
Calcium pyrophosphate deposition disease (CPPD), also known as pseudogout or pyrophosphate arthropathy, is a type of arthritis. It affects the joints and the soft tissues around them. This condition happens when calcium pyrophosphate dihydrate crystals build up in the cartilage and soft tissues of the joints calcium pyrophosphate deposition disease.
It usually affects older adults. It can be hard to diagnose because it looks like other joint problems, like gout or rheumatoid arthritis. At Liv Hospital, we focus on our patients. We work hard to diagnose and treat CPPD arthritis well. This helps our patients manage their condition better and live a better life.
CPPD disease is a type of joint problem that has caught the eye of researchers. It’s caused by calcium pyrophosphate dihydrate crystals in joints. This leads to different symptoms.
To get what CPPD is, knowing its definition and medical terms is key. Calcium Pyrophosphate Deposition Disease is what CPPD stands for. It’s different from other joint issues like gout.
CPPD disease happens when calcium pyrophosphate dihydrate crystals build up in joints. This can cause sudden joint pain, known as pseudogout. Or, it can lead to long-term joint damage.
Medical terms for CPPD include “calcium pyrophosphate dihydrate crystal deposition disease” and “pyrophosphate arthropathy.” Knowing these terms helps doctors diagnose and treat CPPD better.
The CPPD medical term is used a lot in healthcare. It stands for Calcium Pyrophosphate Deposition Disease. This term makes it easier for doctors to talk about it and write it down.
It’s important to note that CPPD and pseudogout are not the same. Pseudogout is the sudden, painful episodes that can happen with CPPD.
CPPD is linked to other joint problems like gout and basic calcium phosphate crystal deposition disease. Even though they seem similar, they are different. This is because of the type of crystals and how they affect joints.
The table below shows how CPPD (including pseudogout) differs from other common joint problems:
|
Condition |
Type of Crystal |
Commonly Affected Joints |
Clinical Presentation |
|---|---|---|---|
|
CPPD/Pseudogout |
Calcium Pyrophosphate Dihydrate |
Knee, wrist, metacarpophalangeal joints |
Acute inflammatory arthritis (pseudogout) or chronic degenerative joint disease |
|
Gout |
Monosodium Urate |
Big toe, ankle, knee |
Acute inflammatory arthritis |
|
Basic Calcium Phosphate Crystal Deposition Disease |
Basic Calcium Phosphate |
Shoulder, hip |
Periarthritis, tendinitis, or destructive arthropathy |
CPPD arthritis is more common with age, hitting people over 60 hard. As more people get older, knowing about CPPD’s demographics is key for doctors and researchers.
CPPD mainly hits older adults, with 4-7% of them affected. It gets more common with age, posing a big risk for the elderly.
Several factors increase the risk of getting CPPD. These include age, genetics, and some metabolic conditions. Knowing these can help spot and manage CPPD early.
Recent studies have shed light on CPPD’s prevalence. For example, a study on US veterans found over 25,000 with CPPD. This shows CPPD’s big impact on healthcare.
To better understand CPPD’s prevalence and demographics, let’s look at some data:
|
Age Group |
Prevalence Rate |
Number of Individuals |
|---|---|---|
|
60-69 years |
3.5% |
10,000 |
|
70-79 years |
5.2% |
15,000 |
|
80 years and older |
7.5% |
5,000 |
The data shows CPPD’s prevalence goes up with age. As the population ages, healthcare needs to be ready to handle more CPPD cases.
To understand CPPD, we need to know how calcium pyrophosphate dihydrate crystals form and settle in joints. These crystals build up in joint cartilage and soft tissues. This leads to inflammation and damage in the joints.
The process of calcium pyrophosphate crystals forming is complex. It’s influenced by many biochemical and physiological factors. It happens when these crystals deposit abnormally in the joint, mainly in the cartilage.
While we don’t know all the details, research points to several factors. These include joint degeneration, metabolic disorders, and genetic predisposition.
Several things can lead to calcium pyrophosphate crystals settling in joints. These include:
CPPD is similar to other calcium crystal diseases, like basic calcium phosphate crystal deposition disease. But, the type of crystals and symptoms can vary a lot.
