At Liv Hospital, we know how a lumbar vertebrae fracture can change your life. An L1 spinal fracture happens in the lower back. It’s often caused by trauma or osteoporosis.
These fractures can make your back hurt a lot and make it hard to move. In bad cases, they can even hurt nerves. Knowing about the causes, symptoms, and treatments is key for a good recovery.
We’re dedicated to top-notch healthcare with full support for international patients. Our focus on you and our advanced spine care mean you get the best treatment.
Key Takeaways
- Understanding the causes and symptoms of L1 vertebrae fractures is essential for effective treatment.
- L1 spinal fractures can result from trauma or osteoporosis, leading to severe back pain and limited mobility.
- Comprehensive care and support are vital for safe and effective recovery.
- Liv Hospital offers advanced spine care with a patient-centered approach.
- Timely medical intervention can greatly improve outcomes for patients with lumbar vertebrae fractures.
Understanding the Anatomy and Function of the Lumbar Spine
To understand an L1 vertebrae fracture, we must first know about the lumbar spine. It’s in our lower back and has five vertebrae, from L1 to L5. This part of our spine is key to our body’s structure.
The lumbar spine supports our body’s weight and allows us to move. It also protects the spinal cord. Its shape helps spread out the weight we carry.
Location and Role of L1 Vertebrae
The L1 vertebra is at the top of the lumbar spine. It’s important because it connects the thoracic spine to the lumbar spine. This vertebra takes a lot of our body’s weight and faces many stresses.
Key characteristics of the L1 vertebra include:
- It is the largest and strongest of the lumbar vertebrae.
- It has a large vertebral body that supports much of the weight.
- The L1 vertebra facilitates flexion, extension, and rotation movements.
Relationship to Thoracolumbar Junction
The thoracolumbar junction is where the T12 and L1 meet. It’s a spot where the spine changes from being less mobile to more mobile. This area is prone to injuries because of the stress it faces.
| Characteristics | Thoracic Spine | Lumbar Spine |
| Mobility | Less mobile due to rib cage support | More mobile, facilitating bending and twisting |
| Vertebral Size | Smaller vertebral bodies | Larger vertebral bodies to support more weight |
Knowing about the lumbar spine, L1 vertebra, and the thoracolumbar junction is key. It helps doctors diagnose and treat injuries in this area.
What Exactly Is an L1 Vertebrae Fracture?
The L1 vertebrae is at the top of the lower back. It can break due to accidents, weak bones, or diseases. This break can really affect how well you live.
These fractures can be different, like compression fractures, burst fractures, and fracture-dislocations. Knowing the type helps doctors choose the right treatment.
Types of L1 Fractures: Compression, Burst, and Fracture-Dislocations
L1 vertebrae fractures can be classified into several types based on the nature of the injury:
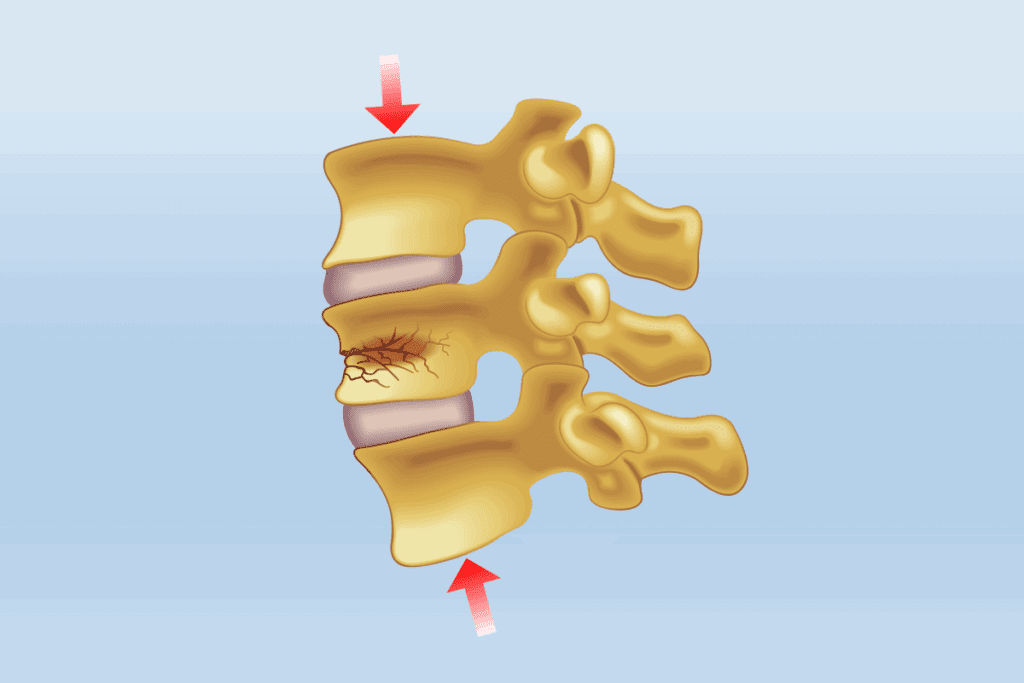
- Compression Fractures: These happen when the vertebra collapses, often in weak bones.
