What is the approach to pediatric thrombocytopenia? Learn the crucial diagnostic steps for ITP in pediatrics. Powerful knowledge for accurate identification and care.
Pediatric thrombocytopenia is when kids have too few platelets. This can cause bleeding or bruising. It’s important to understand this condition well. A platelet count below 150,000/microL is what defines it. It might be noticed if a child bruises easily or bleeds a lot.
It can also pop up during routine tests for other reasons. We’ll look into what causes it, how it’s diagnosed, and how it’s treated. We’ll focus on immune thrombocytopenic purpura (ITP), a big reason for low platelet counts in kids.
Key Takeaways
- Pediatric thrombocytopenia is a condition characterized by a low platelet count.
- Immune thrombocytopenic purpura (ITP) is a common cause of thrombocytopenia in children.
- Understanding the causes and clinical presentation is key for diagnosis.
- Treatment options depend on the cause and how severe it is.
- Good management can really help improve how a patient does.
Understanding Pediatric Thrombocytopenia
To understand pediatric thrombocytopenia, we need to look at its different parts. First, we must know what it is.
Definition and Normal Platelet Values in Children
Pediatric thrombocytopenia is when kids have too few platelets. Platelets help blood clot, and not enough can cause bleeding. In kids, platelet counts should be between 150,000 and 450,000/microL. Counts outside this range might mean thrombocytopenia.

Types of Thrombocytopenia in Pediatric Patients
There are several types of thrombocytopenia in kids, based on why it happens. The main types are:
- Immune thrombocytopenia (ITP): When the immune system attacks platelets by mistake.
- Inherited thrombocytopenia: Passed down in families, affecting platelet production or function.
- Secondary thrombocytopenia: Caused by other health issues, medicines, or infections.
Causes of Decreased Platelet Count in Children
There are many reasons why kids might have low platelet counts. Some include:
- Immune thrombocytopenia (ITP), where the immune system attacks platelets.
- Leukemia or aplastic anemia weakens the bone marrow’s blood-making ability.
- Viral infections can lower platelet production.
Knowing these causes helps doctors diagnose and treat thrombocytopenia in kids. By finding out why platelet counts are low, doctors can create the best treatment plan for each child.
Immune Thrombocytopenic Purpura (ITP) in Pediatrics
ITP in children is a disorder where the immune system attacks and destroys platelets. This leads to a higher risk of bleeding. It’s caused by the immune system making autoantibodies against the patient’s own platelets.
Pathophysiology
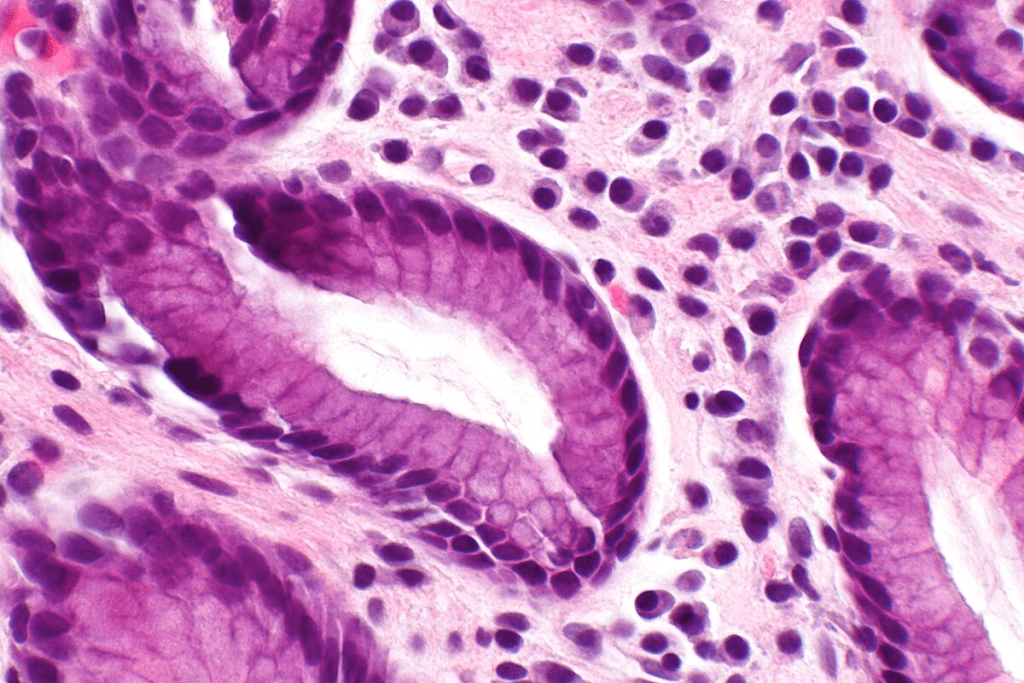
The immune system in children with ITP makes autoantibodies against platelets. This marks them for destruction. The spleen is where this happens, removing these platelets from the blood.
