Last Updated on November 27, 2025 by Bilal Hasdemir

Robotic heart surgery has changed the medical world. It makes surgeries less invasive and helps patients recover faster. The first robotic-assisted heart surgeries took place in 1998 at the Hôpital Broussais in Paris and the Leipzig Heart Center in Germany.
Over the years, technology has improved greatly, allowing more precise and safer procedures. The keyhole open heart surgery early 2018 mrd number marked a significant step in the growth of robotic cardiac procedures, showing how advanced these methods had become.
This progress has led to better patient outcomes, reduced recovery time, and new opportunities for treating complex heart conditions with minimal invasion.
Key Takeaways
- Robotic heart surgery began in 1998.
- Pioneering centers were Hôpital Broussais and Leipzig Heart Center.
- The technology has improved patient outcomes.
- Robotic cardiothoracic surgery enables less invasive procedures.
- Recovery times are potentially quicker with robotic surgery.
The Evolution of Cardiac Surgery: From Open Procedures to Minimally Invasive Techniques

Cardiac surgery has changed a lot, moving from big open-heart surgeries to smaller, less invasive ones. This change is thanks to new technology and the goal of making patients heal faster and with less pain.
Traditional Open Heart Surgery: The Historical Standard
Old-school open-heart surgery needed a big cut in the chest to reach the heart. It worked well but had big downsides. Patients took longer to get better, felt more pain, and faced more risks.
The Shift Toward Minimally Invasive Approaches
Doctors wanted to make heart surgery less invasive. They came up with new methods using smaller cuts. This means less damage, less pain, and faster healing times. It’s a big win for patients.
Key Technological Advancements Enabling Less Invasive Cardiac Surgery
New tech has been key in making heart surgery less invasive. Robotic systems, like the Da Vinci Surgical System, are a big deal. They let surgeons do detailed work through tiny openings.
| Technological Advancement | Description | Impact on Cardiac Surgery |
| Robotic Surgery Systems | High-definition 3D visualization and precise robotic arms | Enhanced precision and control in complex procedures |
| Minimally Invasive Instrumentation | Specialized instruments for smaller incisions | Reduced tissue damage and trauma |
| Advanced Imaging Techniques | Improved preoperative and intraoperative imaging | Better visualization and planning of surgical procedures |
The move to less invasive heart surgery is a big step forward. It’s all thanks to new tech and the goal of better patient care. As we keep improving, the future of heart surgery looks bright.
The Birth of Robotic Surgery: Early Developments and Innovations
The journey of robotic surgery started with the first robotic surgical systems in the late 20th century. This time saw big tech leaps that set the stage for today’s surgery.
When Was Robotic Surgery Invented: The PUMA560 and Early Systems
The first robotic system, PUMA560, was used in 1985 for neurosurgical biopsies. This was a key moment in robotic surgery. It showed how robots could make surgery more precise and cut down recovery times.
In the late 1980s and 1990s, robotic surgical systems kept getting better. Many groups and companies worked on these advancements. These early systems were mainly for neurosurgery and orthopedics.
The Development of Telepresence Surgery in the 1990s
The 1990s brought a big leap with telepresence surgery. This tech let surgeons do operations from far away, using robots. It opened up new ways to help people, even in places far from hospitals.
FDA Approval and Early Clinical Applications
When the FDA approved robotic systems, it was a big step. The first approval was in the late 1990s. This made it easier for doctors to use these systems in real surgeries.
At first, robotic surgery was tested in clinical trials. These tests showed the systems were safe and worked well. As the tech improved, so did the types of surgeries robots could do, like heart surgeries.
First Applications in Cardiac Procedures: The Dawn of Robotic Heart Surgery
The first use of robotic tech in heart surgery changed the game. It was thanks to the teamwork of top heart surgeons and tech innovators.
Pioneering Cardiac Surgeons and Their Contributions
These surgeons brought their skills and worked with engineers. Together, they tackled the tech hurdles of robotic heart surgery. Their hard work led to better patient results and opened doors for more innovation.
First Robotic Heart Surgeries in the Early 2000s
The first robotic heart surgeries happened in 1998. This started a new chapter in heart surgery. These early surgeries tested if robotic systems could work in the OR.
