Intracytoplasmic Sperm Injection (ICSI) is a key fertility treatment. It has changed the way we help couples with fertility issues. This method gives hope to those facing challenges in conceiving iui process is painful.
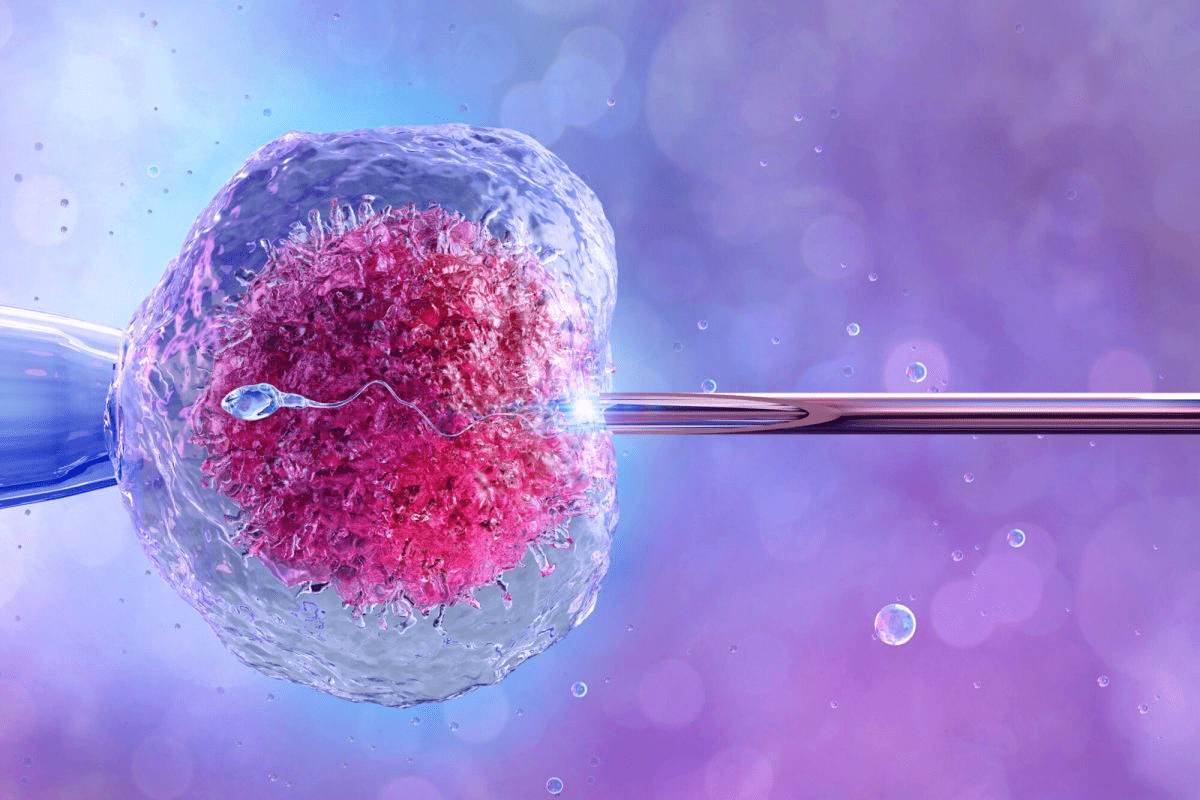
ICSI means injecting a single sperm into an egg. This way, it gets past natural barriers to fertilization. It has greatly increased the chances of getting pregnant for many.
Knowing what ICSI stands for helps couples understand their options. ICSI has opened new doors for many families. It’s a leading treatment in fertility care.
Key Takeaways
- ICSI is a specialized fertility treatment for couples facing male factor infertility.
- The procedure involves injecting a single sperm directly into an egg.
- ICSI has significantly improved fertilization rates for many patients.
- This technique is a part of IVF and is critical for certain fertility challenges.
- Understanding ICSI can help couples make informed decisions about their fertility options.
What Does ICSI Stand For: Understanding the Procedure

The term ICSI stands for a special IVF method. It involves injecting a single sperm into an egg. This method has changed how we treat some types of infertility, mainly those linked to male issues.
