Bisphosphonates have been key in treating osteoporosis for over 20 years. They help keep bones strong and lower fracture risks. But, they can also cause side effects that patients need to know about.Listing seven common bisphosphonates side effects and important safety information regarding their long-term use.
It’s important to understand the possible issues with bisphosphonates. This knowledge helps patients make better health choices. Knowing what might happen can also help patients and doctors work together to protect their bones.
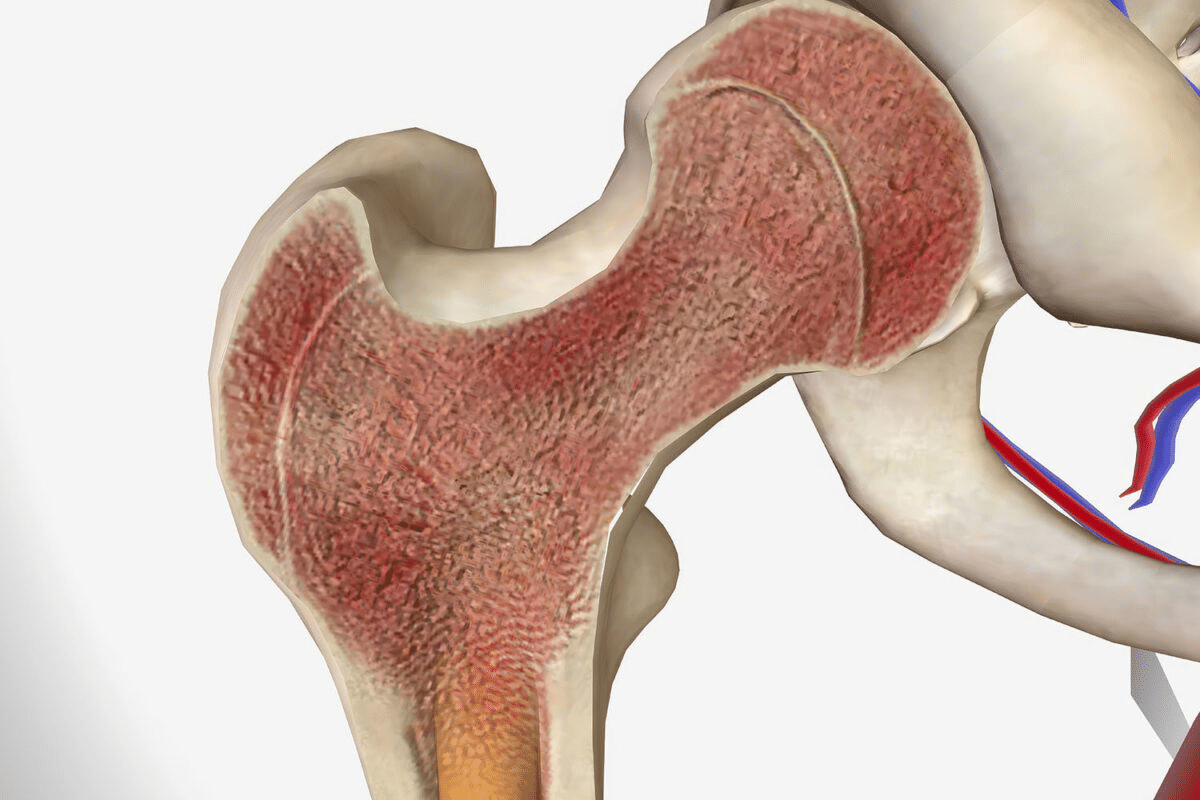
Bisphosphonates are key in fighting osteoporosis, a condition that weakens bones. They are part of a bigger plan to treat osteoporosis. Bisphosphonates are very important in this plan.
Bisphosphonates are medicines used to treat osteoporosis. They help keep or increase bone density. This is important because it lowers the risk of fractures.
Bisphosphonates slow down bone turnover, which lowers fracture risk. They do this by stopping bone resorption. This lets bone formation win over bone loss, making bones stronger.
Key benefits of bisphosphonates include:
There are many bisphosphonate medicines, each with its own use and how to take it. Some well-known ones are:
|
Medication Name |
Administration Frequency |
|---|---|
|
Alendronate (Fosamax) |
Weekly or daily |
|
Risedronate (Actonel) |
Weekly or monthly |
|
Ibandronate (Boniva) |
Monthly or quarterly (intravenous) |
The right bisphosphonate and how often to take it depends on the patient’s needs and health history.