“The introduction of robotic technology in cardiac surgery has been a game-changer, making surgery less invasive and leading to quicker recovery times.”
Initial Clinical Trials and Results
Early trials for robotic heart surgery looked at safety and benefits. The results were good, showing less trauma, less pain, and shorter stays for patients.
These trials set the stage for more use and research in robotic heart surgery. As the field grows, ongoing studies are key to improving techniques and expanding what can be done robotically.
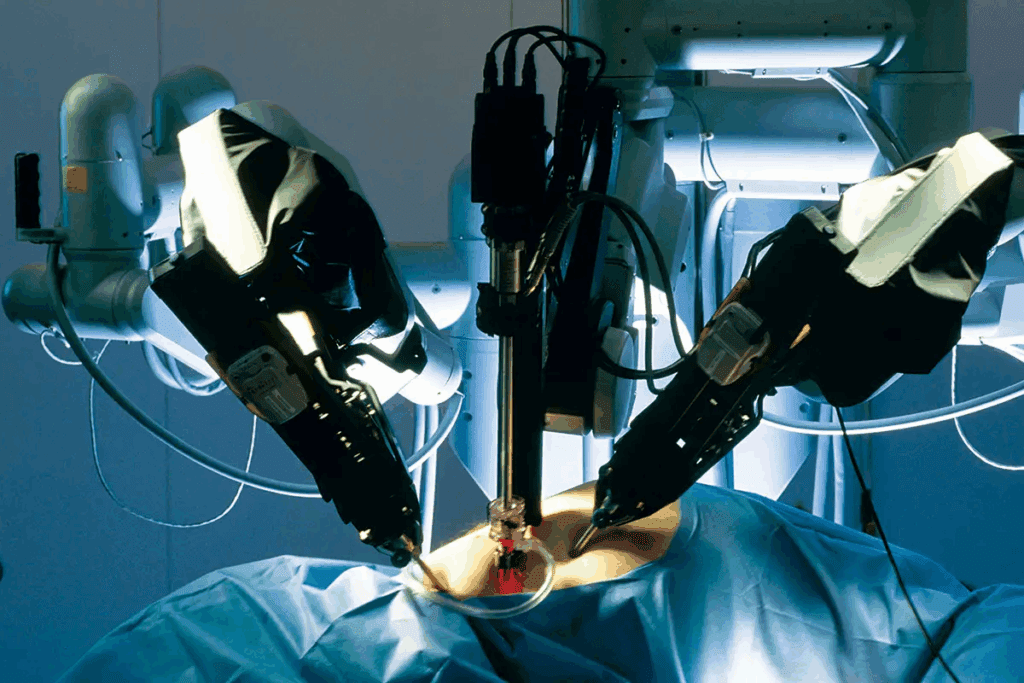
The Da Vinci Surgical System: Revolutionary Technology in Cardiac Surgery
The Da Vinci Surgical System is leading the way in cardiac surgery. It makes complex procedures more accurate. Surgeons can now do detailed heart operations with better precision and less invasiveness.
This means patients recover faster.
Operational Mechanism for Heart Procedures
The Da Vinci System works from a console where the surgeon controls the robotic arms. It offers a clear, 3D view of the surgical area. This setup helps with precise dissection and suturing, key in cardiac surgery.
Key Components:
- High-definition 3D vision system
- Robotic arms with precise instrumentation
- Surgeon console for control and visualization
Evolution of Da Vinci Models for Cardiac Applications
The Da Vinci System has evolved over the years. Each new model has improved its capabilities for cardiac surgery. The transition from the standard Da Vinci to the Da Vinci Si and Xi models has brought big improvements.
These include better visualization, ergonomics, and instrumentation.
| Model | Key Features | Cardiac Application Benefits |
| Da Vinci Standard | Initial robotic surgery platform | Introduced robotic cardiac surgery |
| Da Vinci Si | Improved HD vision, enhanced ergonomics | Better visualization, easier complex procedures |
| Da Vinci Xi | Advanced instrumentation, streamlined setup | Enhanced precision, reduced surgical time |
Comparison with Other Robotic Platforms for Heart Surgery
While the Da Vinci System is a top choice, other robotic systems are also used for cardiac surgery. A comparison shows differences in technology, application, and outcomes.
