Endometriosis is a chronic condition that affects about 10% of women of reproductive age worldwide. It has big health and quality of life implications. It’s important to understand this condition, which impacts around 190 million women globally.is endometriosis dangerousWhat is commonly mistaken for ovarian cancer?
A lot of women face severe symptoms, like intense menstrual pain and trouble getting pregnant. These symptoms can deeply affect their well-being. We need to talk about the dangers of endometriosis and the risks and complications it can bring.
We will look into how common endometriosis is, its symptoms, and possible complications. Our goal is to give you a full picture of endometriosis and its effects on women’s health.
Key Takeaways
- Endometriosis affects about 10% of women of reproductive age worldwide.
- The condition can cause significant health and quality-of-life issues.
- Debilitating symptoms include severe menstrual pain and infertility challenges.
- Understanding the risks and possible complications is key for those affected.
- Healthcare providers play a vital role in managing and treating the condition.
Understanding Endometriosis: A Chronic Condition
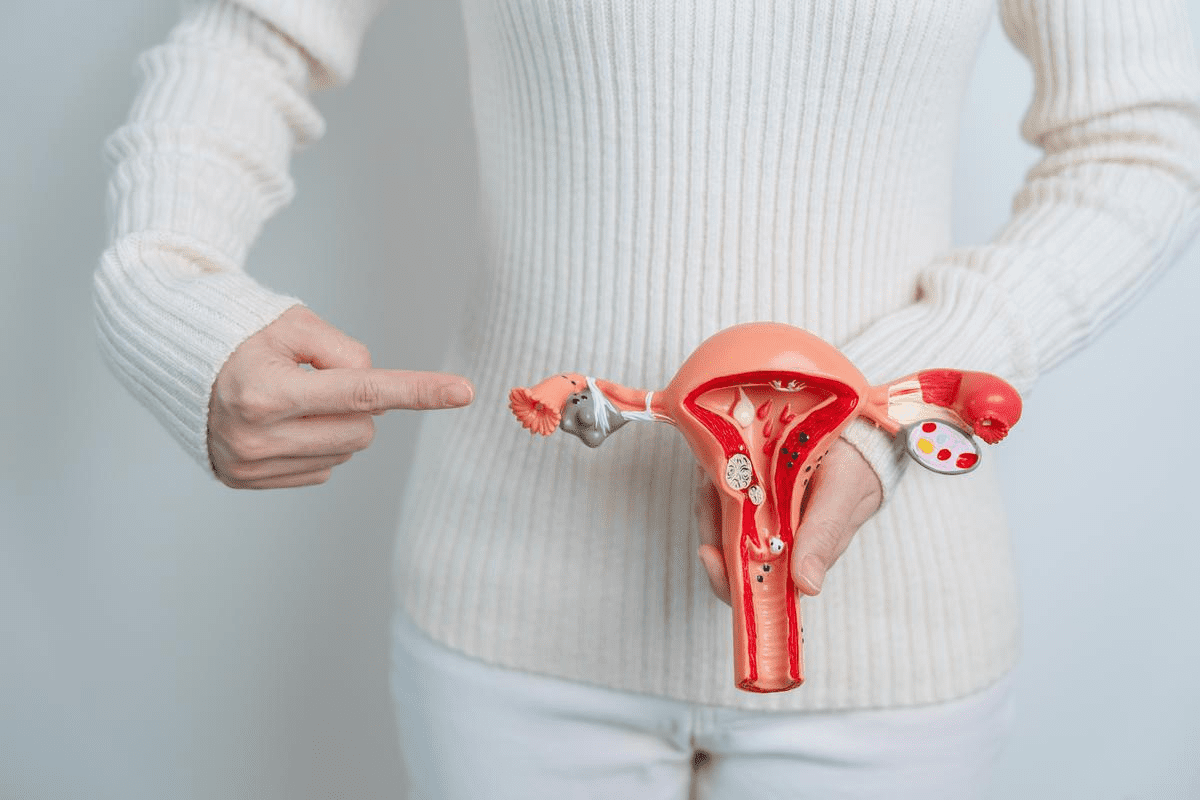
Endometriosis is when tissue like the uterus lining grows outside the uterus. It’s a chronic condition that affects millions of women worldwide. It causes a lot of discomfort and health problems.
We will dive into the details of endometriosis. This includes its definition, types, and stages. We aim to give a clear picture of this complex condition.
What Happens in Endometriosis
In endometriosis, tissue like the uterus lining grows outside the uterus. This leads to inflammation, scar tissue, and adhesions. This misplaced tissue, known as endometrial implants, can be found on the ovaries, fallopian tubes, and other pelvic structures.
The growth of this tissue is influenced by hormonal changes during the menstrual cycle. It thickens, breaks down, and bleeds. But, it can’t exit the body, causing inflammation and pain.