Bisphosphonates are good for treating osteoporosis but can have side effects. It’s important for patients to know about these effects. This knowledge helps manage side effects and use the medication safely.
Side effects from bisphosphonates can differ for each patient. Common issues include heartburn, nausea, and trouble swallowing. Many patients, mainly those taking oral bisphosphonates, experience these problems.
“The most common adverse effects associated with oral bisphosphonates are gastrointestinal in nature,” notes a study on the safety profile of these medications.
“Gastrointestinal irritation, including esophageal irritation and gastritis, has been reported in patients taking oral bisphosphonates.”
Some factors can make side effects from bisphosphonates more likely. These include having past gastrointestinal issues, other health conditions, and taking medications that interact with bisphosphonates. For example, those with esophageal problems are more likely to get esophageal irritation from oral bisphosphonates.
Regular checks with healthcare providers are key for patients on bisphosphonates. These visits help track bone density and watch for side effects. It’s also important for patients to report any unusual symptoms right away.
Regular monitoring can help in early detection and management of side effects, improving the overall safety and efficacy of bisphosphonate treatment.
|
Monitoring Aspect |
Recommendation |
|---|---|
|
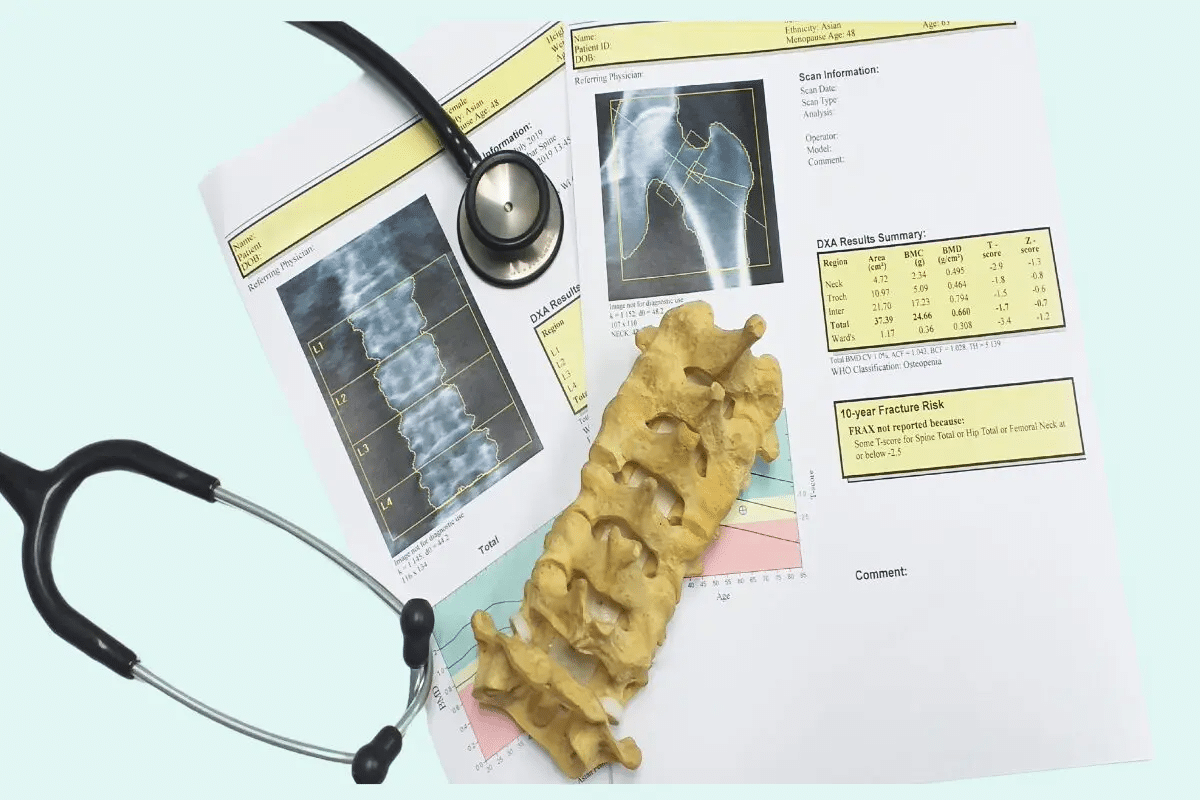
Bone Density |
Regular DEXA scans |
|
Gastrointestinal Health |
Patient reporting of symptoms; possible endoscopy for high-risk patients |
|
Renal Function |
Periodic serum creatinine checks |
Bisphosphonates can cause stomach problems. These issues can be mild or severe. People taking these drugs for osteoporosis often face stomach troubles.
