Last Updated on November 26, 2025 by Bilal Hasdemir
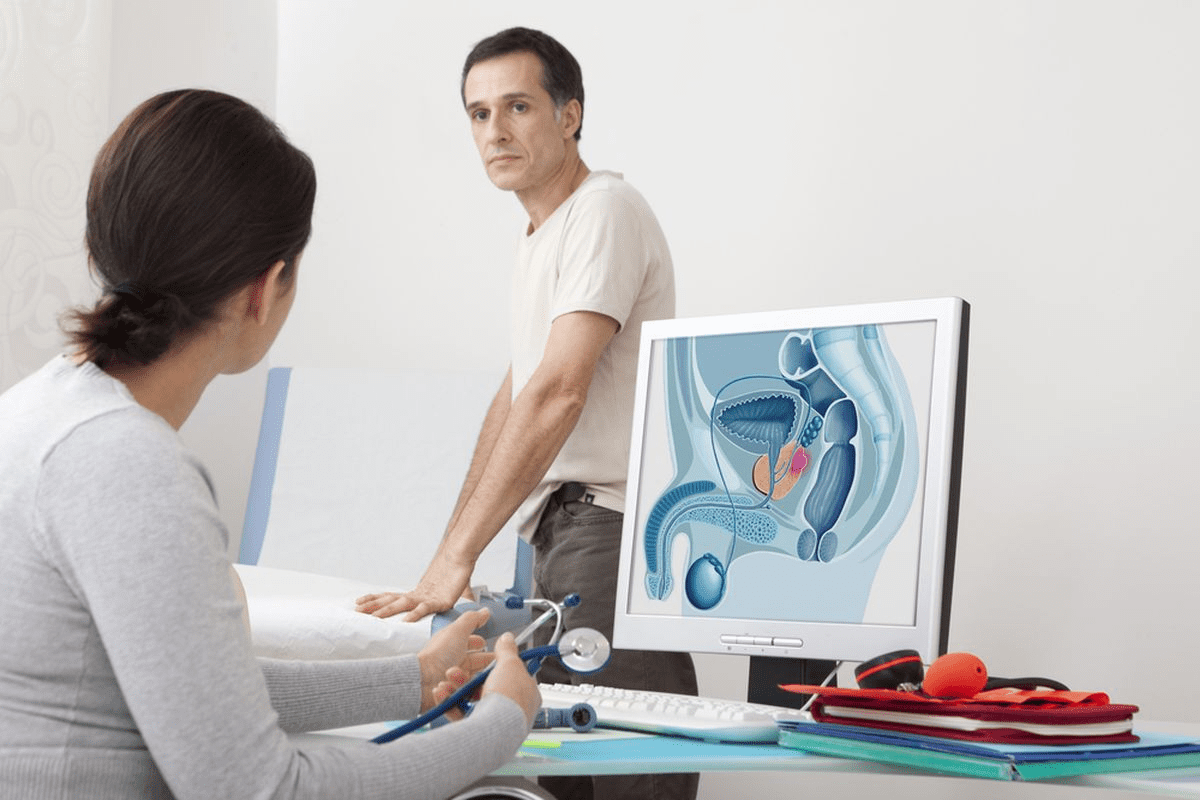
Interventional radiology (IR) is a special field of medicine. It uses advanced imaging for minimally invasive treatments. At Liv Hospitals, we use IR to give patients the latest care. This helps them recover faster and get better results.
IR procedures are key in today’s healthcare. They help diagnose and treat many medical issues. Knowing the most common IR procedures is vital for both patients and doctors.
In this article, we’ll look at the top 12 IR procedures. We’ll talk about why they’re important and their benefits. By diving into these procedures, we hope to show how IR improves patient care.
Key Takeaways
- Interventional radiology is a specialized field that uses advanced imaging for minimally invasive treatments.
- IR procedures are critical in modern healthcare for diagnosis and treatment.
- The top 12 IR procedures will be discussed, highlighting their significance and benefits.
- Liv Hospitals uses IR to provide cutting-edge care and improve patient outcomes.