- Burst Fractures: These are more serious, where the vertebra breaks apart and might hurt the spinal canal.
- Fracture-Dislocations: This type has both a fracture and the vertebra moving out of place, leading to instability.
Each fracture type needs a different treatment plan for recovery.
Stability vs. Instability in Spinal Fractures
How stable the fracture is matters a lot for treatment. Stable fractures are less likely to get worse or cause more harm. Unstable fractures are at higher risk of causing nerve damage or deformity.
| Fracture Type | Stability | Typical Treatment |
| Compression Fracture | Stable | Conservative Management |
| Burst Fracture | Unstable | Surgical Intervention |
| Fracture-Dislocation | Unstable | Surgical Stabilization |
A spine specialist says, “Knowing if a fracture is stable or unstable is key. It decides if you need to just rest or surgery.”
“The key to managing L1 vertebrae fractures lies in accurately assessing the fracture’s stability and selecting the most appropriate treatment strategy.”
Spine Specialist
It’s important for doctors to know the details of an L1 vertebrae fracture. This helps them give the best treatment. Patients then get care that meets their specific needs and helps them recover better.
Primary Causes and Risk Factors
Traumatic injuries, osteoporosis, and certain diseases can cause L1 vertebrae fractures. Knowing these causes helps us spot who’s at risk. It also guides us in how to prevent these fractures.
Traumatic Injuries in Younger Populations
In younger people, traumatic injuries often lead to L1 vertebrae fractures. These injuries might come from car accidents, falls, or sports injuries. The strong impact can break the L1 vertebra.
Osteoporosis and Age-Related Bone Loss
Osteoporosis makes bones weaker and more likely to break, mainly in older adults. As we age, our bones lose density, making them even more fragile.
Pathological Fractures and Underlying Conditions
Pathological fractures happen when a disease or condition weakens the bones. This can include bone cancer, osteomyelitis, or metabolic bone diseases. These conditions raise the risk of fractures in the L1 vertebra.
The table below lists the main causes and risk factors for L1 vertebrae fractures:
| Cause/Risk Factor | Description | Population Most Affected |
| Traumatic Injuries | High-energy events causing spinal fractures | Younger individuals |
| Osteoporosis | Bone density loss increasing fracture risk | Older adults |
| Pathological Conditions | Underlying diseases weakening bone structure | Variable, depending on the condition |
Understanding these causes and risk factors is key. It helps us create better prevention and treatment plans for L1 vertebrae fractures.
Key Symptoms and Warning Signs
It’s important for both patients and doctors to know the signs of L1 vertebrae fractures. Spotting these symptoms early can help get the right treatment fast. This is key to avoiding more serious problems.
Acute Pain Patterns and Location
The main sign of an L1 vertebrae fracture is sharp pain in the lower back. This pain can be very strong and usually happens right where the fracture is. It might get worse when you move, cough, or sneeze, and sometimes spreads to the belly or groin.
