Understanding the left anterior descending artery, also known as the lad heart, is key to knowing how the heart works.
The anterior interventricular artery, or left anterior descending artery, is very important. It helps supply blood to the front part of the left ventricle and the wall between the ventricles.
At Liv Hospital, we know how vital the lad heart is for heart health. We use the latest care and research to help our patients get the best treatment.

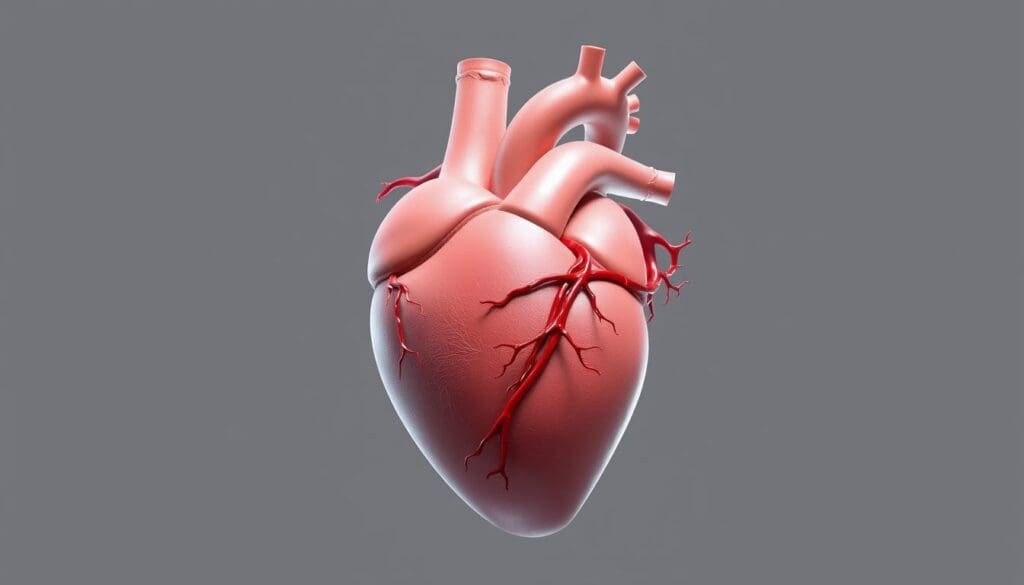
The anterior interventricular artery, known as the LAD heart, is key to heart function. It’s a main branch of the left coronary artery. It runs along the anterior interventricular sulcus to the heart’s apex.
The LAD heart is the anterior interventricular branch of the left coronary artery. It sits in the anterior interventricular sulcus, a groove on the heart’s surface. This groove separates the ventricles. The LAD supplies blood to a big part of the left ventricle and the front two-thirds of the interventricular septum.
The LAD heart is vital for blood flow to the heart muscle. It delivers oxygen-rich blood, which is key for the heart’s electrical system and function. The coronary artery supply, including the LAD, makes sure the heart muscle gets the oxygen and nutrients it needs.
The LAD is a key branch of the left coronary artery. It runs along the anterior interventricular sulcus. This artery is vital for the heart’s oxygen supply. Knowing its path is key for diagnosing and treating heart issues.
The LAD starts from the left coronary artery. This artery splits into the LAD and the left circumflex artery. Its start is important because it begins a vital path for the heart’s left ventricle and septum.
The LAD follows the anterior interventricular sulcus. This groove is between the left and right ventricles. Along this way, it branches to the left ventricle’s front and the septum. This path is key for delivering oxygen to the heart’s most critical areas.
The LAD’s end can vary among people. It usually reaches the heart’s apex. Sometimes, it also covers the heart’s bottom. Knowing these patterns helps doctors plan treatments for heart disease.
The LAD is key in supplying blood to the left ventricle, mainly the anterior wall. It’s vital for the heart’s left ventricle health. This part pumps oxygenated blood all over the body.
The LAD feeds the anterior wall of the left ventricle through its diagonal branches. These branches differ in size and number but are vital. They ensure the anterior wall gets enough oxygen and nutrients.
This supply is critical because the anterior wall is key for the left ventricle’s pumping. Any issue with blood supply here can cause serious heart problems.