- Understanding IR procedures is essential for patients and healthcare professionals.
Understanding Interventional Radiology: Beyond Diagnostic Imaging
Interventional radiology is more than just imaging. It’s a key part of treating many health issues with great precision and quick recovery times. This field has grown a lot, giving new ways to help patients who need more than just imaging tests.
What Is Interventional Radiology?
Interventional radiology uses imaging to guide small, non-surgical procedures. Interventional radiologists perform many treatments, like fixing blood vessels and taking biopsies. They use live images to find and treat problems inside the body.
The Evolution of Interventional Radiology
Interventional radiology has changed a lot in recent years. New imaging tech and medical tools have made it possible to treat more conditions. Now, patients often get better faster and with fewer side effects than with old surgery methods.
At first, radiology was just for looking at images. But as tech improved, it became clear that imaging could also help treat problems. Now, interventional radiology is a big part of medicine, giving minimally invasive options instead of surgery for many people.
IR vs OR: Minimally Invasive Alternatives to Surgery
Interventional radiology (IR) and traditional surgery (OR) are different in how invasive they are. IR uses tiny holes or natural openings, while surgery needs bigger cuts. This makes IR better for patients, with less pain, quicker healing, and fewer risks.
| Characteristics | Interventional Radiology (IR) | Operating Room (OR) Surgery |
| Invasiveness | Minimally invasive, small punctures or natural orifices | More invasive, larger incisions |
| Recovery Time | Generally shorter recovery period | Longer recovery period |
| Pain and Discomfort | Less pain and discomfort | More pain and discomfort |
| Risk of Complications | Lower risk of complications | Higher risk of complications |
It’s important to know the differences between IR and surgery. This helps both patients and doctors make better choices. By understanding IR, we can pick the best treatment for many health problems.
Interventional Radiologist vs. Diagnostic Radiologist: Key Differences
It’s important to know the differences between interventional and diagnostic radiologists. They both play key roles in healthcare, but they have different jobs and training. This knowledge helps patients choose the right care.
Role and Responsibilities
Interventional radiologists use imaging to guide treatments. They do things like angioplasty and tumor ablation. On the other hand, diagnostic radiologists look at images like X-rays and MRIs to find diseases.
Key Responsibilities:
- Interventional Radiologist: They do procedures that need exact imaging.
- Diagnostic Radiologist: They figure out what images show.
Training Requirements and Career Path
Getting to be an interventional radiologist takes more time. First, they go to medical school. Then, they do a residency in radiology and a fellowship in interventional radiology. This training lasts about 6-7 years after medical school.
Training Timeline:
| Stage | Duration | Description |
| Medical School | 4 years | Basic medical education |
| Diagnostic Radiology Residency | 4 years | Specialized training in radiology |
| Interventional Radiology Fellowship | 1-2 years | Advanced training in interventional procedures |
Day-to-Day Practice Differences
Interventional radiologists do procedures and see patients directly. They use imaging to guide their work. Diagnostic radiologists mostly look at images and write reports for other doctors.
In summary, interventional and diagnostic radiologists are both vital in healthcare. They have different jobs, training, and daily tasks. Knowing these differences helps us understand the complexity of modern medicine.
Becoming an Interventional Radiological Procedure
The path to becoming an interventional radiological procedure is complex. It involves technology, medical skills, and caring for patients. We see a big change in medical treatments, with interventional radiology leading the way.
These procedures are designed to be small and less invasive. They often avoid the need for big surgeries. This makes patients recover faster and improves their care quality.
To see how a procedure becomes part of interventional radiology, we look at several things. These include new technology, research, and training for doctors and nurses.
New procedures in interventional radiology come from better imaging and tools. For example, better ultrasound and MRI help with more precise treatments.
| Procedure | Description | Benefits |
| Angiography | Visualizing blood vessels | Diagnoses vascular conditions |
| Angioplasty | Opening blocked vessels | Restores blood flow |
| Embolization | Controlling bleeding | Reduces risk of hemorrhage |
As we keep improving interventional radiology, we must focus on safety and success. This means thorough testing and training. We want new procedures to work well and be safe.