Comparative Analysis:
| Robotic System | Key Technology | Cardiac Surgery Outcomes |
| Da Vinci Xi | Advanced HD vision, precise instrumentation | High precision, reduced complications |
| Robotic System X | Enhanced flexibility, real-time feedback | Potential for improved outcomes, trials ongoing |
| CorPath GRX | Precision robotics for vascular procedures | High accuracy in coronary interventions |
Keyhole Open Heart Surgery: Early Techniques and 2018 MRD Number Breakthrough
Keyhole cardiac surgery is a major leap in heart surgery. It’s a less invasive way to fix heart problems. This method is changing how we do heart surgery, making it less harsh for patients.
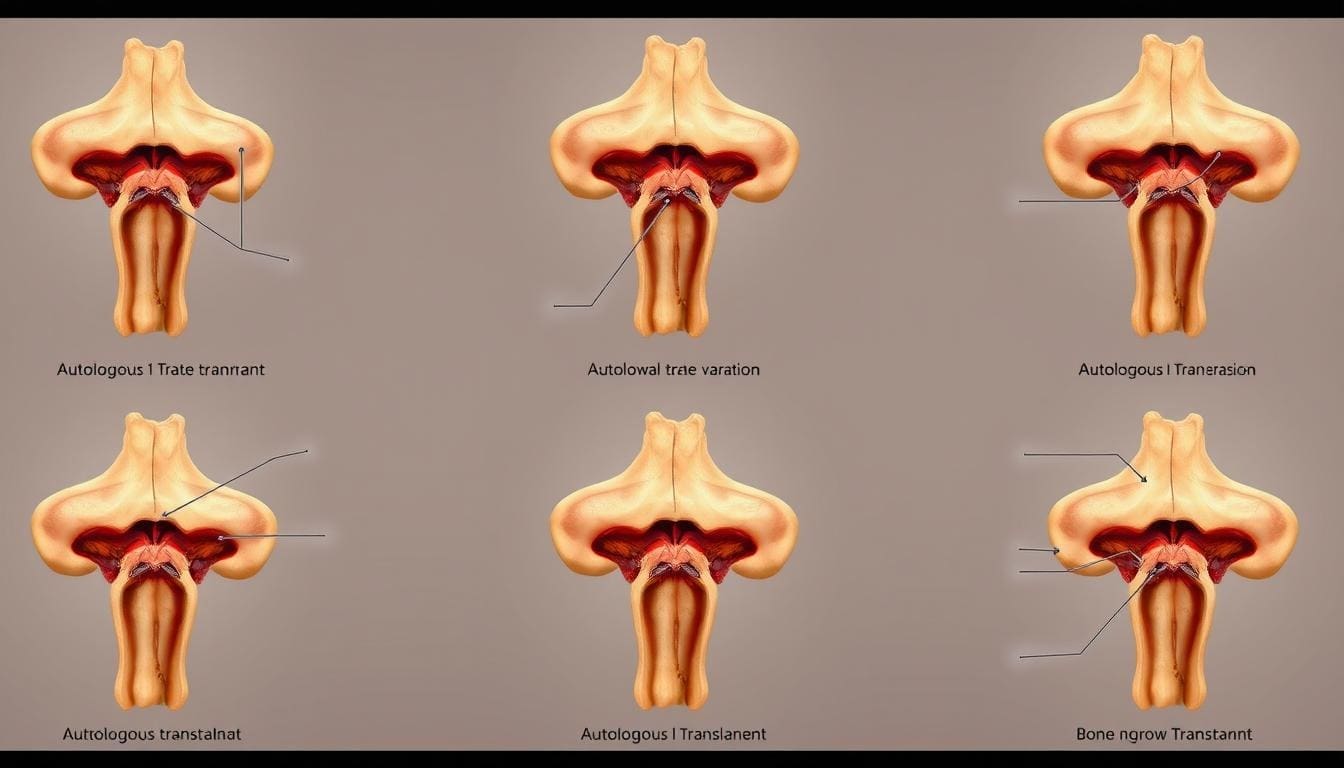
The Concept and Approach of Keyhole Cardiac Surgery
Keyhole surgery makes small cuts to get to the heart. It uses tools and a camera to fix heart issues. This method aims to cause less damage and help patients heal faster.
