
Coronary artery disease is a big problem worldwide, leading to many heart attacks. An electrocardiogram (ECG), a simple, non-invasive test, plays a key role in diagnosing heart conditions, including those related to blocked arteries. Can an ECG spot a blocked artery? Learn the key role of ECG arterial blockage detection in heart diagnostics. Be empowered with knowledge.
We look into how an ECG works and its role in spotting arterial blockages. These blockages are a major cause of heart problems and death. Studies, like one on diabetes and heart disease, show how ECG findings link to blockages. This makes the ECG a vital tool for doctors.
Key Takeaways
- An ECG is a key tool for checking heart health.
- ECG findings can show if arteries are blocked.
- The link between ECG results and heart disease is important.
- Finding blocked arteries early can stop serious heart issues.
- An electrocardiogram is a non-invasive and effective way to diagnose.
Understanding ECG and Its Purpose

ECGs are key in heart health monitoring technology. They show the heart’s electrical activity. This is vital for diagnosing and managing heart issues.
What is an Electrocardiogram (ECG)?
An electrocardiogram, or ECG, is a test that records the heart’s electrical signals. It’s non-invasive and helps us see the heart’s rhythm and function. Electrodes on the skin capture these signals, showing them as a graph.
How ECG Records Heart Activity
Recording heart activity with an ECG involves several steps. Electrodes are placed on the body, usually on the chest, arms, and legs. These electrodes send the heart’s electrical signals to the ECG machine, which displays them as a graph.
The graph shows important details about the heart’s rhythm and function. It can spot heart conditions or other issues.
Normal ECG Readings and Patterns
A normal ECG shows a pattern that means a healthy heart. The tracing includes parts like the P wave, QRS complex, and T wave. Each part shows different aspects of the heart’s electrical activity.
|
ECG Component |
Description |
Normal Pattern |
|---|---|---|
|
P Wave |
Represents atrial depolarization |
Upright in lead II, less than 0.12 seconds |
|
QRS Complex |
Represents ventricular depolarization |
Less than 0.12 seconds, varying morphologies |
|
T Wave |
Represents ventricular repolarization |
Upright in leads I, II, and V4-V6 |
Healthcare professionals analyze these components to check the heart’s function. They look for any abnormalities. This helps in diagnosing heart conditions and finding the right treatment.
The Relationship Between ECGs and Arterial Blockages
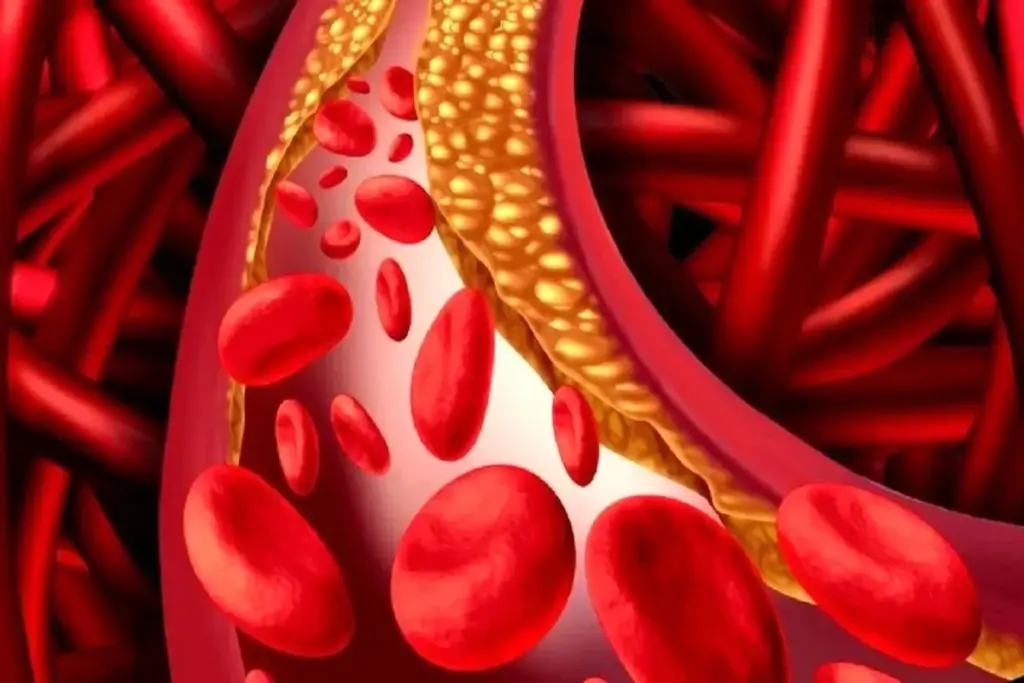
ECGs help us see how arterial blockages affect the heart. Arterial blockages happen when plaque builds up in arteries. This can stop the heart muscle from getting the oxygen and nutrients it needs.