This reduction in platelets can cause bleeding problems. Key factors include:
- Autoantibody production against platelet glycoproteins
- Splenic sequestration and destruction of platelets
- Impaired platelet production due to immune-mediated effects on megakaryocytes
Epidemiology and Risk Factors
Pediatric ITP can happen at any age, but most often between 2 and 5 years. It affects boys and girls equally. Risk factors include a recent viral infection, which can trigger the disease in some children.
Acute vs. Chronic ITP
ITP in children can be either acute or chronic. Acute ITP is more common and usually goes away within six months without treatment. On the other hand, chronic ITP lasts longer than six months and may need more treatment.
The American Society of Hematology (ASH) suggests a careful approach for new cases. Children with mild symptoms may not need immediate treatment. This highlights the need for close monitoring and personalized treatment plans.
Clinical Presentation and Symptoms
Understanding ITP’s clinical presentation is key to early diagnosis and treatment. Children with ITP often show sudden petechiae, purpura, and mucosal bleeding. These signs come from a low platelet count, making it hard to form blood clots.
Common Signs and Symptoms
Pediatric ITP shows various signs and symptoms. Petechiae, small spots on the skin, and purpura, larger bruises, are common. Mucosal bleeding, like nosebleeds or bleeding gums, can also happen. Some kids might face more serious bleeding, like in the gut or bladder, but this is rare.
Severity Classification
ITP’s severity depends on the platelet count and bleeding symptoms. Mild ITP has fewer symptoms and higher platelet counts. Severe ITP has low counts and serious bleeding. Knowing the severity helps choose the right treatment.
Differentiating ITP from Other Causes of Thrombocytopenia
To tell ITP from other thrombocytopenia causes, a detailed check-up is needed. This includes a medical history, physical exam, and lab tests. It’s important to see if the low platelet count is alone or part of a bigger issue.
By looking closely at symptoms and signs, doctors can accurately diagnose ITP. They can then create a good treatment plan for kids with ITP.
Diagnostic Approach to Thrombocytopenia in Children
Diagnosing thrombocytopenia in kids involves a detailed history, physical exam, and lab tests. We’ll cover the steps to understand this condition fully.
Initial Evaluation and History Taking
When a child is suspected of having thrombocytopenia, we start with a thorough medical history and physical exam. We look for signs of bleeding or infections. This helps us find the cause.
Laboratory Testing
Labs are key in diagnosing thrombocytopenia. First, we do a complete blood count (CBC) to check the platelet count. We also examine a peripheral smear to look at platelet shape and rule out other issues.
- Complete Blood Count (CBC)
- Peripheral Smear Examination
- Blood Grouping and Direct Coombs Test (if necessary)
Bone Marrow Examination: When Is It Necessary?
A bone marrow test is not always needed, but is considered for atypical cases or suspected bone marrow failure. It helps check platelet production and look for cancer or other diseases.
Ruling Out Secondary Causes
It’s important to check for secondary causes of thrombocytopenia, like infections or autoimmune disorders. We do more tests based on the child’s symptoms and history to find any underlying issues.
- Infection Screening
- Autoimmune Disorder Testing
- Medication Review
By using this approach, we can accurately diagnose and treat thrombocytopenia in kids. This ensures they get the right care.