By moving forward with these advancements, we can better care for patients. This makes interventional radiology a key part of today’s medicine.
Becoming an Interventional Radiologist: Training Path and Competitiveness
Starting a career as an interventional radiologist is a complex journey. It requires education, training, and a lot of commitment. This field is always changing with new medical technology. It’s a challenging but rewarding path for those who love minimally invasive procedures.
Educational Requirements and Timeline
To become an interventional radiologist, you need a lot of education and training. Here’s what you typically need to do:
- Get a bachelor’s degree in a science field.
- Go to medical school to get an M.D. or D.O. degree.
- Do a residency in diagnostic radiology.
- Maybe do a fellowship in interventional radiology.
This journey can take over 10 years. It’s very competitive because of the tough selection for residency and fellowship programs.
| Stage | Duration | Description |
| Bachelor’s Degree | 4 years | Typically in a science-related field. |
| Medical School | 4 years | Earns an M.D. or D.O. degree. |
| Diagnostic Radiology Residency | 4-5 years | Provides foundational training in radiology. |
| Interventional Radiology Fellowship | 1-2 years | Specialized training in interventional radiology. |
How Competitive Is Interventional Radiology?
Interventional radiology is getting more competitive. This is because it’s in high demand and offers a unique approach. It attracts skilled people because of its technology and lifestyle benefits.
What makes it competitive includes:
- Advancements in technology.
- More demand for less invasive procedures.
- Perceived better work-life balance compared to other specialties.
Interventional Radiology Lifestyle Considerations
The lifestyle of an interventional radiologist is demanding but rewarding. The work is intense, but many enjoy the balance it offers.
Things to consider about the lifestyle:
- Potential for irregular hours, including nights and being on call.
- Need to keep up with new technologies and techniques.
- Chance for a better work-life balance than traditional surgery.
In summary, a career in interventional radiology is a mix of medical challenge, technology, and personal fulfillment. It’s a great choice for many medical professionals.
Comprehensive IR Procedures List: The 12 Most Common Interventional Techniques
Interventional Radiology (IR) has changed medical procedures by providing new, less invasive options. These techniques are making a big difference in how we care for patients.
IR procedures are very different from old-school surgery. Minimally invasive approaches use tiny incisions. This is unlike traditional surgery, which needs bigger cuts.
How IR Procedures Differ from Traditional Surgery
IR procedures are less invasive than traditional surgery. This means less tissue damage and less pain for the patient. It also leads to quicker recovery times.
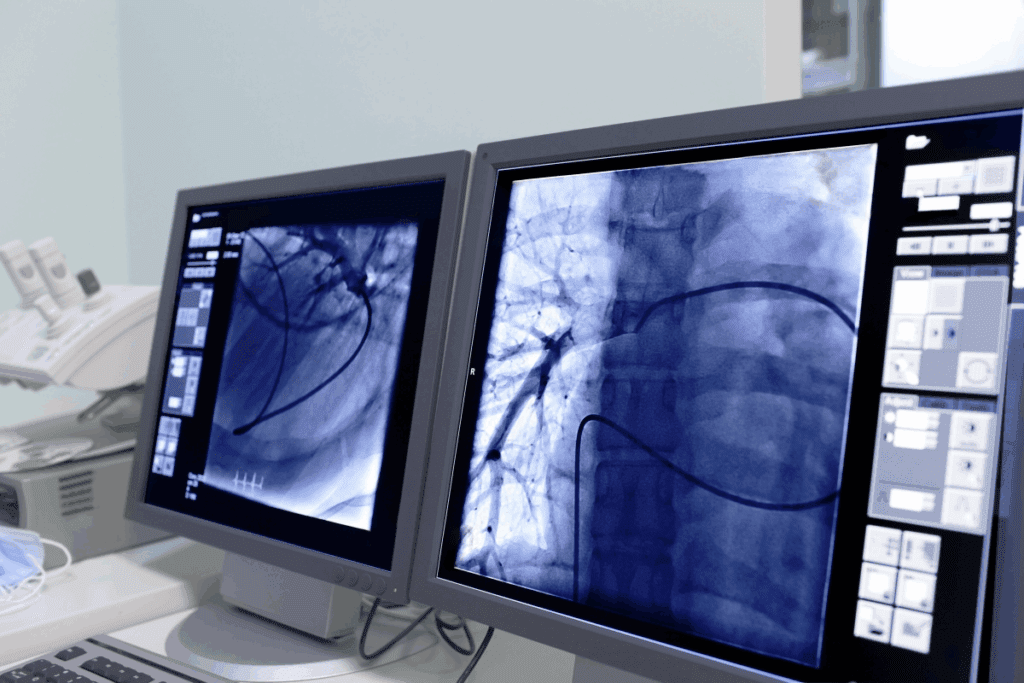
Another big difference is the use of image guidance. Tools like fluoroscopy and MRI help doctors see what they’re doing in real-time. This precision is hard to match with traditional surgery.