Characteristics of acute pain associated with L1 vertebrae fractures include:
- Sharp or stabbing pain in the lower back
- Pain that worsens with movement or activity
- Pain that may radiate to the abdomen or groin
Neurological Symptoms and Red Flags
L1 vertebrae fractures can also cause nerve problems. This might lead to numbness, tingling, or weakness in the legs. If the fracture presses on nerves too much, it can cause even more serious problems.
Red flags that indicate a need for immediate medical attention include:
- Sudden onset of numbness or tingling in the legs
- Progressive weakness in the lower extremities
- Loss of bladder or bowel control
Progressive Symptoms in Untreated Cases
If not treated, L1 vertebrae fractures can get worse. This can lead to more pain, a crooked spine, and nerve problems. Without treatment, these fractures can cause long-term pain and disability.
The table below shows what can happen if these fractures are not treated:
| Symptom/Complication | Description | Potential Impact |
| Increased Pain | Worsening pain over time | Reduced quality of life |
| Deformity | Progressive kyphosis or spinal deformity | Chronic pain, disability |
| Neurological Deterioration | Worsening neurological symptoms | Potential for permanent nerve damage |
Knowing the signs of L1 vertebrae fractures is key to getting help quickly. By recognizing these symptoms, patients can get the care they need. This can help prevent serious long-term problems.
Diagnostic Process for L1 Compression Fractures
Diagnosing an L1 compression fracture is a detailed process. It starts with a careful first check. We know finding the right diagnosis is key to choosing the best treatment.
Initial Assessment and Physical Examination
The first step is a detailed medical history and physical check. We look at the patient’s symptoms, past health, and how the injury happened. A physical exam also checks for nerve problems or spine instability.
During the physical exam, we check for:
- Localized pain or tenderness
- Deformity or abnormal curvature of the spine
- Neurological symptoms such as numbness, weakness, or tingling in the legs
- Any limitations in mobility or flexibility
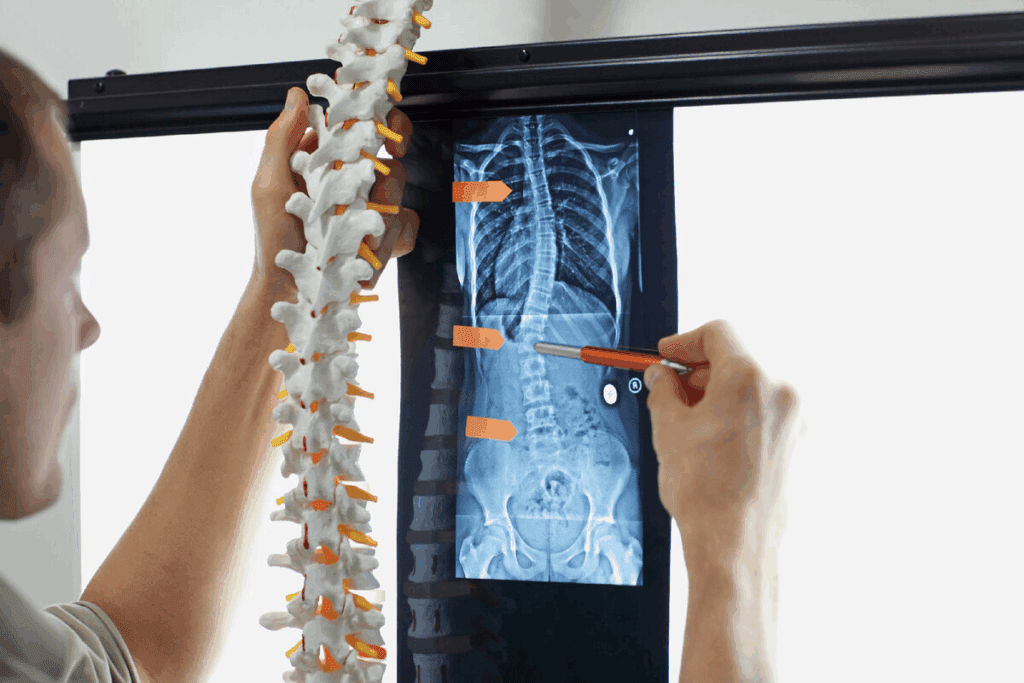
Imaging Studies: X-rays, CT, and MRI Findings
Imaging studies are vital for confirming the diagnosis and understanding the fracture’s severity. We use different imaging methods to get a full picture of the spine’s condition.