The LAD also supplies the interventricular septum, the wall between the left and right ventricles. Its septal branches are essential for this. Proper perfusion here is vital for normal heart function and rhythm.
The septal branches of the LAD are key for the heart’s conduction system. This includes the bundle of His and the bundle branches. They are vital for coordinated ventricular contraction.
To show the LAD’s role in the left ventricle, let’s look at its branches and what they supply:
| Branch | Area Supplied | Function |
| Diagonal Branches | Anterior ventricular wall | Supports left ventricular contraction |
| Septal Branches | Interventricular septum | Nourishes the conduction system |
In summary, the LAD’s role in supplying nearly half of the left ventricle is critical. Its branches ensure the anterior wall and the interventricular septum get the blood they need. This is essential for optimal heart function.
Knowing about the LAD’s branches is key to understanding heart health. The LAD artery is more than just a blood path. It has many branches that feed different parts of the heart muscle.
The septal branches of the LAD are vital for the heart’s electrical system. They supply blood to the septum, where the heart’s electrical signals start. This ensures the heart beats correctly.
Key Functions of Septal Branches:
The diagonal branches of the LAD artery run along the left ventricle’s surface. They give vital blood to this area. These branches vary but are key for the heart’s health.
| Branch | Region Supplied | Function |
| Septal Branches | Interventricular Septum | Nourishes the heart’s electrical system |
| Diagonal Branches | Anterolateral Myocardium | Supports the muscular function of the left ventricle |
In conclusion, the LAD’s branches are essential for heart health. Knowing about them helps in diagnosing and treating heart disease.
The “widow-maker” phenomenon is a severe blockage in the LAD artery. It can have very bad consequences. This is because the LAD artery is key to the heart’s blood supply.
A blockage in the proximal LAD artery is called a “widow-maker.” It can cause a lot of damage to the heart muscle. When this happens, a big part of the heart’s front and sometimes the bottom gets hurt.
The effects of such a blockage are serious. They can include:
Proximal LAD occlusions are very dangerous. They affect a big part of the heart. The LAD artery supplies almost half of the left ventricle. When it’s blocked, the heart can suffer a lot.
There are several things that can make you more likely to have an LAD occlusion. These include:
Knowing these risk factors can help prevent and treat LAD occlusions early. This could save lives.
It’s key for healthcare pros to know the different names for the LAD. This artery is called by many names, showing its big role in heart anatomy.
The LAD is also known as the anterior descending coronary artery, left arterial descending, and left artery descending. These names are used the same way in medical texts. But, some texts might make small differences between them.
Many names for the LAD come from its history and how it’s shaped. Its name comes from where it starts and how it runs. Knowing these names helps us understand medical texts better and talk clearly in hospitals.
In hospitals, “LAD” is the most used term because it’s short and clear. But, knowing other names is important too. You might see them in patient files, imaging reports, or when talking to other doctors.
Knowing these synonyms helps us talk better about this important artery. This improves care for our patients.
Seeing the LAD clearly is key for good heart care. Imaging helps spot and treat heart disease, focusing on the anterior interventricular artery.
Coronary angiography is top for seeing the LAD. It’s a detailed test that uses a contrast agent to show the arteries. This helps us figure out the best treatment.
A study in the Journal of the American College of Cardiology shows its value. It gives clear images of the arteries, helping us plan treatments for LAD disease.
“Coronary angiography is indispensable for diagnosing and treating coronary artery disease, specially when it comes to the LAD.”
CT coronary angiography is a non-invasive option. It uses CT scans to see the arteries, including the LAD, without needing to go inside. We use it for those who can’t have invasive tests or as a first look.
Adding 3D to CT scans helps us see the LAD’s shape and how it fits with other parts. This is key for planning surgeries.
| Imaging Technique | Invasiveness | Resolution |
| Coronary Angiography | Invasive | High |
| CT Coronary Angiography | Non-invasive | High |
Understanding LAD diagrams is vital. They show the LAD’s shape and any problems. We use them to spot disease, plan treatments, and check how well treatments work.
For example, a detailed diagram can show where and how bad stenoses are. This helps us choose the best treatment.