Benefits of Minimally Invasive Approaches
IR procedures have many benefits. Patients usually feel less pain and stay in the hospital less time. They also face fewer complications, which is great for those at high risk for surgery problems.
IR procedures can also target treatments more accurately. For example, they can treat tumors directly, sparing healthy tissues. This can lead to better results and fewer side effects.
Looking at the top 12 IR procedures, it’s clear they’re making a big impact. These techniques offer a less invasive option for many medical conditions. They’re changing medicine and improving patient care.
Vascular IR Procedures
Vascular IR procedures are key in modern medicine. They offer safe, non-invasive treatments for many vascular issues. These methods have changed how we treat vascular diseases, making them safer than old surgery methods.
1. Angiography: Visualizing Blood Vessels
Angiography lets us see inside blood vessels. We use a contrast agent to spot problems like blockages. This tool is vital for planning treatments.
Key benefits of angiography include:
- Accurate diagnosis of vascular conditions
- Guiding interventional procedures
- Minimally invasive, reducing patient risk
2. Angioplasty and Stenting: Opening Blocked Vessels
Angioplasty and stenting open blocked blood vessels. A balloon is used to widen the vessel, and a stent keeps it open. This method is often used for peripheral artery disease.
The advantages of angioplasty and stenting include:
- Improved blood flow to affected areas
- Reduced symptoms such as pain and cramping
- Minimal recovery time compared to surgical alternatives
3. Embolization: Controlling Bleeding and Blocking Abnormal Vessels
Embolization blocks or reduces blood flow to specific areas. It’s used to stop bleeding, manage tumors, or treat vascular malformations. By blocking blood vessels, we can treat various conditions without surgery.
Embolization benefits include:
- Effective control of bleeding
- Minimally invasive treatment of vascular malformations
- Reduced risk of complications compared to traditional surgery
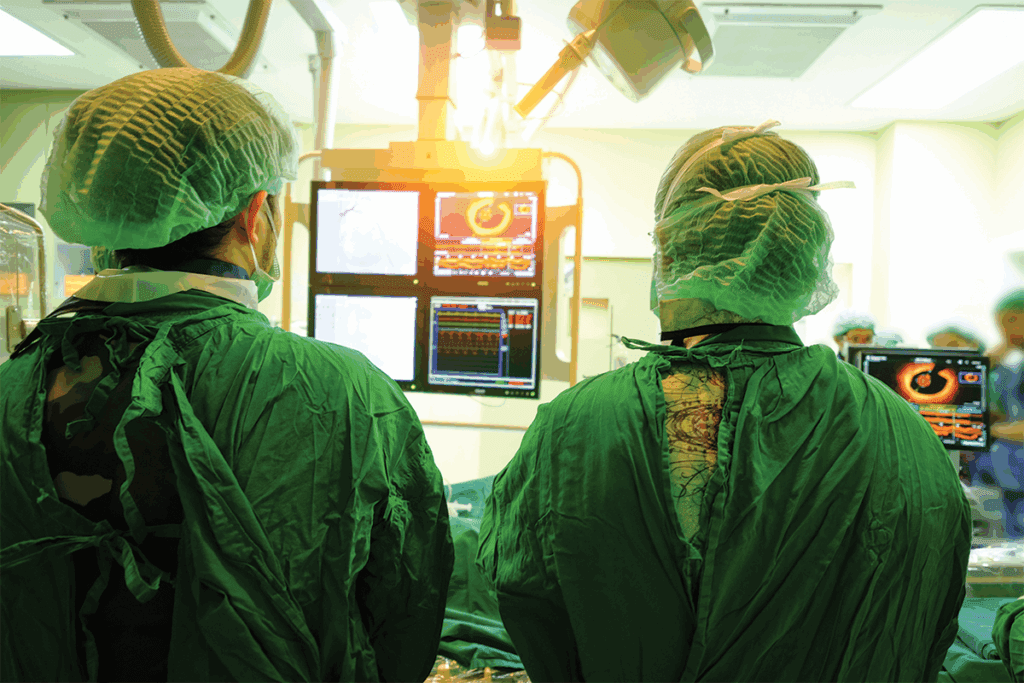
Interventional Oncology Procedures
Interventional oncology is a key part of cancer care today. It focuses on using less invasive methods to treat cancer. These methods aim to target cancer cells directly, protecting healthy tissues.
Tumor Ablation: Destroying Cancer Cells
