For decades, lupus has been a mystery to many, affecting millions globally. New research has found a key part of its puzzle: an imbalance of T cells in the immune system. This breakthrough is leading to new ways to treat the disease.lupus root causeRoot Issues: underlying causes thrombocytopenia
Living with lupus is tough, causing pain and inflammation in the skin, joints, and organs. At Liv Hospital, we’re here to help. We offer care and support for those looking for answers and better treatments.
Key Takeaways
- Recent research has identified an imbalance of T cells as a fundamental root cause of lupus.
- Lupus is a complex autoimmune disease that causes inflammation and pain in various body parts.
- Understanding immune cell abnormalities is key to finding new treatments.
- Liv Hospital is dedicated to delivering top-notch healthcare with full support.
- Patients can now benefit from new treatments thanks to this groundbreaking research.
Understanding Systemic Lupus Erythematosus (SLE)
SLE is a chronic autoimmune disease that affects many body systems. It causes a wide range of symptoms. This disease impacts hundreds of thousands in the United States.
Definition and Prevalence in the United States
SLE happens when the immune system attacks the body’s own tissues. This leads to inflammation and damage in different parts of the body. The disease affects about 322 out of every 100,000 people in the United States.
Women, mostly those of childbearing age, are more likely to get SLE. The Lupus Foundation of America says diagnosing SLE can be hard. This is because its symptoms can look like those of other diseases.
Common Symptoms and Manifestations
SLE symptoms vary but often include fatigue, fever, and joint pain. People with SLE may also have skin rashes and be sensitive to light. In severe cases, SLE can damage the kidneys, heart, and brain.
- Musculoskeletal symptoms like arthritis and muscle pain
- Dermatological manifestations, including rashes and lesions
- Renal involvement, potentially leading to lupus nephritis
The Autoimmune Nature of Lupus
SLE is an autoimmune disease. This means the body’s immune system attacks healthy tissues. The exact cause of this is not fully understood yet.
“The autoimmune nature of lupus makes it a challenging condition to manage, requiring a multifaceted treatment approach that addresses both the symptoms and the underlying immune dysregulation.”
Understanding SLE’s autoimmune nature helps doctors develop better treatments. These treatments aim to balance the immune system and lessen the disease’s effects on patients’ lives.
The Lupus Root Cause: T-Cell Imbalance
Recent studies have found a key link between T-cell imbalance and lupus. This discovery came from top institutions like Northwestern Medicine and Brigham and Women’s Hospital.
The Breakthrough Research by Northwestern Medicine and Brigham and Women’s Hospital
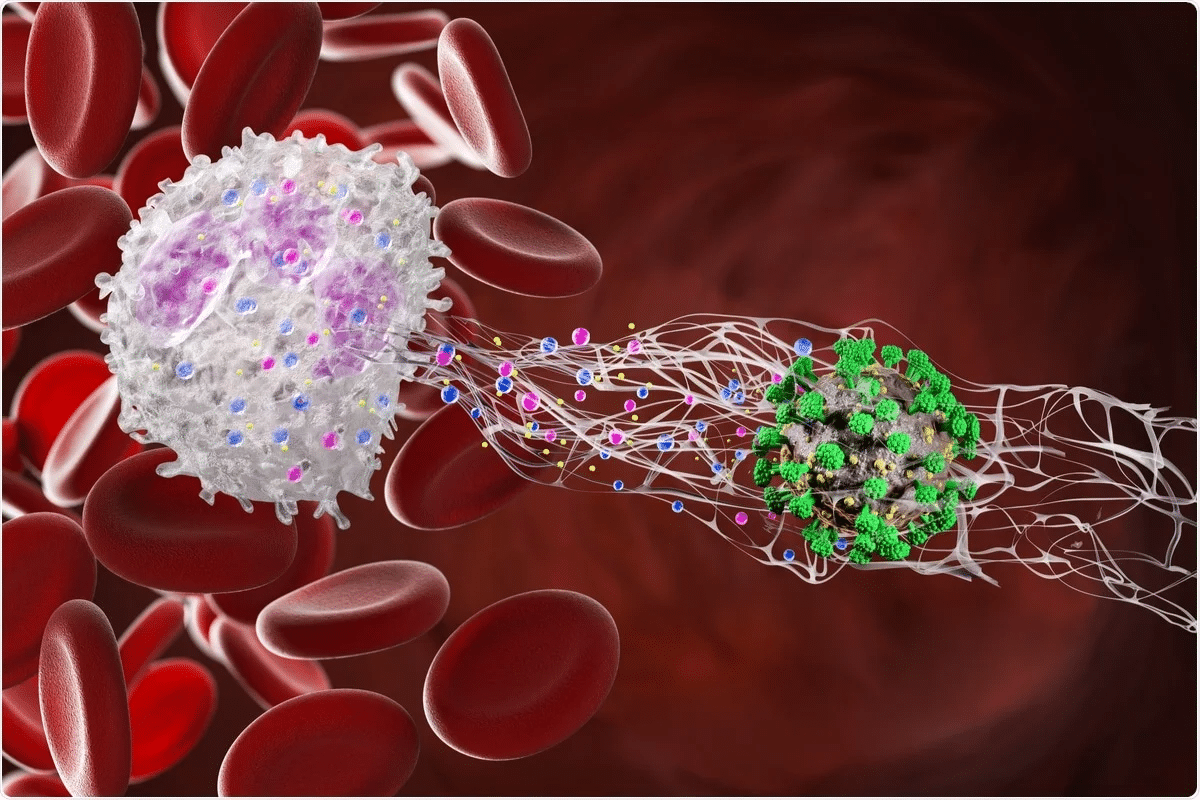
A team-up between Northwestern Medicine and Brigham and Women’s Hospital has made a big leap in understanding lupus. They found that lupus patients have too many harmful T-cells and not enough helpful ones. This imbalance is key to how lupus gets worse.
Excess Damaging T-Cells vs. Insufficient Healing T-Cells