Types and Stages of Endometriosis
Endometriosis can be classified into different types based on where and how deep the endometrial implants are. The main types include:
- Superficial Peritoneal Endometriosis: This type involves the growth of endometrial tissue on the peritoneal surface.
- Deep Infiltrating Endometriosis: Characterized by deep invasion of endometrial tissue into the underlying tissue or organs.
- Ovarian Endometrioma: Also known as “chocolate cysts,” these are cysts filled with old blood, giving them a characteristic appearance.
The stages of endometriosis range from minimal to severe. The Revised American Society for Reproductive Medicine (rASRM) classification system is commonly used to stage endometriosis.
Stage | Description |
Stage I (Minimal) | Isolated implants without significant adhesions. |
Stage II (Mild) | More extensive implants with some adhesions. |
Stage III (Moderate) | Multiple implants with more pronounced adhesions. |
Stage IV (Severe) | Extensive implants with dense adhesions and significant organ involvement. |
“Understanding the different types and stages of endometriosis is key. It helps in developing effective treatment plans and improving the quality of life for women with this condition.”
The Global Impact: Endometriosis Statistics
Understanding the global impact of endometriosis requires looking at the statistics. These numbers show how widespread and impactful it is. It affects a lot of women, mainly those of reproductive age.
About 190 million women worldwide have endometriosis. This makes it a big public health issue. It shows we need more awareness, better management, and support for those affected.
Prevalence Among Women of Reproductive Age
Endometriosis mostly hits women in their reproductive years. It’s most common in women aged 25 to 35. Research says about 1 in 10 women of reproductive age have it.
This shows how critical early diagnosis and treatment are. They help manage symptoms and improve life quality.
Endometriosis in Women with Chronic Pelvic Pain and Infertility
Endometriosis is common in women with chronic pelvic pain and infertility. Studies show many women with these issues have endometriosis. This shows a strong link between endometriosis and these symptoms.
Key statistics include:
- Up to 50% of women with chronic pelvic pain have endometriosis.
- Endometriosis is found in about 25-50% of infertile women.
These numbers highlight the importance of considering endometriosis when diagnosing women with chronic pelvic pain and infertility. This helps in providing timely and proper care.
Is Endometriosis Dangerous? Addressing the Main Concern
It’s important to know the risks of endometriosis to manage it well. While it’s not usually life-threatening, it can cause serious health problems if not treated right.
Physical Health Risks
Endometriosis can lead to chronic pain, heavy or irregular periods, and infertility. These symptoms can really affect your daily life and well-being.
Common Physical Health Risks:
- Chronic pelvic pain
- Heavy or prolonged menstrual bleeding
- Infertility or difficulty conceiving
- Ovarian cysts or endometriomas
- Adhesions or scar tissue in the pelvis
Quality of Life Impact
Endometriosis can really change your life. Chronic pain and symptoms can make it hard to do everyday things. They can also affect your mental health and relationships.
The emotional toll of endometriosis should not be underestimated. Many people feel anxious, depressed, and isolated because of it.
Aspect of Life | Impact of Endometriosis |
Physical Activities | Chronic pain can limit exercise and daily activities |
Mental Health | Increased risk of anxiety and depression |
Social Life | Symptoms can cause isolation and affect relationships |
Long-term Health Implications
Endometriosis can lead to long-term health problems. It’s important to know these risks to manage your health over time.
Potential Long-term Health Implications:
- Increased risk of ovarian cancer
- Potential links to autoimmune disorders
- Impact on mental health over time
- Possible effects on cardiovascular health
Understanding the risks of endometriosis helps you deal with its challenges. It also helps you find the right care for your condition.
Recognizing the Symptoms of Endometriosis
It’s important to know the symptoms of endometriosis early. This helps in getting the right treatment. Endometriosis can make a woman’s life harder in many ways.
Common Pain Symptoms
Pain is a big symptom of endometriosis. It can show up in different ways:
- Severe menstrual pain that can really hurt and stop you from doing things you need to do.
- Chronic pelvic pain that doesn’t just happen during your period but all the time.
- Painful intercourse, which can make things hard in your relationship.
Menstrual Irregularities
Endometriosis also causes problems with your period. You might see:
- Heavy or prolonged menstrual bleeding, which can make you feel tired or weak.
- Irregular periods, where your cycle is off or lasts too long.
Non-Pain Symptoms and Warning Signs
There are other signs of endometriosis too. These include:
- Digestive issues, like bloating, constipation, or diarrhea, mostly when you’re on your period.
- Fatigue, caused by constant pain, heavy bleeding, or other endometriosis-related issues.
- Infertility or trouble getting pregnant, a big worry for many women with endometriosis.
Spotting these symptoms early can help you get the right help. This can make a big difference for women with endometriosis.