Tumor ablation uses heat or chemicals to kill cancer cells. It’s great for tumors that can’t be removed by surgery. We use imaging to find the tumor and apply the right treatment, like radiofrequency ablation (RFA) or cryoablation.
This method has many benefits. It means less recovery time and fewer risks. It’s also good for patients who can’t have other treatments. Tumor ablation works on cancers in the liver, kidney, and lungs.
Chemoembolization and Radioembolization: Targeted Cancer Therapy
Chemoembolization and radioembolization deliver treatment right to the tumor. Chemoembolization injects chemotherapy drugs into the tumor’s blood vessels and then blocks them. This makes the treatment more effective and reduces side effects.
Radioembolization uses tiny radioactive beads in the tumor’s arteries. These beads give a high dose of radiation to the tumor, but not to healthy tissue. Both methods are used for liver cancer and metastases.
Port and Catheter Placement for Chemotherapy
For chemotherapy, ports and catheters are essential. We use radiology to place these devices. They make it easier and safer to get chemotherapy drugs.
These devices are placed under imaging, ensuring they’re in the right spot. This makes treatment more comfortable and less invasive for patients.
Drainage and Fluid Collection Procedures
Drainage procedures, like abscess drainage and nephrostomy, are key in treating infections and other issues. These methods are less invasive and help manage fluid collections and abscesses. This reduces the need for surgery.
7. Abscess Drainage: Treating Infections
Abscess drainage treats abscesses, which are pus collections in the body. Draining the abscess helps get rid of the infection and aids in healing.
The process includes:
- Using imaging to find the abscess
- Inserting a needle or catheter into the abscess
- Draining the pus and possibly leaving a catheter for more drainage
This procedure is done under local anesthesia. It cuts down on recovery time compared to surgery.
8. Biliary Procedures: Managing Liver and Gallbladder Issues
Biliary procedures manage bile duct issues like obstructions or infections. They help restore bile flow, easing symptoms and preventing complications.
Some common procedures are:
- Biliary drainage: relieving bile duct obstructions
- Stent placement: keeping bile ducts open
- Balloon dilation: widening narrowed bile ducts
These methods are important for liver or gallbladder problems. They offer a less invasive option than surgery.