The idea behind keyhole surgery is to be as non-invasive as possible. Surgeons use special tools to work through small openings. This reduces risks and improves results for patients.
The Significance of the 2018 MRD Number Advancements
In 2018, a big step forward was made in keyhole surgery with MRD technology. MRD stands for Minimally Invasive Robotic Direct. It made surgeries more precise and less invasive.
“The integration of MRD technology in 2018 was a game-changer for cardiac surgery, enabling more precise and less invasive operations.”
A Cardiac Surgeon
Clinical Outcomes and Statistical Improvements
Studies show keyhole surgery has improved a lot, thanks to 2018’s MRD advancements. Patients have shorter recovery times, less pain, and fewer problems.
| Outcome Measure | Traditional Open Heart Surgery | Keyhole Open Heart Surgery (2018 MRD) |
| Average Recovery Time | 6-8 weeks | 3-4 weeks |
| Pain Levels (Scale: 1-10) | 7-8 | 4-5 |
| Complication Rate | 15% | 8% |
The numbers show big improvements. There’s less chance of complications and quicker healing. As it keeps getting better, more people might choose keyhole surgery for heart issues.
Robotic Cardiothoracic Surgery: Common Procedures and Applications
Robotic technology has made cardiothoracic surgery more advanced. It allows for more procedures to be done with less invasion. This leads to better results and faster healing for patients.
Mitral Valve Repair and Replacement
Mitral valve repair and replacement are key robotic surgeries. Robotic systems offer precise work, causing less damage to the area. This results in less pain and quicker healing for the patient.
Benefits of Robotic Mitral Valve Surgery:
- Smaller incisions
- Less blood loss
- Reduced risk of complications
- Shorter hospital stay
Coronary Artery Bypass Grafting (CABG)
CABG is vital for those with heart disease. Robotic CABG uses less invasive methods for more precise grafting. The robotic system’s advanced tools help surgeons work more accurately.
| Procedure | Traditional Method | Robotic Method |
| CABG | Large incision, longer recovery | Minimally invasive, quicker recovery |
| Mitral Valve Repair | Significant trauma, longer hospital stay | Less trauma, shorter hospital stay |
Atrial Septal Defect Repair and Other Congenital Heart Procedures
Robotic surgery is used for congenital heart defects like ASD repair. Its precision is key for delicate repairs in children and adults with heart defects.
Specialized Pediatric Applications
Pediatric heart surgery needs great precision because of the small size of children’s hearts. Robotic systems are used for some heart defects in kids. This could mean less invasive surgeries and faster healing.
The future of robotic cardiothoracic surgery looks bright. Ongoing research aims to improve results and expand what can be done robotically.
Patient Experience and Recovery After Robotic Heart Surgery
Patients who have robotic heart surgery often find their recovery smoother and less painful. This is because robotic surgery is less invasive. It means smaller cuts and less damage to the body.
Reduced Pain and Trauma Compared to Traditional Surgery
Robotic heart surgery cuts down on pain and trauma compared to open-heart surgery. The smaller cuts lead to less damage and pain after surgery. Studies show patients need less pain medicine and face fewer problems.
Shorter Hospital Stays and Recovery Timelines
Robotic heart surgery also means shorter hospital stays and quicker recovery. Patients heal faster and get back to their lives sooner. This makes patients happier and saves money on hospital costs.
Long-term Outcomes and Quality of Life Improvements
The long-term results for robotic heart surgery patients are good. They often have better heart function and quality of life. Long-term studies show the benefits last for years, making it a great choice for heart surgery.
Training and Expertise: Becoming a Robotic Cardiac Surgeon
Robotic cardiac surgery needs surgeons to get a lot of training and specific skills. The complex nature of heart surgeries and the advanced tech of robots require a deep education and skill building.
Learning Curve and Specialized Training Requirements
The learning curve for robotic cardiac surgery is steep. Surgeons must first learn traditional heart surgery techniques. Then, they move to robotic-assisted surgeries.
Specialized training programs, given by robot makers, offer hands-on and classroom learning. These programs include simulation training, watching experienced surgeons, and doing surgeries under supervision. The goal is to reduce risks and make sure surgeons are good at robotic heart surgery.