Heartburn and esophageal irritation are common in bisphosphonate users. The drug can irritate the esophagus, causing pain and discomfort. Proper administration is key to minimizing this risk.
Here’s some data on stomach side effects:
|
Symptom |
Frequency |
|---|---|
|
Heartburn |
20% |
|
Nausea |
15% |
|
Difficulty Swallowing |
10% |
Dysphagia, or trouble swallowing, is another side effect. It can be uncomfortable and may lead to serious issues if not treated.
“Patients should be advised to remain upright and not lie down for at least 30 minutes after taking bisphosphonates to reduce the risk of esophageal irritation.”
Nausea and stomach discomfort are common too. These symptoms can be managed with proper administration and sometimes extra medication.
To lessen stomach side effects, follow these guidelines:
Intravenous infusions of bisphosphonates can trigger acute phase reactions in some patients. These reactions are a common side effect associated with the administration of bisphosphonates for osteoporosis treatment.
One of the primary characteristics of acute phase reactions is the onset of flu-like symptoms, including fever. Patients may feel as though they have contracted the flu, with symptoms such as chills, fatigue, and a general feeling of being unwell.
In addition to flu-like symptoms, patients may experience muscle pain and headaches. These symptoms can range from mild to severe and are usually temporary.
The duration of acute phase reactions can vary, but they typically resolve on their own within a few days. Management strategies include the use of over-the-counter pain relievers to alleviate symptoms.
The severity and frequency of acute phase reactions tend to decrease with subsequent infusions. Approximately 1 in 3 patients experience these reactions with the first infusion, characterized by flu-like symptoms, fever, muscle pain, and headaches. Patients should be aware of this and discuss any concerns with their healthcare provider.
Bisphosphonates help treat osteoporosis but can cause pain in bones, joints, and muscles. This side effect can really affect how well a person lives and sticks to their treatment plan.
It’s hard to tell if pain from bisphosphonates or osteoporosis is the cause. Doctors suggest a detailed check-up to figure out the pain’s source.
The National Osteoporosis Foundation says it’s key to know why someone is in pain. This is because osteoporosis can cause pain from fractures or other bone problems.
When pain starts from bisphosphonates can differ for each person. Some might feel pain right after starting treatment. Others might not feel it until later.
A study in the Journal of Bone and Mineral Research found pain usually starts about 3 years after starting bisphosphonates.
Dealing with pain from bisphosphonates needs a few steps. Changing the treatment plan, like the dose or type of bisphosphonate, might help.
Severe pain might mean stopping bisphosphonates. Doctors look at the good and bad of keeping up treatment for each patient.
“For patients with severe musculoskeletal pain, deciding to keep or stop bisphosphonates depends on their health and risk of fractures.”— American Society for Bone and Mineral Research
Osteonecrosis of the jaw (ONJ) is a serious issue for those taking bisphosphonates for osteoporosis. It causes jawbone tissue death, leading to exposed bone in the mouth. This can be very painful and hard to treat.
The exact cause of ONJ is not known, but bisphosphonates are thought to disrupt bone remodeling. This leads to micro-fractures and bone death. Poor oral health and certain dental procedures can trigger ONJ in susceptible individuals.
Several factors raise the risk of ONJ. These include how long you’ve been on bisphosphonates, the type of bisphosphonate, and dental problems or recent surgery. Patients with a history of dental extractions or oral surgery are at higher risk.
|
Risk Factor |
Description |
|---|---|
|
Duration of Therapy |
Longer treatment duration increases ONJ risk |
|
Dental Problems |
Presence of dental issues or recent surgery |
|
Potency of Bisphosphonate |
Higher potency bisphosphonates have a higher risk |
Preventive dental care is key for bisphosphonate users. Regular dental visits, good oral hygiene, and avoiding unnecessary dental work can lower ONJ risk. Patients should inform their dentist about their bisphosphonate treatment.