By using advanced imaging and our knowledge, we give the best care for LAD disease. This improves patients’ lives and outcomes.
Understanding LAD pathologies is key to diagnosing and treating heart diseases. The LAD artery is vital for the heart’s blood supply. Any issues with it can be serious.
Atherosclerosis is a common problem with the LAD. It’s when plaque builds up in the artery walls, causing narrowing or blockage. This can severely cut down blood flow to the heart, leading to pain, heart attacks, or even death.
Risk factors for atherosclerosis of the LAD include high cholesterol, high blood pressure, diabetes, and smoking. It’s important to manage these risks to prevent the disease from getting worse.
| Risk Factor | Description | Impact on LAD |
| High Cholesterol | Elevated levels of LDL cholesterol | Increases plaque formation |
| Hypertension | High blood pressure | Damages arterial walls |
| Diabetes Mellitus | Chronic hyperglycemia | Accelerates atherosclerosis |
| Smoking | Use of tobacco products | Damages endothelium, increases plaque instability |
Congenital anomalies of the LAD are rare but serious. These can include unusual origins, paths, or branching patterns. Some people might have a LAD that comes from the wrong place or gets compressed, which can be dangerous.
LAD pathologies can harm the heart’s function and rhythm. Stenosis or occlusion can cause ischemia or infarction. This can lead to heart failure or dangerous arrhythmias.
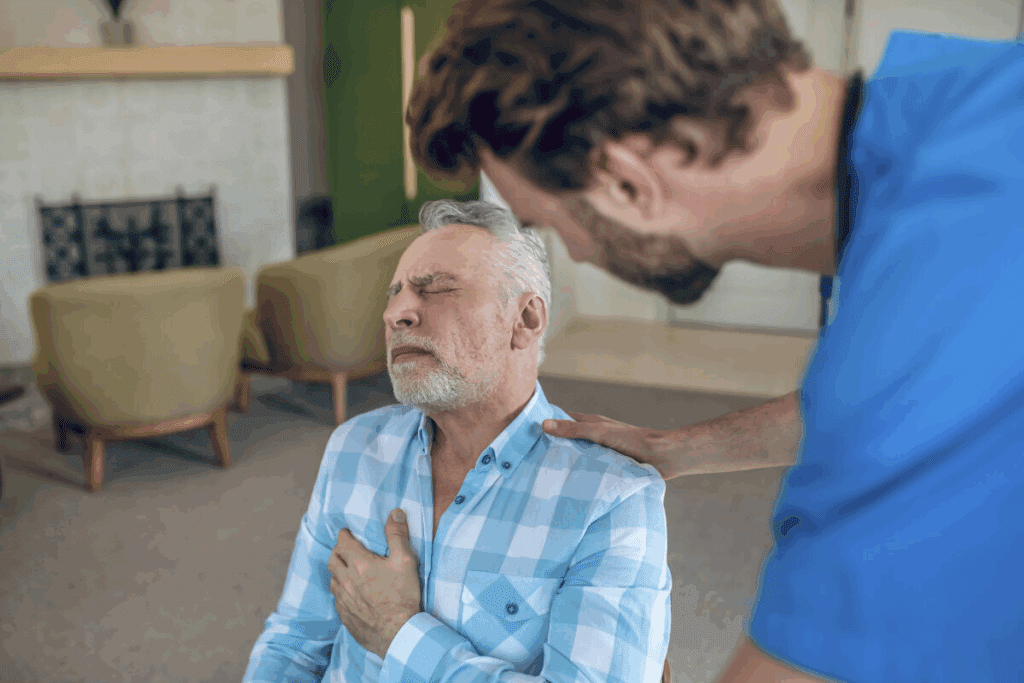
Clinical manifestations may include chest pain, shortness of breath, palpitations, or syncope. Quick diagnosis and treatment are vital to avoid lasting damage.
We must consider the clinical significance of LAD pathologies when evaluating patients with cardiovascular symptoms. Early detection and proper management can greatly improve outcomes.
Understanding LAD disease treatment is key. It includes medical therapy and revascularization. The right treatment depends on disease severity, patient health, and anatomy.