Knowing these differences is key for correct diagnosis and treatment.
It’s important to understand the signs of CPPD arthritis to diagnose and treat it well. This condition can show up in different ways, from sudden inflammation to long-term damage.
Acute CPPD arthritis, or pseudogout, causes sudden pain, swelling, redness, and warmth in the joints. It’s similar to gout but is caused by different crystals.
The pain from an acute attack can be very bad and usually gets worse in 24 to 48 hours. Things that can trigger an attack include:
Chronic CPPD arthropathy is different because it causes slow joint damage and pain. It can look like osteoarthritis but happens faster and in unusual joints.
Chronic CPPD arthropathy is marked by:
CPPD arthritis can affect many joints, but some are more common. The most often affected joints are:
In summary, CPPD arthritis can show up in many ways, from sudden attacks to long-term damage. Knowing these signs is key to diagnosing and treating it right.
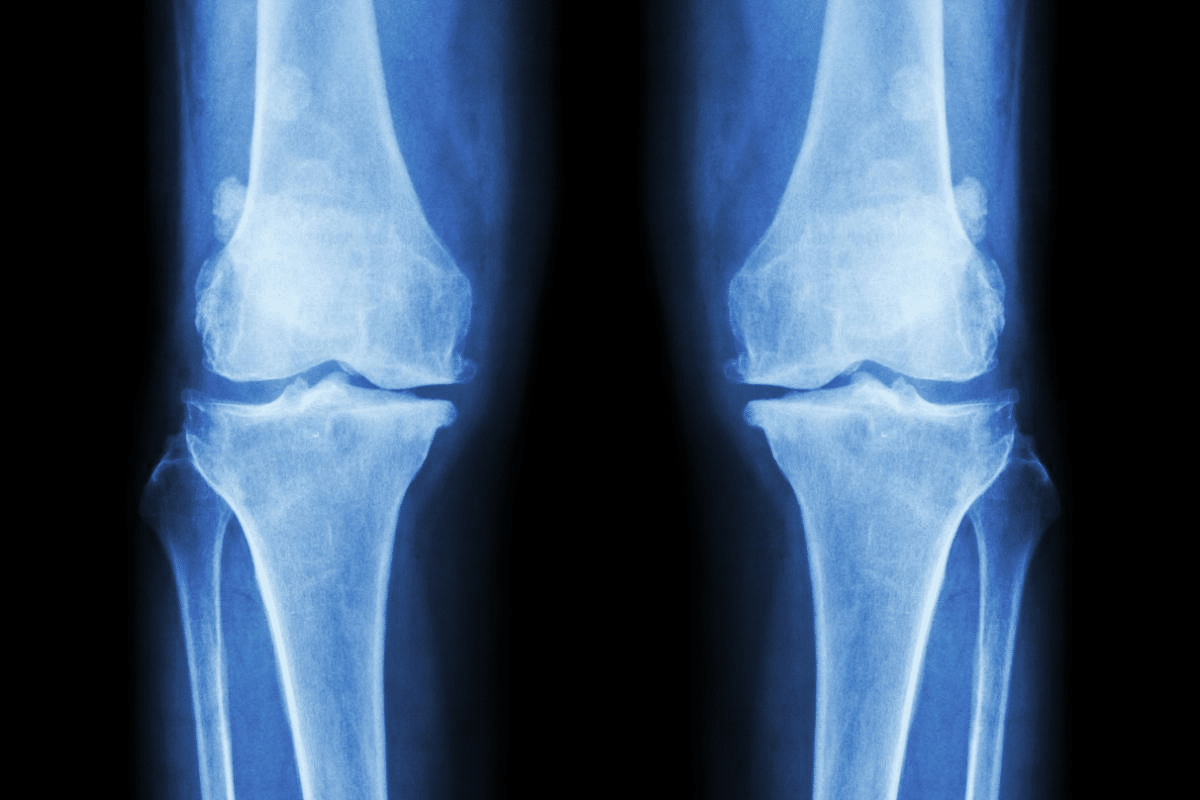
To diagnose Calcium Pyrophosphate Deposition Disease (CPPD), we use a few key steps. These include clinical evaluation, imaging studies, and joint fluid analysis. Getting the diagnosis right is key to treating the disease well.