Definition of Intracytoplasmic Sperm Injection
Intracytoplasmic Sperm Injection (ICSI) means injecting a single sperm into an egg’s cytoplasm. The term intracytoplasmic means the injection happens inside the egg. The cytoplasm is the egg’s gel-like substance full of water, salt, and other important molecules.
This method is different from traditional IVF. In IVF, thousands of sperm are placed near an egg, hoping for natural fertilization. ICSI is great for men with low sperm count, poor motility, or abnormal sperm shape.
The Science Behind ICSI
ICSI’s science is all about precision and skill. First, a healthy sperm is chosen and prepared for injection. An egg is held steady with a special pipette. Then, a sharp pipette injects the sperm into the egg’s cytoplasm.
After the sperm is injected, the egg is watched for fertilization signs. If it fertilizes, the embryo is transferred to the uterus like in regular IVF. ICSI’s success has made it a key option for many facing fertility issues.
The History and Development of ICSI

ICSI’s journey started with a breakthrough in 1991. This marked a new era in fertility treatments. Gianpiero Palermo and his team achieved the first human pregnancy using Intra Cytoplasmic Sperm Injection (ICSI).
The Breakthrough of 1991
The year 1991 was a turning point in reproductive medicine. It was when ICSI was first successfully performed. This gave new hope to couples facing infertility, mainly those with male factor issues.
This achievement was the result of hard work and innovation in assisted reproductive technology.
The first human pregnancy from ICSI was a big deal. It set the stage for ICSI’s global use in fertility clinics.
Evolution of the Procedure Over Time
ICSI has evolved a lot. At first, it was doubted, but as success grew, it became common in fertility treatments.
ICSI’s growth includes better micromanipulation, improved sperm selection, and understanding egg quality. These changes have boosted ICSI’s success rates.
Today, ICSI is a key tool for couples trying to conceive. It has helped millions.
| Year | Milestone in ICSI Development | Impact on Fertility Treatment |
|---|---|---|
| 1991 | First successful ICSI pregnancy | Revolutionized treatment for male factor infertility |
| 1995 | Widespread adoption of ICSI in fertility clinics | Increased accessibility to effective fertility treatment |
| 2000s | Advancements in micromanipulation and sperm selection | Improved success rates and outcomes |
ICSI’s development has been key in improving fertility treatments. Its ongoing evolution promises better results for those trying to start a family.
When Is ICSI Recommended?
When couples face certain fertility challenges, ICSI can be a solution. Intracytoplasmic sperm injection (ICSI) is a special fertility treatment. It has changed how we tackle male factor infertility and other complex fertility issues.
ICSI is suggested for couples with specific fertility challenges. These challenges make regular IVF less effective. Let’s look at the main reasons ICSI is recommended.
Male Factor Infertility Cases
Male factor infertility is a top reason for ICSI. This includes cases where men have:
- Low sperm count (oligozoospermia)
- Poor sperm motility (asthenozoospermia)
- Abnormal sperm morphology (teratozoospermia)
- Obstructive azoospermia (absence of sperm in the ejaculate due to blockage)
- Non-obstructive azoospermia (absence of sperm in the ejaculate due to testicular failure)
In these cases, ICSI lets a single healthy sperm be injected into an egg. This bypasses natural fertilization barriers.
Previous IVF Failures
Couples with unexplained IVF failures or low fertilization rates in past IVF cycles might get ICSI. ICSI can overcome fertilization barriers that stopped success before.
Other Medical Indications
ICSI is also recommended for other medical reasons. These include:
- Couples where the male partner has a history of testicular trauma or surgery that may have affected sperm quality or count.
- Cases where sperm is retrieved surgically, such as through TESE (Testicular Sperm Extraction) or MESA (Microsurgical Epididymal Sperm Aspiration).
- Situations where genetic testing of embryos is needed, as ICSI uses a single sperm. This reduces the risk of contamination with extraneous sperm DNA.
- Couples with unexplained infertility who haven’t succeeded with regular IVF.
Understanding these indications helps us see ICSI’s role in helping couples achieve their fertility goals.