Medical management is often the first step. It aims to reduce symptoms and slow disease growth. It also manages risk factors.
“The goal of medical management is to stabilize the patient and improve quality of life,” as emphasized by cardiology guidelines. Adherence to prescribed medications and lifestyle changes is key for the best results.
Percutaneous coronary intervention (PCI) is a minimally invasive procedure. It’s used to open blocked coronary arteries. PCI is very effective for LAD disease, mainly when the disease is localized.
PCI involves:
Advances in stent technology, such as drug-eluting stents, have significantly improved PCI outcomes. But, the decision to use PCI must consider the complexity of the lesion and the patient’s condition.
Coronary artery bypass grafting (CABG) is a surgical procedure. It bypasses blocked sections of coronary arteries using grafts. CABG is often chosen for LAD disease when there’s significant disease or PCI is not suitable.
The benefits of CABG for LAD lesions include:
As noted by a leading cardiothoracic surgeon, “CABG remains a cornerstone in the management of complex LAD disease, providing durable revascularization.” The choice between CABG and PCI depends on a heart team’s assessment of the patient’s anatomy, comorbidities, and preferences.
New diagnostic tools are giving us a clearer picture of the LAD’s role in heart health. As medical technology improves, we’re learning more about the LAD’s importance in blood flow and heart function.
Recent years have brought big changes in imaging tech, changing cardiology a lot. Coronary computed tomography angiography (CCTA) and cardiac magnetic resonance imaging (MRI) give us detailed LAD images. This helps doctors make more accurate diagnoses.
These new tools are not just making diagnoses better. They also help doctors decide on the best treatments. For example, CCTA can spot blockages in the LAD. Cardiac MRI can see how much damage there is after a heart attack.
As we learn more about the LAD, treatments and prevention plans are getting better. We’re seeing new ways to target treatments and lower the risk of LAD blockages.
Personalized medicine is becoming key, with treatments made just for each person. Also, new percutaneous coronary intervention (PCI) and coronary artery bypass grafting (CABG) methods are on the horizon. They aim to improve results for those with LAD disease.
The LAD heart, or anterior interventricular artery, is key to heart health. It supplies blood to a big part of the heart muscle. This article has covered its anatomy, diseases, and treatments, showing its importance.
This artery feeds nearly half of the left ventricle, including the front wall and the wall between the ventricles. Blockages here can lead to heart attacks. Knowing about the LAD heart helps doctors care for patients better.
Understanding the LAD heart helps us improve patient care and lower heart risks. As we learn more about it, we can give better support to those with LAD-related diseases.
The LAD heart, or the anterior interventricular artery, is a key part of the left coronary artery. It supplies blood to the front of the left ventricle and the wall between the ventricles. This artery is essential for the heart’s function.
The anterior interventricular artery starts from the left coronary artery. It runs along the front wall of the heart and the wall between the ventricles. It supplies blood to these areas.
The “widow-maker” phenomenon is a blockage in the LAD artery’s starting part. This blockage is dangerous because it can severely damage the heart muscle. It can lead to serious heart problems or even death.
The LAD has branches like septal and diagonal branches. These branches help the heart’s electrical system and support the heart’s outer layer. They are vital for the heart’s function.
To see the LAD, doctors use coronary angiography, CT coronary angiography, and 3D reconstruction. These methods help diagnose LAD-related issues.
For LAD disease, treatments include managing the condition medically, using percutaneous coronary intervention, or coronary artery bypass grafting. The choice depends on the disease’s severity and location.
Risk factors for LAD occlusion include atherosclerosis, high blood pressure, high cholesterol, diabetes, and smoking. These factors can lead to LAD disease.
Knowing the LAD’s position and path is key for diagnosing and treating heart issues. It helps us understand its important role in heart function.
The LAD is also called the anterior interventricular artery, left anterior descending artery, or LAD artery. These names are used in medical practice.
New imaging technologies, like better CT coronary angiography, are improving LAD research and diagnostics. Future treatments and prevention methods, such as new drugs and techniques, are also being explored.
Government Health Resource. (2025). LAD Heart 7 Essential Facts About the Anterior.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!
WhatsApp us