First, we do a detailed check-up and look at the patient’s history. We look at their symptoms, past health, and physical check-ups. We’re looking for signs of CPPD, like sudden pain in big joints like the knee or wrist.
We also think about other diseases that might look like CPPD, like gout or osteoarthritis. Knowing how long the symptoms last and how bad they are helps us understand the situation better.
Imaging tests are very important for diagnosing CPPD. X-rays help us see if there’s calcium buildup in the cartilage. We might also use ultrasound or MRI to see more details about the joint and any crystals.
The best way to confirm CPPD is by looking at the joint fluid. We take fluid from the joint and check it under a microscope. If we see certain crystals, we know it’s CPPD.
|
Diagnostic Method |
Description |
Key Findings |
|---|---|---|
|
Clinical Evaluation |
Assessment of patient symptoms and medical history |
Acute monoarthritis, joint pain |
|
Imaging Studies |
Use of X-rays, ultrasound, or MRI to detect crystal deposits |
Chondrocalcinosis, joint damage |
|
Joint Fluid Analysis |
Examination of synovial fluid for CPPD crystals |
Rhomboid or rod-shaped crystals with weak positive birefringence |
By using all these methods together, we can accurately find out if someone has CPPD. Then, we can make a treatment plan that fits their needs.
Diagnosing CPPD arthritis can be tricky because it looks like other arthritis types. This makes it important to figure out the exact cause. A detailed check is needed to find the right diagnosis.
CPPD and gout both involve crystals in the joints. But, they have different crystals and symptoms. Gout has monosodium urate crystals, while CPPD has calcium pyrophosphate dihydrate crystals.
|
Characteristics |
CPPD |
Gout |
|---|---|---|
|
Crystals Involved |
Calcium Pyrophosphate Dihydrate |
Monosodium Urate |
|
Commonly Affected Joints |
Knees, wrists, hips |
Big toe, ankles, knees |
|
Clinical Presentation |
Acute attacks, chronic arthropathy |
Acute attacks, tophi formation |
CPPD can be told apart from osteoarthritis by looking at joint fluid and X-rays. Both can cause pain and stiffness. But, CPPD often shows more inflammation.
Rheumatoid arthritis is an autoimmune disease with symmetrical joint pain and specific antibodies. CPPD, on the other hand, is caused by crystals and can affect joints in a more random way. It doesn’t have the same antibodies as rheumatoid arthritis.
Key differences between CPPD and rheumatoid arthritis include:
Getting the right diagnosis is key for treating CPPD or other arthritis types. It helps doctors choose the best treatment plan.
Managing acute CPPD attacks requires a mix of medicine, lifestyle changes, and sometimes, procedures. The aim is to lessen pain, swelling, and discomfort. This improves the patient’s life quality.
Managing pain is key in treating acute CPPD attacks. We suggest using both medicine and non-medicine methods to control pain well.
Anti-inflammatory drugs are vital in managing acute CPPD attacks. They reduce swelling, easing pain and discomfort.
NSAIDs are commonly used for acute CPPD attacks. They block the production of prostaglandins, which cause inflammation.
Joint aspiration and injections are procedures that help a lot during acute CPPD attacks.
Joint aspiration removes extra fluid from the joint, reducing pain and swelling. Sometimes, corticosteroid injections are given to the joint for more anti-inflammatory effects.
Rest and physical therapy are important for managing acute CPPD attacks. During flares, the joint needs rest to avoid more irritation.
Gentle physical therapy keeps the joint mobile and strong. We advise seeing a physical therapist for a custom exercise plan that fits the patient’s needs.
Managing CPPD arthropathy long-term needs a mix of preventive meds, lifestyle changes, and joint care. A good plan can lessen CPPD attacks, making life better for patients.