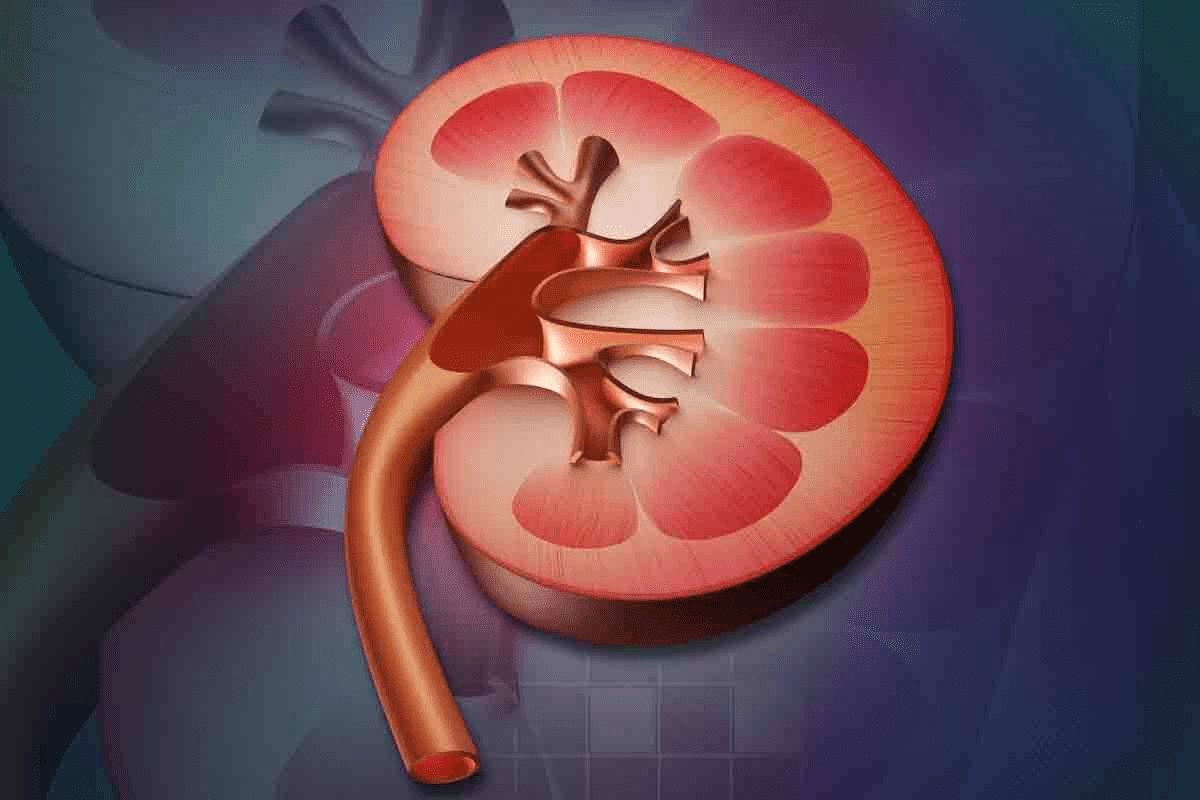
9. Nephrostomy: Kidney Drainage Techniques
Nephrostomy creates a urine drainage path from the kidney when there’s a blockage. It’s essential for relieving pressure and preventing kidney damage.
The steps for a nephrostomy are:
- Imaging to access the kidney
- Insertion of a catheter or nephrostomy tube
- Drainage of urine from the kidney
By doing a nephrostomy, we can help the kidney work normally again and ease symptoms.
Biopsy and Specialized IR Procedures
We use advanced biopsy and IR procedures to improve patient care. These methods help diagnose and treat many health issues. With imaging tech, we do these procedures with great precision and low risk to the patient.
Image-Guided Tissue Sampling
Image-guided biopsy uses ultrasound, CT, or MRI to guide the needle. This way, we can get accurate tissue samples. It’s great for diagnosing cancer, infections, and more.
The benefits are clear:
- Precision: We get the tissue sample from the right spot.
- Minimally invasive: It’s less painful and risky than old-school biopsies.
- Quick recovery: Patients can get back to normal fast.
Venous Access Procedures: Central Lines and Ports
Venous access is key for long-term medication or nutrition. Central lines and ports make it safe and easy.
