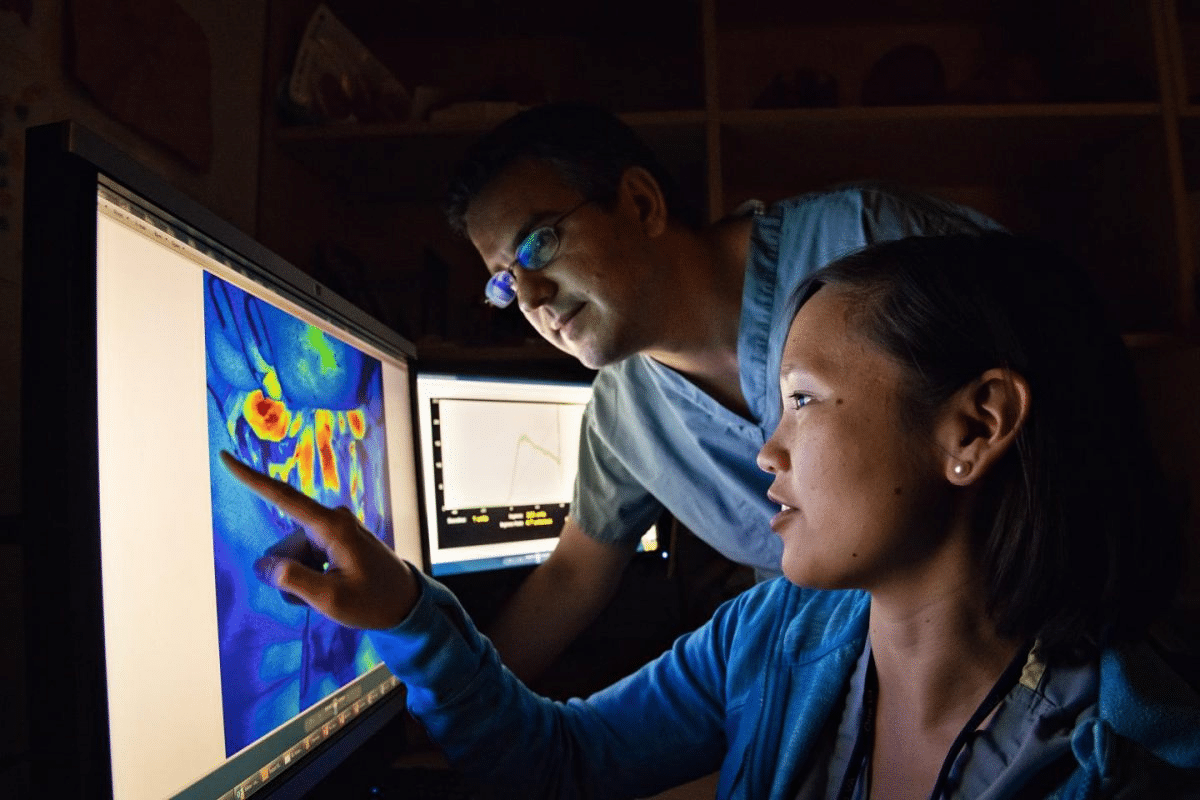
Intraoperative Imaging and Diagnostic Tools
Intraoperative imaging and diagnostic tools are key for guiding surgeries and keeping patients safe. They help surgeons make quick, informed decisions. This can lead to better outcomes and fewer complications.
Fluoroscopy and X-ray
Fluoroscopy and X-ray are common tools used during surgery. They show what’s inside the body in real-time. Fluoroscopy is great for orthopedic and vascular surgeries, helping place implants and grafts accurately.
Key applications of fluoroscopy include:
- Guiding the placement of orthopedic hardware
- Assisting in vascular procedures such as angioplasty
- Verifying the correct positioning of catheters and stents
Ultrasound Applications
Intraoperative ultrasound provides real-time images without radiation. It’s used in many surgeries, like neurosurgery and cardiothoracic surgery. It’s very useful.