Current Pediatric ITP Treatment Guidelines
The latest guidelines for treating pediatric ITP have changed how we manage it. Now, we focus on each child’s needs. This is thanks to new rules from top hematology and pediatric groups.
American Society of Hematology (ASH) Guidelines
The ASH guidelines offer a detailed plan for managing pediatric ITP. They suggest treating based on how bad the symptoms are, not just the platelet count. For kids with mild symptoms, watching them closely is often the first step, without using medicines right away.
American Academy of Pediatrics (AAP) Recommendations
The AAP agrees with ASH on treating ITP based on risk. They say it’s key to look at the child’s health overall. This includes how bad the bleeding is and how it affects their life. The AAP also backs using medicines for kids with serious symptoms or heavy bleeding.
International Consensus Reports
Reports from around the world have made the guidelines even clearer. They bring together ideas from experts worldwide. These reports stress the need for a careful approach, taking into account the child’s age, lifestyle, and health. They also push for more research to improve care.
Risk-Based Treatment Approach
The core of today’s ITP treatment is a risk-based approach. This means looking at how likely it is for the child to bleed and how ITP affects their life. For kids at low risk, just watching them and supporting them might be enough. But for those at higher risk, treatments like corticosteroids or IVIg might be needed.
Using a risk-based approach helps us give more tailored and effective care. It means we avoid unnecessary treatments and aim for the best results for each child.
First-Line Management Strategies
Pediatric ITP management includes several first steps. These are observation, corticosteroids, and immunoglobulins. The right treatment depends on how bad the symptoms are and the patient’s platelet count.
Observation Approach for Mild Cases
Children with mild ITP and little bleeding might just be watched closely. This means no medicine right away. Watching closely is often for those with platelet counts over 20,000/ µL and no big bleeding.
Corticosteroid Therapy
Corticosteroids are a common first choice for kids with ITP. They help when there’s a lot of bleeding or very low platelet counts. Prednisone is given at 2 mg/kg/day for 1-2 weeks, then the dose is slowly lowered.
“Corticosteroids are key in treating pediatric ITP. They quickly raise platelet counts.”
Source: American Society of Hematology Guidelines
Intravenous Immunoglobulin (IVIg)
IVIg is also a first-line treatment, great for sudden bleeding or when platelets need to rise fast. It blocks the spleen from destroying platelets. The usual dose is 1 g/kg, and it might be given again if needed.
- Rapid increase in platelet count
- Effective for acute bleeding
- May require hospitalization for administration
Anti-D Immunoglobulin
Anti-D immunoglobulin is for Rh-positive patients with ITP. It works like IVIg to reduce platelet destruction. The dose is usually 50-75 µg/kg. Anti-D immunoglobulin can cause hemolysis, so it’s essential to monitor hemoglobin levels.
In conclusion, treating pediatric ITP starts with several steps. Each step is chosen based on the patient’s needs. Knowing the benefits and risks of each option helps doctors make the best choices for their patients.
Second-Line Therapies for Persistent or Chronic ITP
When first treatments for pediatric ITP don’t work, second-line therapies are key. These options help kids with ongoing ITP feel better and live better lives.
Thrombopoietin Receptor Agonists
Thrombopoietin receptor agonists (TPO-RAs) boost platelet production. TPO-RAs help kids with chronic ITP by making more platelets. They act like thrombopoietin, a hormone that controls platelet making.
Rituximab
Rituximab targets B cells, which fight platelets in ITP. By getting rid of B cells, rituximab lessens platelet destruction. Rituximab has helped many autoimmune diseases, including ITP, by giving lasting results.
Splenectomy: Considerations in Children
Splenectomy is a big surgery for kids with chronic ITP who’ve tried other treatments. The spleen destroys platelets and makes antibodies. While it can work, it’s a serious surgery with risks. Doctors decide on splenectomy based on how bad ITP is and the child’s health.
Emerging Therapies
New treatments give hope to kids with hard-to-treat ITP. These include spleen tyrosine kinase (Syk) inhibitors and other targeted therapies. Research and trials are checking if these treatments are safe and work well, giving kids more options in the future.