The fight between harmful and healing T-cells is central to lupus. Harmful T-cells cause inflammation and damage, while healing T-cells fix and control the immune system. When there are too many harmful T-cells and not enough healing ones, lupus symptoms appear.
|
T-Cell Type |
Function |
Impact in Lupus |
|---|---|---|
|
Damaging T-Cells |
Contribute to inflammation and tissue damage |
Excessive presence leads to increased disease activity |
|
Healing T-Cells |
Repair and regulate the immune response |
Insufficient numbers result in inadequate immune regulation |
Impact on Skin, Lungs, and Gut Barrier
The T-cell imbalance hits different parts of the body, like the skin, lungs, and gut. It can cause rashes and lesions on the skin. In the lungs, it may lead to inflammation and breathing problems. The gut barrier can also get damaged, causing trouble with nutrient absorption and increased permeability.
Knowing how T-cell imbalance affects these areas is key to finding better treatments. Researchers aim to tackle the root cause to help lupus patients more effectively.
The Role of Interferon in Lupus Development
Interferon is key in understanding lupus. It’s a protein that helps fight off infections. We’ll look at how too much interferon can lead to lupus and the mechanisms behind it.
Normal Function of Interferon
Interferon helps protect us from viruses and other threats. It triggers immune responses to get rid of these invaders. Normally, it’s made in small amounts and controlled by our immune system. But in lupus, this control is lost.
“Interferon is a double-edged sword; it’s essential for fighting off viruses, but when dysregulated, it can contribute to autoimmune diseases.”
Excess Interferon and Lupus
Studies show lupus patients have too much interferon. This extra interferon makes the immune system too active. This can make the disease worse and cause more damage. We’ll see how this affects the body and contributes to lupus.
The Blockage of the Aryl Hydrocarbon Receptor (AHR)
Excess interferon blocks the Aryl Hydrocarbon Receptor (AHR). The AHR helps keep the immune system balanced. When interferon is too high, it stops the AHR from working. This leads to fewer healing T-cells and an immune imbalance.
|
Mechanism |
Effect on Lupus |
|---|---|
|
Excess Interferon |
Increased disease activity and tissue damage |
|
AHR Blockage |
Reduced production of healing T-cells |
|
Immune System Imbalance |
Contribution to lupus development and severity |
Understanding interferon’s role in lupus is key to finding new treatments. By tackling the disease’s root causes, we can improve treatment options and outcomes for patients.
Genetic Factors Contributing to Lupus
Research shows that genetics play a big role in lupus risk. Lupus often runs in families, showing a hereditary link.
Hereditary Risk Factors
People with a family history of lupus are more at risk. Studies found that if one twin has lupus, the other is more likely to get it too. This is true, even more so for identical twins, pointing to a strong genetic connection.
Key hereditary risk factors include:
- A family history of lupus or other autoimmune diseases
- Genetic variations that affect the immune system’s function
Specific Genes Associated with Lupus
Several genes are linked to a higher lupus risk. These genes affect the immune system in different ways, like clearing dead cells and controlling immune cell activity.