Preventive meds are key in fighting CPPD arthropathy. They cut down on attacks and slow the disease. Common ones include:
Table: Preventive Medications for CPPD Arthropathy
|
Medication |
Purpose |
Common Side Effects |
|---|---|---|
|
Colchicine |
Prevent acute attacks, reduce inflammation |
Gastrointestinal issues, muscle weakness |
|
NSAIDs |
Manage pain and inflammation |
Gastrointestinal issues, kidney damage |
|
Corticosteroids |
Reduce inflammation during acute attacks |
Weight gain, mood changes, increased blood pressure |
Changing your lifestyle is key in managing CPPD arthropathy. These changes can lower attack risks and boost health. Good changes include:
Keeping joints safe is critical for CPPD patients. Ways to do this include:
For severe CPPD, surgery might be needed. This can include:
By using meds, making lifestyle changes, protecting joints, and sometimes surgery, patients can manage CPPD well. This improves their life quality.
For those with CPPD arthritis, it’s key to manage the condition well. This means taking steps to control symptoms, keep joints healthy, and adjust to daily life changes.
Managing pain is a big part of living with CPPD. Here are some ways to do it:
“Pain management is not just about medication; it’s about adopting a holistic approach to well-being,” says Medical Expert, a rheumatologist. “By using different techniques, patients can better control their symptoms.”
Regular exercise is key for keeping joints mobile and reducing stiffness. Good activities include:
Always talk to a healthcare provider before starting any new exercise program to make sure it fits your needs and abilities.
There’s no special “CPPD diet,” but some diet changes can help. These include:
A recent study found that “Dietary interventions can play a significant role in managing chronic inflammatory conditions.”
Using assistive devices and making home changes can make daily life easier. Examples are:
By using these strategies, people with CPPD can live more active and fulfilling lives.
Understanding CPPD arthritis is key to improving life quality for those with it. Managing CPPD well needs a full approach. This includes medical care, lifestyle changes, and self-care.
Living with CPPD means handling both sudden attacks and ongoing joint problems. A broad care plan helps tackle CPPD’s challenges. This includes using pain relief, anti-inflammatory drugs, and injections.
Managing CPPD also means making lifestyle adjustments. This includes exercising, eating right, and using aids. Taking charge of CPPD can lessen its daily impact.
We stress the need for a detailed care plan for better CPPD outcomes. Working with healthcare and using self-care strategies can improve life quality. This way, people with CPPD can live better despite the condition.
CPPD arthritis, also known as calcium pyrophosphate deposition disease, is a type of arthritis. It happens when calcium pyrophosphate dihydrate crystals build up in the joints. This leads to joint pain and inflammation.
CPPD is a broader term that includes various conditions, including pseudogout. Pseudogout is a type of acute CPPD arthritis. It is known for sudden joint pain and swelling.
Symptoms of CPPD arthritis vary. But common signs include joint pain, stiffness, and swelling. These often affect the knees, hips, and wrists.
Diagnosing CPPD arthritis involves several steps. It includes a clinical evaluation, imaging studies, and joint fluid analysis. These help find calcium pyrophosphate dihydrate crystals.
For acute CPPD attacks, treatment options include pain management and anti-inflammatory medications. Joint aspiration and injections may also be used. Rest and physical therapy are recommended during flares.
Long-term management of CPPD arthritis includes preventive medications and lifestyle changes. Joint protection techniques and surgical interventions may be needed for severe cases.
To alleviate CPPD symptoms, maintaining a healthy weight and regular exercise are key. Dietary modifications can also improve joint health.
Yes, assistive devices like canes, walkers, and orthotics can aid in daily activities. They help individuals with CPPD arthritis move more easily and independently.
While there’s no cure for CPPD arthritis, a good treatment plan can manage symptoms. It can slow disease progression and improve quality of life.
CPPD arthritis is more common in older adults. Its prevalence increases with age, mainly after 60.
CPPD arthritis is different from other arthritis types like gout or osteoarthritis. It has unique causes, symptoms, and treatment methods.
Key What Is Calcium Pyrophosphate Deposition Disease & Treatment? https://www.ncbi.nlm.nih.gov/books/NBK540151/
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!