How Arterial Blockages Affect Heart Function
Blockages in arteries can cut off blood flow to the heart muscle. This can lead to chest pain, known as angina, or even a heart attack. The impact on the heart depends on where and how bad the blockage is.
ECGs can spot these heart function changes. They record the heart’s electrical signals. This gives us clues about how blockages affect the heart.
ECG Changes That May Indicate Blockages
Some ECG changes can show if there are blockages. For example, changes in the ST segment, T waves, and Q waves can mean ischemia or infarction. These changes happen because the blockage messes with the heart’s electrical signals.
ST segment deviation is a key sign of heart problems. It can show up as ST segment elevation or depression. Both are important for diagnosing coronary artery disease.
ST Segment Elevation and Depression
ST segment elevation often means a heart attack. It happens when a coronary artery is completely blocked. ST segment depression suggests ischemia, where the heart muscle doesn’t get enough oxygen.
Knowing these ECG changes is key for catching artery blockages early. Doctors can then decide on the right tests and treatments.
ECG Arterial Blockage Detection: Capabilities and Limitations
It’s key to know what ECGs can and can’t do in finding blockages. ECGs are a big help in heart health checks.
What ECGs Can Reveal About Arterial Health
ECGs show the heart’s electrical activity. They can spot blockages by looking for odd heart rhythms or patterns.
Key insights from ECGs include:
- Detection of arrhythmias that may be associated with arterial blockages
- Identification of ST segment changes indicative of ischemia or infarction
- Recognition of Q waves that may signify previous myocardial infarctions
Sensitivity and Specificity in Detecting Blockages
ECGs are good tools, but they’re not perfect. New ECG tech helps more, but we must know their limits.
The sensitivity of ECGs is how well they find blockages. The specificity is how well they say who doesn’t have blockages.
Why Some Blockages Go Undetected
Some blockages might not show up on ECGs. This can be because of where the blockage is, how bad it is, or if there’s extra blood flow.
Reasons for undetected blockages include:
- Blockages in certain coronary artery branches that are not reflected in standard ECG leads
- Presence of silent ischemia, where there are no noticeable symptoms
- Limitations in the ECG technology used, such as standard ECG vs. advanced 12-lead ECG
Knowing what ECGs can and can’t do helps doctors. They can then decide if more tests are needed.
Types of Arterial Blockages and Their ECG Signatures
Arterial blockages come in different forms, each with its own ECG signs. Knowing these differences is key to correct ECG reading and patient care.
Complete vs. Partial Blockages
Blockages can be either complete or partial. Each type affects ECG readings differently. Complete blockages block the artery fully, causing big ECG changes like ST-segment elevation. This often means a heart attack is happening.
Partial blockages cause smaller ECG changes. This makes them harder to spot.
“The presence of a blockage, whether complete or partial, necessitates prompt evaluation and management to prevent further cardiac damage,” cardiologists say.
Acute vs. Chronic Blockages
It’s also important to tell acute from chronic blockages. Acute blockages happen suddenly and show big ECG changes. Chronic blockages show up as stable ECG patterns over time, like T-wave inversion or Q waves.
Location-Specific ECG Changes
The spot where a blockage happens affects the ECG. For example, a block in the left anterior descending artery shows up in leads V2-V4. A block in the right coronary artery shows up in leads II, III, and aVF. Knowing these helps doctors diagnose and treat better.