Key imaging studies include:
- X-rays: First look at vertebral alignment and fracture
- CT scans: Detailed bone structure and fracture severity
- MRI: Soft tissue damage, neurological compression, and spinal stability
Assessing Fracture Severity and Stability
After confirming the diagnosis, we evaluate the fracture’s severity and stability. We look at how much the vertebral body has collapsed, the state of the posterior ligamentous complex, and any nerve issues.
Factors influencing fracture severity include:
- Percentage of vertebral body height loss
- Presence of kyphotic deformity
- Involvement of the posterior wall of the vertebral body
- Any retropulsion of fracture fragments into the spinal canal
By combining clinical findings with advanced imaging, we can accurately classify the fracture. This helps us choose the best treatment plan.
Conservative Treatment Options for L1 Vertebrae Fracture
When it comes to L1 vertebrae fractures, we often start with conservative treatments. These methods are chosen to avoid more serious procedures. They are effective in managing the fracture without surgery.
Bed Rest and Activity Modification
Bed rest and changing how you move are key parts of treatment. They help the fractured vertebra heal by reducing stress. It’s important to avoid heavy lifting and bending to prevent making the fracture worse.
Bracing Techniques and Duration
Bracing is also a big part of treatment. Bracing techniques keep the spine stable, which helps with healing. How long you need to wear a brace depends on the fracture’s severity and your health. Usually, it’s for 6 to 12 weeks.
Pain Management Approaches
Managing pain is critical for those with L1 vertebrae fractures. We use medicines, physical therapy, and other methods like acupuncture or chiropractic care. These help control pain and improve life quality.
Monitoring Healing Progress
It’s important to keep an eye on how the fracture is healing. We use checks and scans to track progress. This lets us make changes to the treatment plan if needed.
With a detailed conservative treatment plan, we can manage L1 vertebrae fractures well. This helps patients recover and get their spinal health back.
Physical Therapy and Rehabilitation Protocols
Physical therapy is key in treating L1 vertebrae fractures. It helps patients get better. A good rehab plan is important for strength, mobility, and function. This improves patients’ lives.
Early Mobilization Strategies
Starting to move early is vital in rehab. We suggest gentle exercises and slow movements. This stops stiffness and helps healing.
Early movement boosts blood flow, lessens muscle loss, and aids bone healing. We adjust these strategies based on each patient’s needs and fracture stability.
Core Strengthening and Stabilization Exercises
Strengthening the core is essential for spine support and stability. We focus on exercises that build abdominal and back muscles. These muscles keep the spine aligned and prevent injuries.
A sample core strengthening program might include:
| Exercise | Repetitions | Sets |
| Plank | 30 seconds | 3 |
| Bridging | 15 | 3 |
| Pelvic Tilt | 10 | 3 |
Long-term Rehabilitation Goals
Our long-term goals for patients with L1 vertebrae fractures are full recovery, less pain, and better function. We help set realistic goals and create a detailed plan to reach them.
Rehab plans are customized based on progress. They may include advanced exercises, manual therapy, and education on body mechanics. Our aim is to give patients the tools for a healthy, active life.
Minimally Invasive Procedures for Compression Fractures
Minimally invasive procedures have changed how we treat compression fractures. They offer relief with fewer side effects. These new methods are now a top choice for treating painful vertebral compression fractures.
Vertebroplasty: Procedure and Outcomes
Vertebroplasty is a minimally invasive procedure. It involves injecting bone cement into a fractured vertebra. This makes the vertebra stronger and can help with pain and mobility.
The procedure is done under local anesthesia and sedation. This helps patients recover fast. Research shows vertebroplasty can reduce pain right away. But, the long-term effects are being studied more.