Notable genes linked to lupus include:
- IRF5, which regulates interferon, a key immune protein
- STAT4, involved in signaling that controls immune cell function
- BLK, linked to B cell function and tolerance
How Genetics Interact with Environmental Triggers
Genetics are key in lupus risk, but environment also plays a part. The mix of genetic predisposition and environmental factors can lead to lupus in some people.
Examples of environmental triggers include:
- Ultraviolet light exposure, which can trigger lupus flares
- Infections, which may trigger autoimmune responses
- Certain medications, known to induce lupus-like symptoms in some individuals
Understanding how genetics and environment interact is key to fighting lupus. It helps in finding better ways to prevent and treat the disease.
Environmental Triggers for Lupus
Lupus is a complex autoimmune disease. It can be triggered or worsened by many environmental factors. Knowing these triggers is key to managing lupus and improving life quality for those with it.
Ultraviolet Light Exposure
Ultraviolet (UV) light is a known lupus trigger. UV radiation can cause skin problems and make symptoms worse. People with lupus should protect themselves from UV light. This includes using sunscreen, wearing protective clothes, and staying out of the sun during peak hours.
Infections and Viruses
Some infections and viruses can start lupus or make it worse. For example, the Epstein-Barr virus (EBV) increases lupus risk. We’ll talk about how to handle infections and keep the immune system strong.
Medications That Can Trigger Lupus
Some medicines can make lupus symptoms worse or start them. This includes certain blood pressure drugs, antibiotics, and anti-inflammatory drugs. It’s important for patients to tell their doctors about all their medicines to watch for lupus triggers.
Environmental Pollutants and Toxins
Environmental pollutants and toxins can also trigger lupus. These include silica dust, pesticides, and industrial chemicals. Cutting down on these exposures can help manage lupus symptoms.
|
Environmental Trigger |
Examples |
Prevention Strategies |
|---|---|---|
|
Ultraviolet Light |
Sun exposure, tanning beds |
Use sunscreen, wear protective clothing |
|
Infections and Viruses |
Epstein-Barr virus, other viral infections |
Practice good hygiene, get vaccinated |
|
Medications |
Certain antihypertensives, antibiotics |
Monitor medication use with healthcare provider |
|
Pollutants and Toxins |
Silica dust, pesticides, industrial chemicals |
Avoid exposure, use protective gear |
By understanding and managing these environmental triggers, people with lupus can better control their symptoms. This improves their overall well-being.
Hormonal Influences on Lupus Development
Hormones play a big role in lupus, a complex autoimmune disease. The way hormones and the immune system work together can change how lupus starts and how bad it gets.
The Female Predominance in Lupus
Lupus mostly affects women, mainly when they are of childbearing age. This has led scientists to look into how sex hormones might be involved. They found that estrogen might be key, as it affects how the immune system works.
Women are more likely to get lupus, which hints at a hormonal link. Studies suggest that sex hormones could play a part in how active lupus is.
Estrogen’s Role in Immune Regulation
Estrogen can change how the immune system works. It can enhance the making of certain antibodies and change how immune cells act. This might help explain why autoimmune diseases like lupus happen.
|
Hormone |
Effect on Immune System |
Relevance to Lupus |
|---|---|---|
|
Estrogen |
Modulates immune cell activity, enhances antibody production |
Potential contributor to lupus development and severity |
|
Progesterone |
Influences immune response, may have protective effects |
Less clear, requires further research |
Hormonal Changes During Pregnancy and Menopause
Hormones change a lot during pregnancy and menopause. These changes can also affect lupus. In pregnancy, more estrogen can make lupus symptoms worse for some women. On the other hand, less estrogen in menopause might also change how lupus symptoms show up.
It’s important to understand these hormonal shifts to manage lupus well. Doctors need to think about these changes when planning treatment for patients.
Identifying Personal Triggers and Prevention Strategies
Finding out what causes lupus flare-ups can really help people with lupus live better. Knowing and controlling these triggers can lessen symptoms’ frequency and intensity.
Keeping a Symptom Journal
Keeping a symptom journal is a great way to find personal triggers. It means writing down daily activities, possible triggers, and any symptoms. Looking for patterns can show what triggers symptoms. For example, noting when symptoms happen, the weather, and new foods or meds can be very helpful.
A symptom journal can be a simple notebook or a fancy app. The most important thing is to keep it up and write everything down. Apps can also remind you and analyze your data, making it easier to spot patterns.