Understanding different blockages and their ECG signs helps doctors. This leads to better care for heart patients.
What to Expect During an ECG Procedure
The ECG procedure is a non-invasive test that records the heart’s electrical activity. Knowing what to expect can help reduce anxiety. We’re here to guide you through what happens during an ECG.
Preparation and Setup
Before starting, you’ll need to prepare in a few simple ways. You might need to remove jewelry or metal objects that could interfere. Our team will clean the areas on your chest, arms, and legs where the electrodes will go.
The electrodes are small, sticky patches that connect to the ECG machine. They detect your heart’s electrical activity and send it to the machine for analysis. You’ll lie down on an examination table, and our team will place the electrodes as needed.
The Testing Process
Once the electrodes are in place, the ECG machine starts recording your heart’s activity. You’ll need to stay very quiet and breathe normally. The machine captures the electrical signals from your heart and displays them on a monitor for our team to analyze.
In some cases, you might do a stress test as part of your ECG. This involves exercising on a treadmill or stationary bike. It helps see how your heart works under stress, which is important for diagnosing heart conditions.
“The ECG is a valuable diagnostic tool that provides insights into the heart’s electrical activity. By understanding the test process, patients can feel more comfortable and informed about their heart health.”Cardiology Expert
Duration and Discomfort Levels
The actual ECG recording takes only a few minutes. The whole process, from start to finish, usually takes about 10 to 15 minutes. You might feel a slight pinch when the electrodes are removed, but it’s usually painless and doesn’t cause much discomfort.
|
Procedure Step |
Duration |
Discomfort Level |
|---|---|---|
|
Preparation |
5 minutes |
Minimal |
|
ECG Recording |
2-3 minutes |
None |
|
Removing Electrodes |
1 minute |
Slight pinch |
Knowing what to expect during an ECG can make it less scary. Our team is dedicated to making sure you’re comfortable and getting accurate results to support your heart health.
Interpreting ECG Results for Possible Blockages
Reading electrocardiogram (ECG) results is key to spotting possible blockages in arteries. Doctors use ECGs to see how the heart’s electrical activity is doing. This helps them understand the heart’s health.
Key Indicators Cardiologists Look For
Doctors look at several important signs in ECG results for blockages. These include:
- ST Segment Changes: Changes in the ST segment can show heart problems like ischemia or infarction, often due to blockages.
- Q Waves: Deep and wide Q waves might mean a heart attack in the past, showing blockages.
- T Wave Inversion: Inverted T waves can mean the heart is not getting enough blood, which might be due to blockages.
Common Misinterpretations and False Positives
Even though ECGs are very helpful, they’re not perfect. Mistakes can happen for many reasons, like:
- Technical Issues: Bad electrode placement or faulty equipment can give wrong readings.
- Patient Factors: Things like body type or health problems can change ECG results.
The Importance of Clinical Correlation
It’s vital to match ECG findings with what the patient is experiencing. This means looking at symptoms, medical history, and other test results. By combining ECG data with clinical info, doctors can make better choices for patient care.
We stress that reading ECG results needs a full approach. It’s about using both technical knowledge and clinical insight to spot blockages correctly.
Stress ECG Testing for Detecting Hidden Arterial Issues
Stress ECG testing is key for finding hidden blockages in arteries. It checks the heart’s work when it’s stressed, usually through exercise or medicine.
How Stress Tests Reveal Blockages
When you do a stress test, your heart beats faster and needs more oxygen. If there are blockages, the heart might not get enough oxygen. This can show up on the ECG as changes.
These changes might include ST segment shifts or T-wave inversions. They can also show arrhythmias. Doctors use these signs to spot blockages and figure out how bad the disease is.
Exercise vs. Pharmacological Stress Testing
There are two main ways to do stress tests: exercise and pharmacological. Exercise tests use physical activity, like on a treadmill, to raise your heart rate.
Pharmacological tests, though, use medicine to mimic exercise. This is for people who can’t exercise for health reasons.
Interpreting Stress Test Results
Reading stress test results needs skill and careful thought. Doctors look for signs of heart problems, like ST segment changes. They also check how well the heart works under stress.