The Complete ICSI Procedure: Step by Step
For many couples facing infertility, ICSI offers a hopeful path to parenthood. This advanced reproductive technology involves several key steps. Each step requires precision and care for successful results.
Ovarian Stimulation Phase
The ICSI journey starts with ovarian stimulation. Medications are used to stimulate the ovaries to produce multiple eggs. This phase is vital as it boosts the chances of getting viable eggs for fertilization.
We monitor the patient’s response closely through ultrasound scans and blood tests. This ensures the medications are working effectively.
Key aspects of ovarian stimulation include:
- Administration of fertility drugs to stimulate egg production.
- Regular monitoring through ultrasound and blood tests.
- Adjusting medication dosages based on the patient’s response.
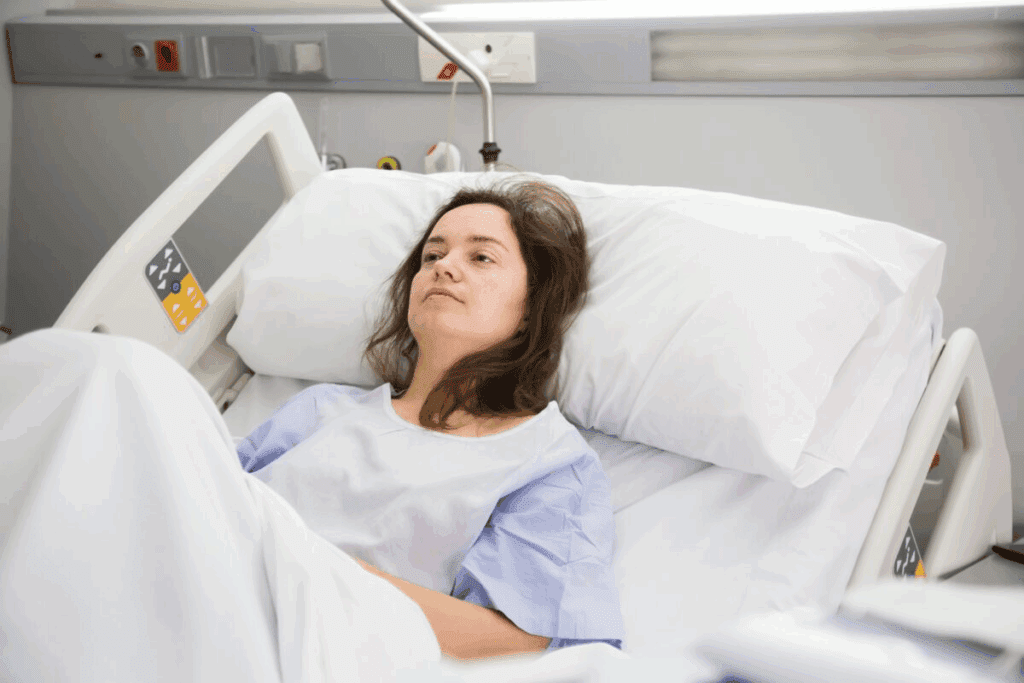
Egg Retrieval Process
Once the eggs are mature, the egg retrieval process begins. This is a minor surgical procedure done under sedation. A needle is guided by ultrasound to aspirate the eggs from the ovaries.
The egg retrieval process is typically:
- Performed under sedation to minimize discomfort.
- Guided by ultrasound to ensure precision.
- A relatively quick procedure, usually taking about 30 minutes.
Sperm Collection and Preparation
On the same day as the egg retrieval, a semen sample is collected from the male partner. The sperm is then prepared using specialized techniques to isolate the healthiest sperm for injection.
Sperm preparation involves:
- Centrifugation to separate sperm from seminal fluid.
- Selection of the most motile and morphologically normal sperm.
- Preparation of the sperm for microinjection.
The Microinjection Technique
The final step is the microinjection technique. A single sperm is injected into an egg using a microscopic needle. This delicate process is done using a specialized microscope and micromanipulation equipment.
The microinjection technique requires:
- Highly specialized equipment and expertise.
- Precision to ensure the sperm is injected into the egg without causing damage.
- Careful handling to maximize the chances of successful fertilization.