When ONJ happens, treatment aims to manage symptoms and pain. This may include antibiotics, pain meds, and sometimes surgery to remove dead bone tissue.
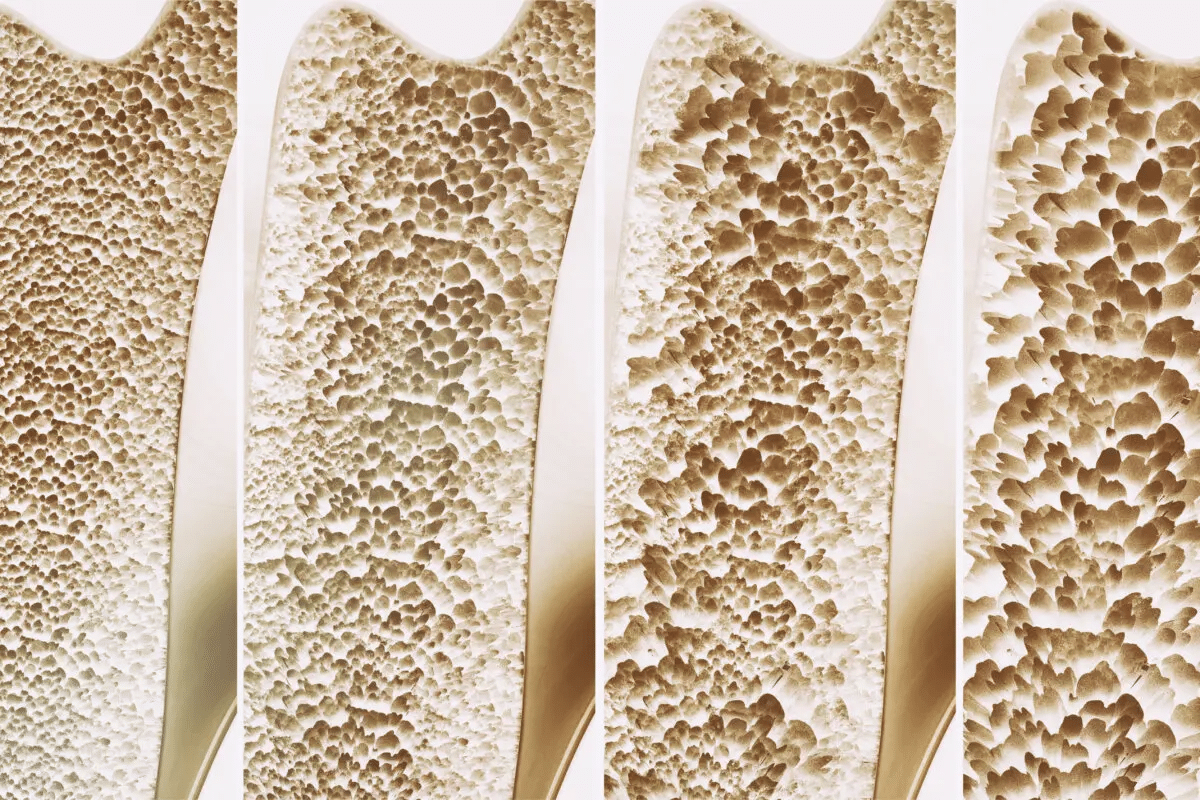
Bisphosphonates are good for treating osteoporosis but can cause atypical femoral fractures. This is a rare but serious side effect for those on long-term therapy.
Bisphosphonates slow down bone loss, which can cause micro-cracks in bones. This increases the risk of atypical femoral fractures, mainly in those treated for over 5 years. It’s important for patients and doctors to know about this risk.
Those on long-term bisphosphonate therapy should watch for new thigh, hip, or groin pain. These signs could mean an atypical femoral fracture is coming. Spotting it early is vital to avoid a full fracture.
When atypical femoral fractures are suspected, X-rays or MRI scans are used to confirm. Quick evaluation is key to start the right treatment.