If a test shows problems, it might mean serious heart disease. This could lead to more tests, like coronary angiography, to check further.
Stress ECG testing helps find hidden heart problems early. This is key for managing heart disease and preventing serious heart issues.
Comparing ECG to Other Arterial Blockage Detection Methods
Several methods can detect arterial blockages, each with its own strengths and weaknesses. Electrocardiogram (ECG) is a key tool in cardiology. But how does it stack up against other advanced diagnostic techniques?
Coronary Angiography
Coronary angiography is the top choice for finding coronary artery disease. It uses a contrast dye to show blockages on an X-ray. Though very accurate, it’s a risky, invasive procedure.
Comparison with ECG: ECG is safe and non-invasive. It can’t see blockages directly but is good for first checks and monitoring. Angiography gives clear views of the arteries, making it better for complex blockages.
CT Coronary Angiography
CT coronary angiography is a safe test that uses CT scans to see the heart’s arteries. It shows detailed images of the heart and its blood vessels, spotting blockages.
Comparison with ECG: Like ECG, CT coronary angiography is safe. But it gives more detailed info about the arteries and can find blockages ECG might miss.
Nuclear Stress Tests
Nuclear stress tests use a tiny amount of radioactive material to see how well the heart gets blood during stress and rest.
Comparison with ECG: ECG can be used in stress tests. But nuclear stress tests offer more info on heart muscle blood flow, helping spot ischemia or infarction.
Cardiac MRI
Cardiac MRI uses magnetic fields and radio waves to make detailed heart images. It checks heart function, finds scar tissue, and sees coronary arteries.
Comparison with ECG: Cardiac MRI gives a full picture of the heart’s structure and function. It beats ECG in showing the heart and its blood vessels directly.
|
Diagnostic Method |
Invasiveness |
Ability to Detect Blockages |
Additional Information |
|---|---|---|---|
|
ECG |
Non-invasive |
Indirect detection through electrical activity |
Heart rhythm, electrical activity |
|
Coronary Angiography |
Invasive |
Direct visualization of blockages |
Detailed coronary artery images |
|
CT Coronary Angiography |
Non-invasive |
Direct visualization of blockages |
Coronary artery images, calcium scoring |
|
Nuclear Stress Tests |
Non-invasive |
Indirect detection through perfusion |
Heart muscle perfusion, ischemia detection |
|
Cardiac MRI |
Non-invasive |
Direct visualization of heart structure and function |
Comprehensive heart assessment, scar tissue identification |
When ECGs Fail: Silent Ischemia and Missed Blockages
ECGs are great for spotting heart problems, but they’re not perfect. They can miss blockages, which is scary. This is true for silent myocardial ischemia, where the heart doesn’t get enough oxygen but doesn’t hurt.
Understanding Silent Myocardial Ischemia
Silent myocardial ischemia is when the heart muscle doesn’t get enough oxygen. This is usually because of a blockage in the coronary arteries. But, it doesn’t cause chest pain or other usual signs of heart trouble. This makes it very dangerous because it can go unnoticed until it’s too late.
Risk Factors for Silent Ischemia:
- Diabetes
- High blood pressure
- High cholesterol
- Smoking
- Family history of heart disease
Risk Factors for ECG-Negative Blockages
Some people are more likely to have blockages that ECGs miss. This includes those with diabetes, a history of heart disease, or many risk factors for heart disease. It’s very important for these people to get a full check-up for heart health beyond just an ECG.
Warning Signs Beyond ECG Results
Even if an ECG looks fine, there are other signs that might mean there’s a blockage. Look out for shortness of breath, feeling very tired, or pain in the arms, back, neck, jaw, or stomach. Spotting these signs early is key to catching artery blockages before they get worse.
It’s vital to take a complete approach to heart health. This means regular check-ups, risk assessments, and tests when needed. By doing this, we can find and manage risks linked to silent ischemia and blockages that ECGs can’t see.
When to Seek Medical Attention for Suspected Arterial Blockages
Knowing when to get medical help for arterial blockages is key. If not treated quickly, blockages can cause serious heart problems. We’ll show you the emergency signs, symptoms needing an ECG, and risk factors that mean you should act fast.