Benefits of intraoperative ultrasound include:
- Enhanced visualization of soft tissue structures
- Ability to assess blood flow and organ perfusion
- Guidance for tumor resection and biopsy procedures
CT and MRI in the Operating Room
Advanced operating rooms now use CT and MRI for detailed imaging during surgery. These tools give surgeons the detailed info they need for complex surgeries.
|
Imaging Modality |
Key Features |
Surgical Applications |
|---|---|---|
|
CT |
High-resolution cross-sectional imaging |
Neurosurgery, orthopedic surgery |
|
MRI |
Excellent soft tissue differentiation |
Neurosurgery, oncologic surgery |
Emerging Imaging Technologies
New technologies in intraoperative imaging are exciting. These include augmented reality, photoacoustic imaging, and optical coherence tomography. They promise to improve surgery even more.
Potential benefits of emerging technologies:
- Improved visualization of complex anatomy
- Enhanced precision in tumor resection
- Reduced need for revision surgeries
Intraoperative Medication Administration
Intraoperative medication administration is key to patient safety and successful surgery. This critical phase needs careful medication management to avoid complications and get the best results.
Antibiotics and Infection Prevention
Antibiotics are vital during surgery to prevent infections. Prophylactic antibiotics help lower the risk of infections, which is important in high-risk surgeries.
“The timely administration of antibiotics is critical in reducing the incidence of SSIs,” the CDC says. We give antibiotics right before the surgery starts to help prevent infections.
Emergency Medications
Emergency medications are needed for sudden problems like severe bleeding or allergic reactions. Quick and correct use of these drugs is essential for patient safety.
We have a ready cart with emergency drugs. Our team is trained to use them quickly and correctly if needed.
Anticoagulation Management
Managing anticoagulation during surgery is complex. It’s a balance between preventing blood clots and avoiding too much bleeding.
We use anticoagulant medications carefully. We watch their effects closely to keep the patient safe.
Drug Safety Protocols
Strong drug safety protocols are vital during surgery. This includes checking medication orders, making sure labels are right, and watching for drug interactions.
“Safety is never an accident. It’s the result of careful planning, attention to detail, and a commitment to doing the right thing,” a medical safety expert says. We follow strict safety rules to avoid medication mistakes.
Patient Safety Measures During the Intraoperative Phase
Keeping patients safe during surgery is key. The intraoperative phase is a high-risk time. This is because of the surgery’s complexity, anesthesia, and the team involved.
Surgical Time-Out and Checklists
Surgical time-outs and checklists are vital. Time-outs pause the surgery to check the patient’s identity and the procedure. Checklists ensure all steps are followed before, during, and after surgery.
Infection Prevention Protocols
Preventing infections is a top priority. We use antibiotics, skin prep, and sterile techniques to lower the risk of surgical site infections (SSIs).
- Administering antibiotics before the incision
- Using antiseptic solutions for skin prep
- Ensuring sterile technique by all team members
Preventing Never Events
Never events are serious mistakes that should never happen. These include wrong-site surgery and medication errors. We have strict safety protocols to prevent these.
- Verifying patient identity and surgical site
- Using radiopaque markers for site identification
- Counting surgical instruments and sponges
Quality Assurance Measures
We ensure safety measures work through quality checks. This includes audits, staff feedback, and ongoing education on best practices.
“Quality is never an accident; it is always the result of high intention, sincere effort, intelligent direction, and skillful execution; it represents the wise choice of many alternatives.” – William A. Foster
Specialized Intraoperative Care for Different Surgical Specialties
Intraoperative care varies by surgical specialty. Each specialty has its own challenges and needs during surgery. This ensures the best care for patients.
Cardiac Surgery Considerations
Cardiac surgery is high-risk. Cardiopulmonary bypass is key, needing careful anticoagulation and temperature control. We also keep hemodynamic stability at its best.
- Monitoring cardiac function through transesophageal echocardiography (TEE)
- Managing anticoagulation to prevent thrombosis during cardiopulmonary bypass
- Maintaining optimal perfusion pressures
Neurosurgical Procedures
Neurosurgery needs precise care to protect the brain. We use electrophysiological monitoring to keep neural pathways safe.
“The use of intraoperative MRI has revolutionized neurosurgery, allowing for real-time assessment of tumor resection and reducing the risk of neurological damage.” –
A leading neurosurgeon
- Utilizing intraoperative imaging to guide surgical resection
- Maintaining optimal cerebral perfusion pressure
- Employing electrophysiological monitoring to protect neural function
Orthopedic Surgery Requirements
Orthopedic surgery is complex. We focus on patient positioning to avoid injury and ensure access.