Here’s what’s important:
- Central Lines: Catheters in big veins for treatment.
- Ports: Implantable for long-term access, fewer needle sticks.
- Image guidance: Imaging tech for accurate placement and fewer problems.
Image-guided sampling and venous access improve patient results. These IR procedures show how vital interventional radiology is in healthcare today.
Pain Management and Spine Interventions
Modern medicine has moved towards less invasive spine treatments for pain. We now offer many effective treatments. These not only ease pain but also improve life quality for our patients.
Vertebroplasty and Kyphoplasty: Treating Spinal Fractures
Vertebroplasty and kyphoplasty treat spinal compression fractures. These methods inject bone cement into the vertebra to stabilize it and lessen pain.
Vertebroplasty injects bone cement directly into the fractured vertebra. It offers quick pain relief and stabilizes the fracture.
Kyphoplasty is similar but first creates a cavity in the vertebra with a balloon. Then, it fills this cavity with bone cement. Kyphoplasty can also help restore some lost vertebra height.
Advanced Pain Management Techniques
There are more advanced pain management options. These include:
- Nerve blocks: Injecting medication into specific nerves to block pain signals.
- Spinal cord stimulation: Implanting a device that sends electrical impulses to the spinal cord to reduce pain.
- Radiofrequency ablation: Using heat from radio waves to lesion specific nerves and reduce pain.
Patient Selection and Outcomes
Choosing the right patient is key for spine intervention success. We evaluate each patient’s condition, medical history, and health to find the best treatment.
| Procedure | Success Rate | Recovery Time |
| Vertebroplasty | 80-90% | 1-3 days |
| Kyphoplasty | 85-95% | 1-3 days |
| Nerve Blocks | 70-80% | Immediate |
By choosing the right patients and using the best techniques, we see big improvements in pain management and life quality.
Conclusion: The Future of Interventional Radiology
Interventional radiology (IR) is on the verge of big changes. New technologies and techniques are coming. These will make patient care even better.
IR is changing how we treat complex health issues. Thanks to better imaging and less invasive methods, IR’s role in medicine is growing. We’ll see IR play a bigger part in treating diseases, helping patients recover faster.
Research and teamwork among healthcare experts are driving IR’s growth. As we look ahead, IR will likely be key in treating vascular diseases and cancer. By embracing these advancements, we can offer top-notch care to our patients.
FAQ
What is the difference between interventional radiology and diagnostic radiology?
Interventional radiology uses imaging to guide procedures. Diagnostic radiology looks at images to find medical issues.
How long does it take to become an interventional radiologist?
It takes 13-15 years after high school. This includes medical school, residency, and fellowship.
Is interventional radiology competitive?
Yes, it’s very competitive. There are only a few spots for fellowship each year.
What is the lifestyle like for an interventional radiologist?
They work long hours, including nights and weekends. But, some have more regular hours.
Do interventional radiologists perform surgery?
No, they do not. They do minimally invasive procedures, not open surgery.
What are the benefits of minimally invasive IR procedures?
These procedures have small incisions and less pain. They also have shorter recovery times and lower risks.
What is the role of an interventional radiologist in cancer treatment?
They use procedures like tumor ablation to help manage cancer. This is a key part of cancer treatment.
What is the difference between IR and OR?
IR is minimally invasive procedures under imaging. OR is traditional surgery in a sterile environment.
Do radiologists work weekends?
Some, like interventional radiologists, may work weekends. It depends on their job and setting.
What is diagnostic radiology?
It’s a field that uses images to diagnose and manage health issues. This includes X-rays and MRI scans.
What is IR doctor meaning?
An IR doctor specializes in minimally invasive procedures. They use imaging to guide these procedures.
What does IR stand for in medical terms?
IR stands for interventional radiology. It’s a field that uses imaging for minimally invasive procedures.
References
Majumdar, A., et al. (2024). Current trends in herbal medicines targeting renal cell carcinoma. Phytomedicine, 131, 152837. https://www.sciencedirect.com/science/article/abs/pii/S2950199724001174