The Diagnostic Journey: Challenges and Approaches
Getting a diagnosis for endometriosis can be tough. It’s because the symptoms are not clear-cut. This makes the journey to find out what’s wrong long and hard. You might see many doctors and go through several tests.
Why Diagnosis Is Often Delayed
It’s hard to get a diagnosis because the symptoms are similar to other health issues. Lack of awareness among both patients and doctors makes it even harder.
The symptoms of endometriosis, like pelvic pain and irregular periods, can look like other problems. This makes it tough to figure out what’s really going on.
Diagnostic Methods and Tests
There are different ways to find out if you have endometriosis. These include:
- Pelvic exams to check for any unusual findings
- Imaging tests like ultrasound and MRI
- Laparoscopy, a surgery that lets doctors see inside the pelvis
Laparoscopy is the best way to diagnose endometriosis. It lets doctors see and take a sample of the affected areas.
Questions to Ask Your Doctor
It’s important to ask your doctor questions when you’re trying to get a diagnosis. Some good questions are:
- What could be causing my symptoms?
- What tests do you suggest I have?
- What happens next if I do have endometriosis?
Knowing about the diagnostic process and the tests available helps. It makes it easier to deal with the challenges of getting a diagnosis for endometriosis.
Complications Associated with Endometriosis
Endometriosis can lead to many complications that affect a woman’s life. These issues can touch on fertility, pregnancy, and even increase cancer risk. They also impact the urinary and gastrointestinal systems.
Fertility Issues and Pregnancy Complications
Women with endometriosis often struggle with infertility. This is because the condition can cause adhesions and scar tissue. These can make it hard for sperm to reach the egg or for a fertilized egg to implant.
Even if pregnancy happens, women with endometriosis face higher risks of pregnancy complications. These can include preterm labor, placenta previa, and gestational hypertension. A study showed that these risks are higher, making it important to closely monitor pregnancies.
“Women with endometriosis are at a higher risk for pregnancy complications, and their pregnancies should be considered high-risk.”
Urinary and Gastrointestinal Disorders
Endometriosis can also cause urinary disorders. For example, it can affect the bladder or ureters. This can lead to painful urination or blood in the urine.
When endometriosis involves the bowel, it can cause gastrointestinal disorders. Symptoms may include constipation, diarrhea, or even bowel obstruction. These issues can greatly affect a woman’s quality of life and need special care.
Cancer Risk: Understanding the Connection
There’s evidence that endometriosis may raise the risk of certain cancers, like ovarian cancer. The exact reason is not clear, but chronic inflammation and hormonal changes might play a part.
A meta-analysis showed a slightly higher risk of ovarian cancer in women with endometriosis. This highlights the need for better awareness and possibly more cancer screening for this group.
It’s key to understand these complications to manage endometriosis well. By knowing the risks and working with healthcare providers, women can improve their health outcomes.
Treatment Options for Managing Endometriosis
The goal of treating endometriosis is to control symptoms and prevent long-term damage. This is done through a mix of medical and surgical methods. Each treatment plan is made to fit the person’s needs and how severe their condition is.
Pain Management Medications
Managing pain is key in treating endometriosis. Over-the-counter pain relievers like ibuprofen can help with mild to moderate pain. For more severe pain, doctors might prescribe stronger medications.
Other medications can also help manage symptoms. Hormonal treatments, for example, can stop menstrual bleeding. This can reduce pain and other symptoms of endometriosis.
Hormone Therapy
Hormone therapy is a big part of treating endometriosis. It works by lowering estrogen levels. This slows down the growth of endometrial tissue and eases symptoms. Treatments include birth control pills, hormonal IUDs, and GnRH agonists.
These therapies can help manage symptoms and are often used together with other treatments. But, they can have side effects. Always talk to a healthcare provider before starting hormone therapy.
Surgical Interventions
For some, surgery is needed to manage endometriosis. Laparoscopic surgery is common. It removes endometrial lesions with less recovery time. In severe cases or when other treatments fail, more extensive surgery might be needed.
Discussing surgery options with a healthcare provider is important. It’s about weighing the benefits and risks. Surgery can help some women, but it’s not a cure, and symptoms can come back.
In summary, treating endometriosis well needs a full approach. This includes pain meds, hormone therapy, and sometimes surgery. By knowing the treatment options, women can work with their doctors to find a plan that suits them best. This improves their quality of life.
Living with Endometriosis: Coping Strategies
Coping with endometriosis is more than just medical treatment. It’s about a whole approach. People with endometriosis need various strategies to manage their daily lives. These include physical techniques, emotional support, and lifestyle changes.
Physical Coping Techniques
Physical coping methods are key in managing endometriosis symptoms. Pain management is a big part of it. Healthcare experts say exercise is great for chronic pain.
Gentle exercises like yoga and swimming can help. They reduce pain and boost well-being.