Understanding the detailed steps of the ICSI procedure helps couples appreciate the complexity and care needed. We are dedicated to providing the highest level of care and expertise throughout the ICSI process.
ICSI vs. Traditional IVF: Key Differences
Understanding the differences between ICSI and traditional IVF is key when choosing fertility treatments. We’ll dive into these differences to help you pick the best option for you.
Fertilization Methods Compared
ICSI involves directly injecting a sperm into an egg, boosting fertilization chances. Traditional IVF mixes eggs and sperm in a dish, letting fertilization happen naturally.
Key differences in fertilization methods:
- ICSI: Direct injection of sperm into the egg
- Traditional IVF: Mixing of eggs and sperm in a dish
Success Rate Differences
Success rates differ between ICSI and traditional IVF. They depend on egg and sperm quality and the cause of infertility.
| Treatment | Average Success Rate |
|---|---|
| ICSI | 50-60% |
| Traditional IVF | 40-50% |
When to Choose ICSI Over Standard IVF
ICSI is best for couples with male infertility, past IVF failures, or specific medical needs. We’ll guide you on if ICSI is right for you.
Success Rates and Outcomes of ICSI
ICSI success rates are key for those facing fertility issues. The path to parenthood is complex. Knowing ICSI outcomes helps manage hopes and make informed choices.
Statistical Overview of ICSI Success
ICSI has boosted fertilization rates for couples with male fertility issues. The live birth rate per cycle is about 40-50% for women under 35. This rate drops as the woman gets older.
Here’s a clearer look at ICSI success rates by age:
- Under 35 years: 40-50% live birth rate per cycle
- 35-37 years: 30-40% live birth rate per cycle
- 38-40 years: 20-30% live birth rate per cycle
- 41-42 years: 10-20% live birth rate per cycle
- Over 42 years: Less than 10% live birth rate per cycle
Factors Affecting ICSI Outcomes
Many factors influence ICSI success. These include sperm and egg quality, and the individuals’ ages. The skill of the embryologist and the lab’s quality also play a role.
Key factors affecting ICSI outcomes are:
- Sperm quality: Sperm quality and motility are vital.
- Eggs quality and quantity: Eggs’ number and quality matter a lot.
- Age: Age is a big factor, with success rates dropping after 35.
- Embryologist’s expertise: The embryologist’s skill can impact success.
Age-Related Success Rates
Age is a major factor in ICSI success. As women age, egg quality and quantity decline. This makes pregnancy harder.
Knowing how age affects success rates helps couples plan. Talking to a fertility specialist can give personalized insights into ICSI chances.
Potential Risks and Complications
ICSI is a highly effective fertility treatment, but it comes with risks. It’s important to know these risks to make the right choice.
Short-Term Risks
Short-term risks of ICSI include:
- Ovarian Hyperstimulation Syndrome (OHSS) from ovarian stimulation
- Infection or bleeding at the egg retrieval site
- Reactions to treatment medications
Long-Term Considerations
Research on long-term effects of ICSI is ongoing. Some studies hint at a higher risk of health issues in children conceived through ICSI. But, the evidence is not solid.
“The majority of children born after ICSI are healthy, but there may be a slightly increased risk of certain health problems.”
Talking to your healthcare provider about these risks is key.
Genetic Implications
ICSI raises concerns about genetic risks for the offspring. It bypasses natural selection, which might increase the risk of passing on genetic factors.
| Genetic Factor | Natural Conception | ICSI |
|---|---|---|
| Chromosomal Abnormalities | Natural selection processes may reduce transmission risk | Bypassing natural selection may increase transmission risk |
| Hereditary Conditions | Risk depends on genetic carrier status | Similar risk as natural conception if sperm is from a carrier |
Genetic counseling is advised for couples thinking about ICSI, if there’s a family history of genetic disorders.
In summary, ICSI is a valuable fertility tool, but knowing its risks is essential. Being informed helps patients make the best choices for their fertility journey.
The Emotional and Financial Journey of ICSI
ICSI, or Intracytoplasmic Sperm Injection, is more than a medical procedure. It’s a journey filled with emotions and financial concerns for many couples. It’s important to understand the psychological and financial sides before starting this path to parenthood.