- Using fluoroscopy to guide orthopedic procedures
- Managing blood loss through meticulous hemostasis
- Employing techniques to minimize infection risk
Obstetric and Gynecological Procedures
Obstetric and gynecological surgeries need careful care, with a focus on fetal monitoring and maternal stability.
- Monitoring fetal heart rate during obstetric surgery
- Managing maternal blood loss and fluid status
- Employing techniques to minimize the risk of complications
By tailoring care to each specialty, we improve patient outcomes and care quality.
Intraoperative Complications and Emergency Management
Managing intraoperative complications is key to keeping patients safe during surgery. We must be ready to tackle emergencies that can happen during surgery. These emergencies can greatly affect how well a patient does.
Hemorrhage Control
Hemorrhage is a big problem during surgery that needs quick action. Prompt recognition and intervention are vital to stop severe blood loss. We use surgical ligation and cauterization to stop bleeding.
The surgical team must work together to find and fix the bleeding source. Sometimes, hemostatic agents are used to help control bleeding.
Cardiac Emergencies
Cardiac emergencies during surgery are serious and need fast action. We watch patients closely for signs of heart trouble, like arrhythmias or ischemia. Advanced cardiac life support (ACLS) protocols are used when needed to handle these emergencies.
The anesthesiologist is key in managing heart emergencies by giving the right meds and keeping the heart working well. Close collaboration between the surgical and anesthesia teams is vital for good management.
Anesthetic Complications
Anesthetic complications can happen for many reasons, like anesthetic overdose or allergic reactions. We must watch closely to prevent these problems.
If an anesthetic complication happens, quick recognition and action are needed to keep the patient safe. This might mean changing the anesthetic or using reversal agents.
Crisis Resource Management
Crisis resource management is key in intraoperative emergencies. We stress the importance of effective communication and teamwork in crisis situations. This means clear roles, good info sharing, and making decisions together.
Our team gets ready for crises through training and simulation. This helps us respond well under pressure.
Conclusion: The Future of Intraoperative Care and Technology
Looking ahead, intraoperative care will be shaped by new technologies and practices. This evolution aims to better patient outcomes and improve care quality. It’s an exciting time for surgical management.
New tools like real-time monitoring and precision medicine are changing surgery. Technologies like artificial intelligence and robotics will also play big roles. These advancements promise to make surgeries safer and more precise.
Keeping healthcare professionals up-to-date is key. They need ongoing education to deliver top-notch care. As the field grows, so does the need for continuous learning.
The future of intraoperative care is bright. We’re ready to embrace new breakthroughs. Our goal is to provide the best healthcare, supporting patients from around the world.
FAQ
What does “intraoperative” mean in a medical context?
“Intraoperative” means during a surgery. It’s from when the patient gets ready for surgery to when it’s all done.
What are the three phases of surgical care?
Surgical care has three phases: before, during, and after surgery. Each phase needs special care and management.
What happens during the intraoperative period?
In the intraoperative period, the surgical team does the surgery. They give anesthesia, watch the patient’s health, and keep them safe and comfortable.
What is the role of the anesthesiologist during surgery?
The anesthesiologist gives anesthesia, checks the patient’s anesthesia level, and manages pain. They also watch the patient’s vital signs.
What are some common intraoperative monitoring techniques?
Common monitoring includes watching the heart, brain, and lungs. Advanced tech might also be used for safety.
How is patient safety maintained during the intraoperative phase?
Safety is kept up with time-outs, infection prevention, and quality checks. The team follows strict rules for medication and care.
What are some specialized intraoperative care considerations for different surgical specialties?
Specialties like cardiac, neuro, and orthopedic surgery need special care. This includes specific positioning, anesthesia, and monitoring.
How are intraoperative complications managed?
Complications like bleeding or heart issues are handled quickly. The team follows crisis management protocols.
What is the significance of proper patient positioning during surgery?
Right positioning is key for good surgery access and avoiding injuries. The team carefully positions the patient.
What are some emerging technologies in intraoperative care?
New tech includes MRI and CT scans during surgery and robotic surgery. These aim to improve results and precision.
How is medication administered during the intraoperative period?
Medication is managed by the anesthesia team and surgeons. They use antibiotics, emergency meds, and manage blood thinners safely.
What is the role of the surgical team during the intraoperative period?
The team, including surgeons and nurses, works together. They ensure the patient’s safety and the surgery’s success.
References
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6491077/