Certification and Credentialing Processes
Certification and credentialing are key to making sure surgeons are ready for robotic heart surgery. Each place might have its own rules, but they usually follow the same steps.
- Finish a recognized robotic surgery training program
- Watch and be supervised by a skilled robotic heart surgeon
- Do a certain number of surgeries to show you can do it
- Keep your certification by learning more and following best practices
Volume-Outcome Relationship in Robotic Cardiac Surgery
The link between how many surgeries you do and your results is true in heart surgery. For robotic heart surgery, doing a lot of cases helps keep your skills sharp and improves patient results.
| Volume Category | Average Annual Cases | Mortality Rate (%) | Complication Rate (%) |
| Low Volume | < 20 | 2.5 | 10 |
| Medium Volume | 20-50 | 1.8 | 7 |
| High Volume | > 50 | 1.2 | 4 |
The table shows that doing more surgeries leads to better results. This highlights the need for constant training and high standards in robotic heart surgery.
Current Challenges and Future Innovations in Robotic Heart Surgery
Robotic heart surgery is growing but faces technical and cost hurdles. Despite these, new technologies are set to bring big changes.
Technical Limitations and Areas for Improvement
Robotic heart surgery is a big leap forward but has some technical issues. It needs better dexterity, clearer visuals, and more touch feedback. Even with advanced systems, there’s room for better tools and techniques.
Key technical limitations include:
- Limited tactile feedback
- High initial investment
- Need for specialized training
Fixing these problems is key for robotic heart surgery to grow and be accepted more.
Cost Considerations and Healthcare Economics
The cost of robotic heart surgery is a big factor. It includes the price of the equipment, upkeep, and disposable items. But, it can save on hospital stays and recovery times, making it more cost-effective.
| Cost Component | Traditional Surgery | Robotic Surgery |
| Initial Hospital Stay | $15,000 | $10,000 |
| Recovery Time Costs | $8,000 | $4,000 |
| Equipment and Maintenance | $0 | $5,000 |
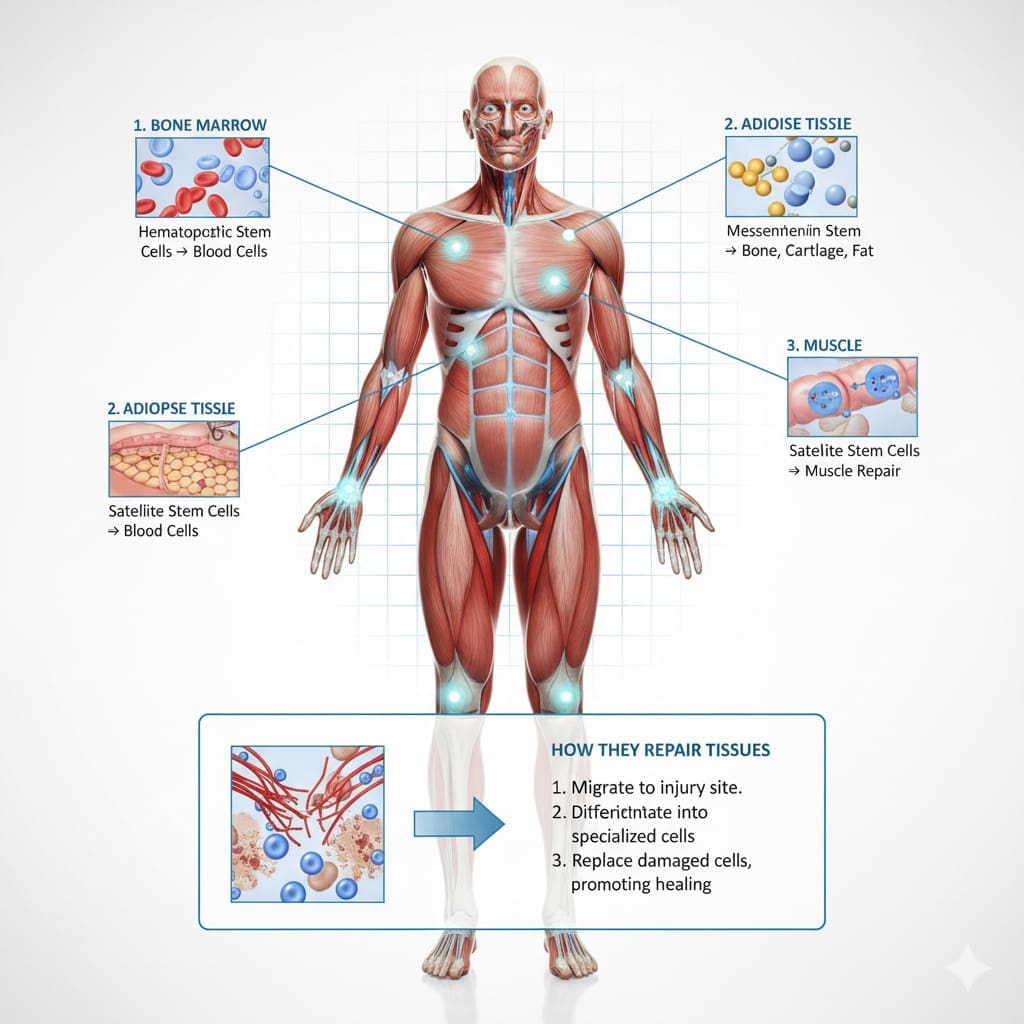
Emerging Technologies: AI, Augmented Reality, and Remote Surgery
New tech like AI, AR, and remote surgery is changing robotic heart surgery. They promise better precision, outcomes, and access.
AI can look at past surgeries to predict and suggest the best methods. AR gives surgeons real-time data, helping them make accurate decisions.
Remote surgery lets doctors operate from anywhere, making top-notch care more available. This could make surgery more accessible worldwide.
These new technologies will likely lead to big improvements in robotic heart surgery. They will help patients get better results and make surgery more available.
Conclusion
Robotic heart surgery has made big strides, changing cardiac surgery a lot. It moved from old open-heart surgeries to new, less invasive ways. This has made patients recover faster and do better overall.