Emergency Warning Signs
Some symptoms are a medical emergency. If you or someone else has any of these, get help right away:
- Chest pain or discomfort that spreads to the arm, neck, or jaw
- Shortness of breath without trying hard
- Feeling very tired or weak
- Dizziness or feeling like you might pass out
- Cold sweats or feeling sick to your stomach
These signs might mean a heart attack or serious heart problem. Quick action is very important.
Symptoms That Warrant an ECG
If you’re feeling any of these, talk to your doctor about getting an ECG:
- Recurring chest pain or discomfort
- Feeling your heart beat irregularly or too fast
- Unexplained shortness of breath
- Swelling in your legs or ankles
An ECG can find heart problems and blockages.
Risk Factors That Increase Urgency
Some risk factors make you more likely to get blockages. If you have any of these, watch your heart health closely:
|
Risk Factor |
Description |
|---|---|
|
Family History |
A family history of heart disease |
|
Smoking |
Using tobacco products |
|
High Blood Pressure |
Uncontrolled high blood pressure |
|
High Cholesterol |
High levels of bad cholesterol |
|
Diabetes |
Diabetes that’s not well-managed |
If you’re at risk, talk to your doctor about heart health monitoring technology and cardiac monitoring for artery health. This can help prevent problems.
Real-time Arterial Blockage Detection Using ECG Monitoring
Real-time ECG monitoring is changing how we find and handle blockages in arteries. This new tech lets doctors diagnose faster and more accurately. This leads to better health outcomes for patients. We’ll look at the different ways and tools used for detecting blockages in real-time.
Ambulatory ECG Monitoring
Ambulatory ECG monitoring uses a portable device to record the heart’s electrical signals for 24 to 48 hours. It’s great for catching symptoms that don’t show up in regular tests.
Benefits of Ambulatory ECG Monitoring:
- It keeps monitoring for a long time.
- It catches heart problems that only happen sometimes.
- It helps doctors understand and manage heart issues better.
Implantable Cardiac Monitors
Implantable cardiac monitors are small devices put under the skin to watch the heart’s rhythm all the time. They can spot irregular heartbeats and other heart issues, sending alerts to doctors.
Advantages of Implantable Cardiac Monitors:
- They can monitor the heart for a long time.
- They automatically send alerts for heart problems.
- They’re put in with a small procedure.
Remote Monitoring Technologies
Remote monitoring lets doctors check on patients’ heart activity from afar. This is done through devices that send ECG data to a central place.
Key Features of Remote Monitoring Technologies:
|
Feature |
Description |
Benefit |
|---|---|---|
|
Real-time Data Transmission |
ECG data is sent in real-time to healthcare providers |
Timely intervention for cardiac events |
|
Continuous Monitoring |
Ongoing surveillance of heart activity |
Early detection of possible issues |
|
Alert Systems |
Automated alerts for abnormal heart rhythms or events |
Prompt response to cardiac abnormalities |
In conclusion, new ECG monitoring techs like ambulatory monitoring, implantable monitors, and remote systems are changing how we deal with artery blockages. These tools help doctors act fast and well to heart problems. This leads to better care for patients.
Advanced ECG Technology for Blockage Detection
Advanced ECG systems are changing how we find blockages in arteries. They make diagnosing better. This helps patients get help early and recover faster.
12-Lead vs. Standard ECGs
The traditional ECG uses 12 leads to show the heart’s electrical activity. A standard ECG has fewer leads. The 12-lead ECG gives a clearer picture, helping spot blockages better.
Key differences between 12-lead and standard ECGs include:
- More detailed data with 12-lead ECGs
- Can spot small heart activity changes
- 12-lead ECGs pinpoint blockages better
|
Feature |
12-Lead ECG |
Standard ECG |
|---|---|---|
|
Lead Configuration |
12 leads |
Fewer leads |
|
Data Detail |
Comprehensive |
Limited |
|
Blockage Detection |
More accurate |
Less accurate |
Continuous Monitoring Systems
Continuous ECG monitoring systems give real-time data for a long time. They show how the heart works under different conditions. This is great for catching blockages or heart issues that come and go.