Kyphoplasty: Technique and Benefits
Kyphoplasty is another minimally invasive technique for treating vertebral compression fractures. It creates a space in the fractured vertebra before filling it with bone cement. This helps restore the vertebra’s height and corrects kyphotic deformity.
Kyphoplasty offers pain relief and can also help restore some lost height. This can improve spinal alignment and lower the risk of future problems.
Patient Selection for Minimally Invasive Interventions
Choosing the right patients for minimally invasive procedures like vertebroplasty and kyphoplasty is key. The fracture’s severity, any neurological symptoms, and the patient’s health are important factors.
These procedures are best for patients with painful osteoporotic compression fractures that haven’t improved with other treatments. A healthcare professional must evaluate each patient to find the best treatment.
Surgical Interventions for Unstable L1 Fractures
Surgery is often needed for unstable L1 vertebrae fractures. These fractures can risk the spine’s stability and health. When the fracture is complex or there are signs of neurological issues, surgery is key to fix the spine and avoid more problems.
Indications for Surgical Management
Doctors decide on surgery based on several factors. These include the fracture’s severity, any neurological problems, and the patient’s overall health. Unstable fractures that can’t be treated without surgery need it to stop the spine from getting worse and to prevent nerve damage.
Here are some reasons for surgery:
- Significant spinal instability or deformity
- Neurological deficits or progressive neurological decline
- Severe compression or burst fractures with significant bone fragments compromising the spinal canal
- Failure of conservative management to achieve adequate pain control or spinal stability
Spinal Fusion and Instrumentation Techniques
Surgery for unstable L1 fractures often includes spinal fusion and instrumentation techniques. Spinal fusion joins vertebrae together using bone grafts. These can come from the patient or a donor.
Instrumentation, like rods, screws, and plates, adds extra stability. It helps correct deformities, reduce fragments, and keep the spine aligned.
Recovery Timeline and Rehabilitation After Surgery
The recovery time and rehabilitation process vary. It depends on the surgery’s complexity and the patient’s health. Patients usually stay in the hospital for a few days after surgery.
Post-operative rehabilitation is key for the best results. It involves a team of physical therapists, pain managers, and follow-up doctors. The process includes:
- Early mobilization and physical therapy to restore strength and mobility
- Pain management strategies to control post-operative pain
- Monitoring for possible complications and managing them quickly
- Gradual return to normal activities, with guidance on safe lifting and bending techniques
Knowing the surgical options for unstable L1 fractures helps patients and doctors make the right treatment choices. This aims to fix the spine, reduce pain, and improve life quality.
Complications of Untreated L1 and Related Vertebral Fractures
Ignoring L1 vertebrae fractures can cause chronic pain and deformity. These issues can be severe and last a long time. They affect not just the spine but also overall health and happiness.
Collapse of Lumbar Vertebrae and Progressive Deformity
The collapse of lumbar vertebrae, like at L1 or L2, can cause kyphosis. This is when the spine curves abnormally. It can make you look shorter and cause chronic pain because of how the spine works.
Kyphosis makes daily life hard. It can also get worse over time if not treated.
Compression Fractures at T12-L1 and Adjacent Levels
Fractures at T12-L1 can lead to more fractures nearby. This is because the spine’s stress changes after a fracture.
This increases the risk of more fractures. It can start a cycle of degeneration and more problems, like more kyphosis and pain.
Chronic Pain and Functional Limitations
Untreated vertebral fractures often lead to chronic pain. This pain can come from the fracture, the deformity, or the strain on muscles and other parts of the body.
People with these fractures may also have trouble moving around. Chronic pain and spinal deformity can limit how well you can do daily tasks.
Effective management of vertebral fractures is key. It helps avoid these problems and ensures the best results for patients.
Prevention Strategies and Long-term Management
Managing L1 vertebrae fractures long-term means using many strategies. These help keep bones strong and prevent falls. This approach not only makes life better for patients but also lowers the chance of more fractures.
Osteoporosis Treatment and Bone Health Optimization
It’s key to manage osteoporosis to stop future fractures. This includes making lifestyle changes, eating right, and using medicine.