Supportive Care and Management of Bleeding
Managing bleeding in pediatric ITP is key. A full care plan is needed to prevent and handle bleeding issues. This approach helps improve patient results.
Activity Restrictions and Precautions
Children with ITP need to avoid risky activities. We suggest no contact sports or head trauma risks. Instead, they can do safe activities like swimming or reading.
Management of Acute Bleeding Episodes
Quick action is needed for bleeding in ITP. Apply pressure, use special agents, and follow the doctor’s orders. In bad cases, hospital care is needed to manage bleeding and avoid serious issues.
Platelet Transfusions: Indications and Limitations
Platelet transfusions might be needed for severe bleeding. But they should be used carefully. They’re usually for life-threatening bleeding or when other treatments don’t work.
Patient and Family Education
Teaching patients and families about ITP is vital. They need to know about safe activities, bleeding signs, and when to get help. Knowing this helps families manage their child’s condition better.
With these supportive care steps, we can better manage pediatric ITP. This reduces the chance of bleeding problems.
Conclusion: Prognosis and Long-term Outcomes
Pediatric Immune Thrombocytopenic Purpura (ITP) usually has a good prognosis. Most kids get better in six to eighteen months.
The long-term results for kids with ITP vary. They depend on several things, like if they have chronic ITP. About 20-30% of patients might have chronic ITP, which means their platelet count stays low for over a year.
Some factors increase the chance of chronic ITP. These include being older when symptoms start, being a girl, and having symptoms that come on slowly. Girls are more likely to get chronic ITP, with a 4.1 times higher risk.
Knowing these factors helps in managing ITP in kids better. It lets doctors create treatment plans that fit each child’s needs.
FAQ’s:
What is pediatric thrombocytopenia, and how is it defined?
Pediatric thrombocytopenia is a condition in kids with low platelet counts. This can cause bleeding or bruising. It’s when a child’s platelet count is below 150,000/μL.
What are the common causes of thrombocytopenia in children?
Thrombocytopenia in kids can come from many sources. This includes immune thrombocytopenic purpura (ITP), infections, and certain medicines. It can also be caused by bone marrow issues or genetic conditions.
How is ITP diagnosed in children?
Doctors use a detailed approach to diagnose ITP in kids. They look at the child’s medical history and do a physical exam. They also do a complete blood count (CBC) and a blood smear.More tests might be needed to make sure it’s not something else.
What are the current treatment guidelines for pediatric ITP?
The American Society of Hematology (ASH) and the American Academy of Pediatrics (AAP) have guidelines. They suggest a treatment plan based on how severe the symptoms are and the risk of bleeding.
What are the first-line treatment options for pediatric ITP?
For mild cases, doctors might just watch and wait. For more serious cases, they might use corticosteroids, IVIg, or anti-D immunoglobulin. The choice depends on the child’s symptoms and health.
When are second-line therapies considered in pediatric ITP?
If first-line treatments don’t work, doctors might try second-line options. These include thrombopoietin receptor agonists, rituximab, and sometimes surgery to remove the spleen.
How is bleeding managed in children with ITP?
Managing bleeding in kids with ITP involves careful care. This includes avoiding activities that might cause injury and using platelet transfusions in serious cases. They also treat bleeding right away.
What is the prognosis for children with ITP?
Most kids with ITP get better on their own within a few months. But some might have chronic ITP and need ongoing care.
How can families and caregivers support children with ITP?
Families and caregivers can help by learning about ITP. They should follow treatment plans and take steps to prevent bleeding. They also need to offer emotional support during treatment.
What are the key aspects of supportive care for pediatric ITP?
Supportive care for kids with ITP includes educating them and their families. It also means following activity restrictions and managing bleeding episodes. Platelet transfusions might be needed, too.
References
- Hui, D. (2022). Guidelines for pediatric immune thrombocytopenia. In StatPearls. Retrieved October 1, 2025, fromhttps://www.ncbi.nlm.nih.gov/books/NBK603670/
- Peters, J., et al. (2017). Thrombocytopenia in childhood: A practical guide for clinicians. Blood Reviews, 32(1), 1-14.https://www.sciencedirect.com/science/article/abs/pii/S1751722217301944