For those at risk, doctors might look at other treatments or change the bisphosphonate plan. This could mean a break from the drug or switching to something else.
“The decision to continue or modify bisphosphonate therapy should be based on an individual patient’s risk-benefit profile.”
Knowing the risks and benefits of bisphosphonates helps patients and doctors make better choices for osteoporosis treatment.
Bisphosphonates can cause hypocalcemia, which is low calcium in the blood. This is more common in people who already have low calcium or vitamin D. It’s important to manage this condition to avoid serious problems.
Bisphosphonates stop bones from releasing calcium into the blood. This can worsen hypocalcemia in those with low calcium or vitamin D. It’s key for patients to have enough calcium and vitamin D before starting treatment.
Hypocalcemia can cause several symptoms, including:
It’s important to notice these symptoms early to get help quickly.
Supplementing with calcium and vitamin D is vital for patients on bisphosphonates. Getting enough of these nutrients can help avoid electrolyte imbalances. Patients should talk to their doctor about the right amount to take.
It’s important to regularly check electrolyte levels, like calcium, for patients on bisphosphonates. Doctors might suggest blood tests to catch any imbalances. Spotting problems early helps prevent bigger issues.
Doctors might adjust the bisphosphonate dose, add calcium and vitamin D supplements, or fix any underlying issues. They can create a plan that fits each patient’s needs.
Ocular complications and vision changes are possible side effects of bisphosphonate therapy. Patients need to know about these risks. Bisphosphonates can cause eye-related issues.
Bisphosphonates are linked to eye problems like conjunctivitis, uveitis, and scleritis. These can cause discomfort, pain, and serious vision issues if not treated quickly.
Patients on bisphosphonates should watch for vision or eye health changes. Look out for blurred vision, eye pain, redness, and increased sensitivity to light. If these symptoms appear, see a healthcare provider right away.
Treatment for eye problems linked to bisphosphonates varies. Sometimes, stopping the bisphosphonate is needed. Other times, more medications or therapies are required.
Preventive care is important to reduce eye risks. Regular eye exams and telling your eye care provider about bisphosphonate treatment are key. This proactive approach helps protect eye health during osteoporosis treatment.
Bisphosphonates are a key part of treating osteoporosis. They help lower the chance of fractures in patients. But, they can also cause side effects that patients need to know about.
It’s important to understand both the good and bad sides of bisphosphonate therapy. These drugs make bones stronger. Yet, they might upset your stomach, cause fever, or lead to other issues.
Patients should talk to their doctors to lessen risks. They should watch for side effects, take care of their teeth to avoid jaw problems, and know the signs of unusual bone fractures.
Being informed and careful helps patients get the most from bisphosphonate therapy. This careful balance is essential for treating osteoporosis well.
Bisphosphonates can cause stomach upset, flu-like symptoms, and muscle pain. They may also lead to jaw problems, bone fractures, and eye issues. Hypocalcemia and other side effects are possible too.
To lessen stomach problems, take bisphosphonates with an empty stomach. Stay upright for 30 minutes after. Avoid bending or lying down.
You might feel flu-like, have a fever, muscle pain, or headaches. These symptoms start within 24-48 hours and usually go away in a few days.
For pain, try over-the-counter pain meds, rest, and physical therapy. Sometimes, stopping the bisphosphonate is needed.
ONJ is jawbone damage. To prevent it, see your dentist regularly, keep your teeth clean, and avoid dental work while on bisphosphonates.
Look out for thigh or groin pain. This could mean an atypical femoral fracture is coming. Tell your doctor if you have these symptoms.
Taking calcium and vitamin D helps keep bones strong. It also prevents low calcium levels, a side effect of bisphosphonates.
Bisphosphonates can cause eye issues like conjunctivitis, uveitis, and scleritis. If you have vision problems, tell your doctor.
Follow your doctor’s advice, report any side effects, and keep up with regular check-ups. This helps manage risks and adjust treatment as needed.
Bisphosphonates help prevent fractures, slow bone loss, and increase density. They are a key treatment for osteoporosis.
Long-term use can raise the risk of fractures, jaw problems, and other issues. It’s important to monitor and assess risks over time.
Government Health Resource. Evidence-Based Medical Guidance. Retrieved from https://www.nejm.org/doi/full/10.1056/NEJMcp1513724
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!