Make sure to get enough calcium and vitamin D. These are key for strong bones. Medicine like bisphosphonates, SERMs, and parathyroid hormone analogs can also help. They make bones stronger and lower the risk of breaking them.
| Osteoporosis Treatment Options | Description | Benefits |
| Bisphosphonates | Reduce bone resorption | Decrease fracture risk |
| SERMs | Mimic estrogen’s effect on bone density | Maintain bone health |
| Parathyroid Hormone Analogs | Stimulate bone formation | Increase bone density |
Fall Prevention and Safety Measures
Stopping falls is just as important as treating fractures. We tell patients to take steps to stay safe every day.
Removing things that could trip you, putting up handrails, and better lighting can help a lot. Also, exercises like tai chi can improve balance and strength.
Follow-up Care and Monitoring
Seeing a doctor regularly is vital for checking on L1 vertebrae fractures. It helps track healing and catch any problems early. This ensures the best care for patients.
Keeping an eye on things lets us act fast if needed. This helps patients get the best results from their treatment.
Conclusion: Navigating Recovery and Improving Quality of Life
Recovering from an L1 vertebrae fracture needs a deep understanding of treatment and ways to better life quality. We’ve looked into the details of lumbar vertebrae fractures. This includes their causes, symptoms, andhow to treat them.
Getting better means fixing the fracture and keeping bones strong. Knowing how to diagnose, treat, and rehab is key. This helps people regain their strength and move freely again.
Our institution is dedicated to top-notch healthcare and supporting patients fully. Our team helps patients through their recovery. We make sure they get the care and advice they need to live better after an L1 vertebral fracture.
FAQ
What is an L1 vertebrae fracture?
An L1 vertebrae fracture is a break in the first lumbar vertebra. It can happen from trauma, osteoporosis, or other health issues.
What are the symptoms of an L1 vertebrae compression fracture?
Symptoms include sharp back pain and trouble moving. In bad cases, you might feel numbness or weakness in your legs.
How is an L1 vertebrae fracture diagnosed?
Doctors use a physical check, X-rays, CT scans, and MRI to find out how bad the fracture is.
What are the treatment options for an L1 vertebrae fracture?
Treatment can be simple, like resting and using a brace. Or it might need more, like vertebroplasty or surgery.
What is the difference between a stable and unstable L1 vertebrae fracture?
A stable fracture doesn’t move much. An unstable one does, which can hurt your spine’s stability.
Can osteoporosis lead to an L1 vertebrae compression fracture?
Yes, osteoporosis makes bones weak. This increases the chance of a fracture in the L1 vertebra.
What is the role of physical therapy in recovering from an L1 vertebrae fracture?
Physical therapy is key in getting better. It helps with moving, strengthening, and stabilizing exercises.
What are the possible complications of untreated L1 vertebrae fractures?
Not treating can cause more problems. These include a crooked spine, constant pain, and even nerve damage.
How can future vertebral fractures be prevented?
To prevent fractures, manage osteoporosis, keep bones strong, avoid falls, and see your doctor regularly.
What is the recovery timeline for surgical treatment of an L1 vertebrae fracture?
Recovery time varies. It depends on the surgery and how well you heal. It usually takes months of care and exercise.
Are minimally invasive procedures effective for treating L1 compression fractures?
Yes, vertebroplasty and kyphoplasty can help. They stabilize the fracture and ease pain for some patients.
How does the location of the fracture, such as at the thoracolumbar junction, affect treatment?
The fracture’s location matters. Fractures at the thoracolumbar junction need special care because of the area’s unique anatomy and movement.
Reference
- Eastell, R., Rosen, C. J., Black, D. M., et al. (2019). Pharmacological management of osteoporosis in postmenopausal women: An Endocrine Society Clinical Practice Guideline. The Journal of Clinical Endocrinology & Metabolism, 104(5), 1595-1622. https://academic.oup.com/jcem/article/104/5/1595/5418884


