Other physical methods include heat therapy, physical therapy, and acupuncture. These can lessen pain and enhance life quality.
Emotional and Psychological Support
Emotional and psychological support is essential for those with endometriosis. The condition can make people feel isolated and frustrated. Support groups, online or in-person, offer a sense of belonging.
Counseling or therapy can also help. Techniques like cognitive-behavioral therapy (CBT) can improve mental health.
Lifestyle Modifications and Complementary Therapies
Lifestyle changes are important in managing endometriosis. Eating an anti-inflammatory diet can help symptoms. Nutritional supplements like omega-3 fatty acids are also beneficial.
- Avoiding foods that trigger or worsen symptoms
- Adding stress-reducing activities like meditation or mindfulness
- Ensuring enough sleep and maintaining a healthy weight
Complementary therapies like herbal remedies and mind-body therapies are options. But, always talk to a healthcare provider before trying new therapies.
Myths and Misconceptions About Endometriosis
Endometriosis is misunderstood by many, despite its commonality. These myths can change how people see the condition and the help they get. We want to clear up these misconceptions with facts, helping to raise awareness and support for those with endometriosis.
Common Misunderstandings
Many myths surround endometriosis, leading to confusion. Some common misconceptions include:
- Endometriosis is just a painful period: Many think it’s only about painful menstruation. But it’s more complex, involving hormones, immunity, and body structure.
- It’s a rare condition: Actually, it affects a lot of women of childbearing age, making it more common than thought.
- There’s a simple cure: Sadly, there’s no single cure for endometriosis. Treatment varies, depending on the person’s needs.
Evidence-Based Facts
To fight these myths, we need to focus on proven facts. Here are some important truths about endometriosis:
Myth | Fact |
Endometriosis only affects women during their menstrual years. | While it’s more common during reproductive years, symptoms can persist after menopause, and it can also affect younger girls. |
Endometriosis is caused by poor lifestyle choices. | Research shows it’s influenced by genetics, hormones, and environment, not just lifestyle. |
Surgery is the only effective treatment. | Treatment plans vary and can include medication, lifestyle changes, and surgery, depending on the severity and individual needs. |
By knowing the facts and debunking myths, we can better support those with endometriosis. Awareness and accurate info are key to improving their lives.
Conclusion: Navigating Life with Endometriosis
Living with endometriosis needs a full plan that includes good management and strong support. Knowing about the condition helps people deal with it better. This way, they can live a better life.
It’s tough to live with endometriosis, but the right help makes a big difference. We stress the need for support from doctors, groups, or family. This support is key to handling the condition.
Managing endometriosis well means using many strategies. This includes medical care, changing your lifestyle, and getting emotional support. By using these methods, people can lessen the condition’s effects on their life and health.
FAQ
What is endometriosis and how does it affect women?
Endometriosis is a chronic condition where tissue like the uterus lining grows outside it. This causes pain, discomfort, and symptoms in millions of women, mainly those of reproductive age.
What are the common symptoms of endometriosis?
Symptoms include pelvic pain, irregular periods, heavy or irregular bleeding, and painful sex. Recognizing these symptoms is key for early diagnosis and treatment.
How prevalent is endometriosis among women?
It affects a significant number of women worldwide. About 10% of women of reproductive age have it, though the real number might be higher due to underdiagnosis.
Is endometriosis a dangerous condition?
Endometriosis is not usually life-threatening but can greatly affect a woman’s life. It can lead to fertility issues, urinary and gastrointestinal problems, and may increase cancer risk.
How is endometriosis diagnosed?
Diagnosing endometriosis is tough and often requires a mix of medical history, physical exams, imaging tests, and sometimes laparoscopy. Knowing the diagnostic process helps in understanding the journey to diagnosis.
What are the treatment options for managing endometriosis?
Treatments include pain meds, hormone therapy, and surgery. These aim to reduce symptoms, improve life quality, and address related issues.
Can endometriosis be cured?
There’s no definitive cure for endometriosis yet. But treatments and coping strategies can manage the condition, lessen symptoms, and enhance well-being.
How does endometriosis impact fertility?
Endometriosis can affect fertility in some women, making it harder to conceive. Knowing this is important for those wanting to start a family.
Are there any lifestyle changes that can help manage endometriosis?
Yes, making dietary changes, exercising, managing stress, and trying complementary therapies can help alleviate symptoms and improve life quality for those with endometriosis.
What are some common myths about endometriosis?
Myths include thinking endometriosis is normal, only causes menstrual cramps, or is rare. Facts show it’s a serious health issue needing awareness and proper management.
How can individuals cope with the emotional and psychological impact of endometriosis?
Coping involves seeking support from healthcare providers, support groups, and loved ones. Stress management and lifestyle adjustments also help improve overall well-being.
References
National Center for Biotechnology Information. Endometriosis: Severity of Period Pain. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC7573391/