The benefits of continuous monitoring include:
- Sees short heart problems
- Checks if treatments work
- Helps care for patients sooner
AI-Enhanced ECG Interpretation
Artificial Intelligence (AI) is making ECG readings better. AI looks at lots of ECG data to find signs of blockages. This makes diagnosing faster and more accurate.
Advantages of AI-enhanced ECG interpretation:
- More accurate diagnoses
- Quicker results
- Finds small heart issues
As we keep improving these ECG technologies, finding and treating blockages will get even better. This will lead to better health outcomes for patients.
Future Developments in ECG-Based Blockage Detection Systems
ECG-based blockage detection systems are getting smarter. New technologies are making ECGs better at finding blockages in arteries.
Innovations on the Horizon
New ECG tech is all about being more accurate and monitoring in real-time. Some exciting new features include:
- Advanced signal processing techniques
- Artificial intelligence (AI) integration for enhanced pattern recognition
- Improved electrode materials for better signal quality
Wearable ECG Devices
Wearable ECG devices are changing how we monitor heart health. They give us constant, real-time data. This makes it easier to catch problems early.
Wearable ECG devices offer many benefits, such as:
- Continuous monitoring
- Early detection of heart conditions
- Increased patient engagement in health monitoring
Predictive Analytics and Machine Learning
Predictive analytics and machine learning are big steps forward for ECGs. They look at lots of data to spot patterns that might mean blockages.
|
Technology |
Application |
Benefit |
|---|---|---|
|
Predictive Analytics |
Analyzing ECG data for risk assessment |
Early identification of possible blockages |
|
Machine Learning |
Pattern recognition in ECG readings |
More accurate blockage detection |
Using these technologies, we can make ECGs even better at finding blockages. This means better care for patients.
Conclusion
We’ve looked at how electrocardiograms (ECGs) help find blockages in arteries. This is very important for heart health. ECGs give us clues about heart activity and possible blockages.
It’s key to know what ECGs can and can’t do in heart care. They show a lot about artery health. But, they’re just one part of a bigger check-up plan. This plan might also include more tests like coronary angiography or stress tests.
While ECGs are helpful, they’re not perfect. Sometimes, heart problems can be hidden. But, knowing the risks and signs can help people stay on top of their heart health with their doctors.
New ECG tech, like AI and wearable devices, is getting better. These advancements could lead to catching blockages sooner and more accurately. This could really help patients get better care.
FAQ
What is an ECG, and how does it detect arterial blockages?
An electrocardiogram (ECG) is a test that checks the heart’s electrical activity. It shows how well the heart is working. It spots blockages by looking for changes in the heart’s electrical signals.
Can an ECG detect all types of arterial blockages?
ECG is very helpful in finding blockages, but it’s not perfect. Some blockages might not show up on a standard ECG. More tests, like stress ECG or coronary angiography, might be needed.
What is the difference between a standard ECG and a stress ECG?
A standard ECG checks the heart at rest. A stress ECG checks it during exercise. Stress ECG can find blockages that aren’t seen at rest.
How accurate is ECG in detecting arterial blockages?
ECG’s accuracy depends on the blockage type and severity, and other heart issues. It’s good at finding many blockages, but not always 100% right. More tests might be needed to be sure.
What are the benefits of real-time ECG monitoring for detecting arterial blockages?
Real-time ECG monitoring lets doctors watch the heart continuously. It helps catch blockages and other heart problems quickly.
How do advancements in ECG technology improve blockage detection?
New ECG tech, like 12-lead ECGs and AI, makes ECG better at finding blockages. It’s more accurate and useful.
What are the risk factors for ECG-negative blockages?
Risk factors include silent ischemia, diabetes, high blood pressure, and family heart disease history. People with these risks might need more tests, even with a normal ECG.
When should I seek medical attention for suspected arterial blockages?
Get medical help right away for emergency signs like chest pain or trouble breathing. If you have symptoms or risk factors, see a doctor quickly.
References
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC3214392/