The Da Vinci Surgical System and other robots are key to this change. They let surgeons do tricky heart surgeries with more skill and less harm. This means patients feel less pain and have less damage.
As robotic heart surgery gets better, we’ll see even more progress. New tech like AI and augmented reality will help a lot. They will make surgeries even more precise and safe.
Robotic heart surgery is becoming a big part of modern cardiac surgery. It will keep getting better, leading to even better care for patients. This makes it a very important part of heart surgery today.
FAQ
What is robotic heart surgery?
Robotic heart surgery is a new way to do heart operations. It uses a robotic system, like the Da Vinci Surgical System. This method helps doctors do complex surgeries with more precision and accuracy.
When was robotic surgery invented?
The first robotic surgical system, PUMA 560, was made in the 1980s. But, the Da Vinci Surgical System and others were approved by the FDA in the late 1990s and early 2000s.
What are the benefits of robotic heart surgery?
Robotic heart surgery has many benefits. It causes less pain and trauma. Patients also have shorter hospital stays and better long-term health compared to traditional surgery.
What procedures can be performed using robotic cardiothoracic surgery?
Robotic cardiothoracic surgery can do many procedures. This includes fixing mitral valves, doing coronary artery bypass grafting (CABG), and repairing atrial septal defects. It also helps with congenital heart problems.
How does the Da Vinci Surgical System work?
The Da Vinci Surgical System is a robotic platform. It lets surgeons do complex surgeries with better precision and accuracy. It has a surgeon’s console, a patient-side cart, and a vision system. This setup allows for detailed dissection, suturing, and tissue manipulation.
What kind of training is required to become a robotic cardiac surgeon?
To be a robotic cardiac surgeon, you need special training. This includes a learning curve, certification, and credentialing. You also need to meet specific volume requirements to stay skilled.
What are the current challenges in robotic heart surgery?
Robotic heart surgery faces some challenges. These include technical limitations and cost. There’s also a need for better technology and innovation. New technologies like AI and augmented reality are being explored.
What is the future of robotic heart surgery?
The future of robotic heart surgery looks bright. Advances in technology, like AI and augmented reality, are expected. These will likely improve outcomes, lower costs, and make robotic cardiac surgery more accessible.
References
- Chitwood, W. R., Jr. (2013). Historical evolution of robot-assisted cardiac surgery. Annals of Cardiothoracic Surgery, 1(4), 340-349. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9723535/