Psychological Aspects of Treatment
The emotional ups and downs of ICSI can be intense. Couples may feel hopeful, anxious, or disappointed. The stress of uncertainty can be overwhelming, making emotional support key.
Everyone’s experience with ICSI’s psychological impact is different. Things like past struggles with infertility, the pressure of trying again, and fear of failure can weigh heavily.
Average Costs in the United States
The cost of ICSI is a big concern. In the United States, a single cycle can cost between $12,000 to $15,000. This doesn’t include extra costs for medications and tests.
It’s common to need more than one cycle, which can increase the total cost. So, planning your finances is a big part of the ICSI process.
Insurance Coverage Options
Insurance for ICSI varies a lot. Some plans cover part or all of the costs, while others don’t cover it at all.
- Check your insurance policy to understand what is covered.
- Some states have laws requiring insurance companies to cover infertility treatments.
- Discuss financial options with your healthcare provider.
Support Resources for Couples
Having the right support is vital for the ICSI journey. Support groups, counseling, and online resources offer emotional support and practical advice.
We suggest couples look into these resources. They can help deal with the emotional and financial challenges of ICSI.
Conclusion
Intracytoplasmic sperm injection (ICSI) has changed the world of reproductive medicine. It gives hope to couples facing fertility issues. This article has shown how ICSI helps many people.
The ICSI process involves injecting a single sperm into an egg. This method helps with male fertility problems and past IVF failures. Knowing about ICSI helps people choose the right fertility treatment.
ICSI has changed how we treat fertility problems. It offers new hope to those struggling. This shows how ICSI is a big step forward in reproductive medicine.
If you’re thinking about ICSI, talk to a fertility expert. They can help you decide what’s best for you. This summary shows why ICSI is a key option for those wanting to have children.
FAQ
What does ICSI stand for?
ICSI stands for Intracytoplasmic Sperm Injection. It’s a special IVF method where a single sperm is injected into an egg.
What is Intracytoplasmic Sperm Injection?
Intracytoplasmic Sperm Injection (ICSI) is a fertility treatment. It involves injecting a single sperm directly into an egg to help fertilize it.
How does ICSI work?
ICSI works by injecting a single sperm into the egg’s cytoplasm. This bypasses natural barriers, increasing fertilization chances.
When is ICSI recommended?
ICSI is recommended for male factor infertility and when IVF fails. It’s also used for specific medical reasons.
What is the difference between ICSI and traditional IVF?
ICSI and traditional IVF differ in fertilization methods. ICSI injects a sperm into an egg, while traditional IVF relies on natural fertilization.
What are the success rates of ICSI?
ICSI success rates depend on age, sperm, and egg quality. It generally has a high success rate in achieving fertilization and pregnancy.
What are the risks and complications of ICSI?
ICSI risks include short-term issues like infection or bleeding. Long-term and genetic implications are also possible, though rare.
How much does ICSI cost?
ICSI costs vary by location, clinic, and individual circumstances. In the United States, it can range widely.
Is ICSI covered by insurance?
Insurance coverage for ICSI varies. Some plans cover it fully or partially, while others may not.
What support resources are available for couples undergoing ICSI?
Couples can find support through counseling, support groups, and online resources. These help with the emotional and psychological aspects of treatment.
What is the significance of ICSI in fertility treatment?
ICSI has greatly improved fertility treatment. It offers a highly effective solution for those facing specific fertility challenges, like male factor infertility.
How is sperm prepared for ICSI?
Sperm preparation involves selecting and preparing a healthy sperm for injection. This is done through washing and centrifugation.
What is the role of ovarian stimulation in ICSI?
Ovarian stimulation is key in ICSI. It involves using medications to stimulate the ovaries to produce multiple eggs, increasing fertilization chances.
References
National Center for Biotechnology Information. Intracytoplasmic Sperm Injection (ICSI): A Fertility Treatment Overview. Retrieved from https://pubmed.ncbi.nlm.nih.gov/1352926/
National Center for Biotechnology Information. Evidence-Based Medical Guidance. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/1349351)**