Working with Healthcare Providers to Identify Triggers
While a journal is very useful, talking to healthcare providers is also key. Doctors can help figure out what triggers symptoms and explain journal data. They might also suggest tests or refer you to specialists.
At doctor’s visits, share your journal with your healthcare provider. This teamwork can help understand your specific triggers and create a plan to prevent flare-ups.
Lifestyle Modifications to Reduce Flare-ups
Once you know what triggers your symptoms, making lifestyle changes can help a lot. Changing your diet, managing stress, and avoiding certain environments are common steps. For example, eating more fruits, veggies, and omega-3s can help fight inflammation.
|
Lifestyle Modification |
Potential Benefit |
|---|---|
|
Avoiding Ultraviolet Light Exposure |
Reduces risk of skin-related flare-ups |
|
Stress Management Techniques |
Helps in reducing stress-related flare-ups |
|
Balanced Diet |
Supports overall health and reduces inflammation |
By using these strategies, people with lupus can actively manage their condition. This can greatly improve their quality of life.
Breakthrough Treatments Targeting the Root Cause
Recent research has led to new treatments for lupus. These treatments aim to tackle the disease’s root cause. This progress offers hope for better managing lupus.
Anifrolumab: Blocking Interferon Activity
Anifrolumab is a big step in lupus treatment. It’s a monoclonal antibody that blocks interferon activity. This has shown promise in reducing lupus symptoms in trials.
Restoring T-Cell Balance
Research shows T-cell imbalance plays a big role in lupus. New treatments aim to balance these cells. This could help reduce inflammation and damage caused by lupus.
Other Emerging Therapies Based on Root Cause Research
Other treatments are being developed too. They target specific disease pathways. As we learn more about lupus, we’ll see more innovative treatments.
Personalized Medicine Approaches for Lupus
The future of lupus treatment is personalized. Treatments will be tailored to each patient’s needs. This could greatly improve treatment outcomes and quality of life.
Combining emerging therapies and personalized medicine is key. With ongoing research, we’re hopeful for more effective treatments for lupus.
Conclusion: The Future of Lupus Research and Treatment
Lupus is a complex disease, and finding its root cause is key to better treatments. Research by places like Northwestern Medicine and Brigham and Women’s Hospital has made big strides. They’ve found that T-cell imbalance and interferon play big roles in lupus.
New treatments are on the horizon, aiming to tackle lupus at its source. Anifrolumab, for example, blocks interferon, giving patients new hope. We expect more research to bring even more effective ways to manage lupus.
It’s important to find what triggers lupus and how to prevent it. Working with doctors and making healthy lifestyle choices can help. The future of lupus treatment is looking up, with a focus on care that’s tailored to each person.
FAQ
What is lupus and how does it affect the body?
Lupus is a complex autoimmune disease. It can affect many parts of the body, like the skin, joints, and kidneys. It happens when the immune system attacks healthy tissues, causing various symptoms.
What is the root cause of lupus?
Research shows that an imbalance of T cells is a main cause of lupus. This imbalance leads to too many damaging T cells and not enough healing ones. This imbalance helps lupus progress.
How does interferon contribute to lupus development?
Interferon is important for the immune system. But too much of it can harm by blocking the aryl hydrocarbon receptor (AHR). This reduces healing T cells and makes lupus worse.
Are there any genetic factors that contribute to lupus?
Yes, genetics play a big role in lupus. Certain genes increase the risk of getting the disease. These genes can work with environmental factors to cause lupus.
What are some common environmental triggers for lupus?
Environmental triggers for lupus include UV light, infections, some medications, and pollutants. These can make symptoms worse and help lupus progress.
Why is lupus more common in females, and what role does estrogen play?
Lupus is more common in females because of hormones, like estrogen. Estrogen affects the immune system. Changes in estrogen levels, like during pregnancy or menopause, can affect lupus symptoms.
How can patients identify their personal triggers and manage their condition?
Patients can find their personal triggers by keeping a symptom journal and talking to their doctors. Making lifestyle changes, like avoiding UV light and managing stress, can help control symptoms.
What are some emerging treatments targeting the root cause of lupus?
New treatments, like anifrolumab, aim to fix lupus by blocking interferon and balancing T cells. Other treatments are being developed based on research into lupus’s causes.
What is the future of lupus research and treatment?
The future of lupus research and treatment looks good. Studies are exploring new therapies and personalized medicine. Understanding lupus better will lead to better treatments and outcomes for patients.
References
National Center for Biotechnology Information. Evidence-Based Medical Guidance. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC5125867/









