Last Updated on November 26, 2025 by Bilal Hasdemir
Prostate cancer can affect many parts of a patient’s life, including causing pain in unexpected areas like the legs. Advanced prostate cancer can lead to leg pain and cramps, which can greatly reduce a patient’s quality of life. Could your leg cramps cancer symptoms be linked to your prostate? This powerful guide reveals the shocking connection you need to be aware of now.
We look into how prostate cancer can impact the legs, focusing on leg cramps and other related symptoms. It’s important for patients to understand these symptoms to get medical help on time and manage their condition well.
Prostate cancer’s effect on the legs is often seen in advanced stages. At this point, the cancer may have spread to other parts of the body, like the bones. This can cause pain and discomfort.
Key Takeaways
- Prostate cancer can cause leg pain and cramps, mostly in advanced stages.
- Understanding the symptoms is key for timely medical help.
- Leg pain from prostate cancer usually happens when the cancer spreads to the bones.
- Managing leg cramps and pain is vital for a good quality of life.
- Patients should get medical help if they have ongoing leg pain or cramps.
Understanding Prostate Cancer and Its Spread
To understand how prostate cancer affects leg health, we need to know about the disease and how it grows. Prostate cancer is a big health issue for millions of men around the world.
What is Prostate Cancer?
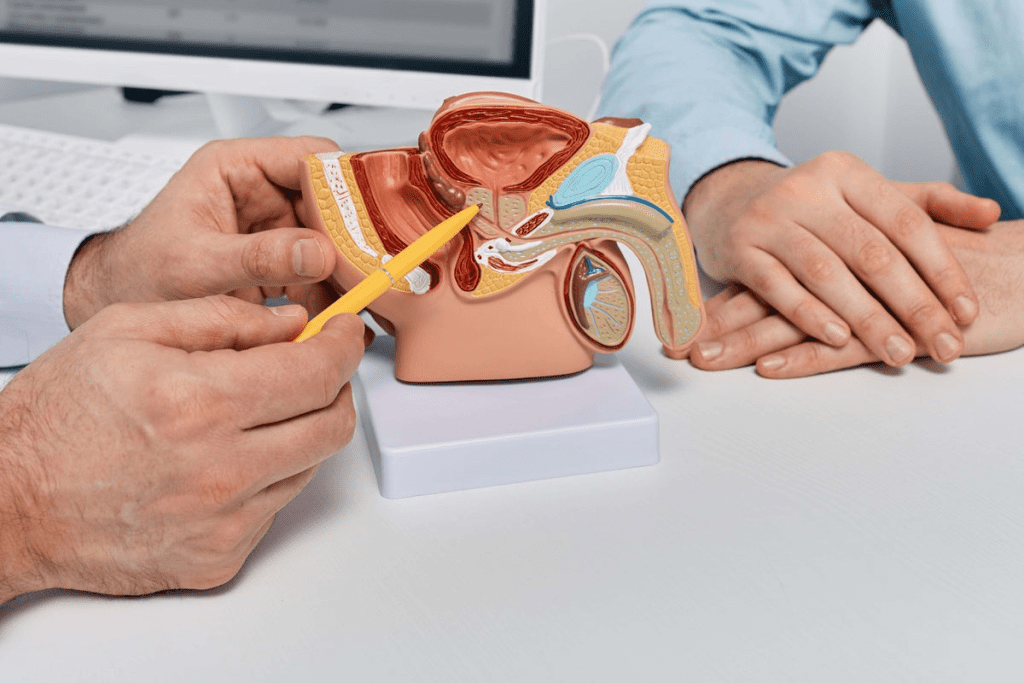
Prostate cancer starts in the prostate gland, a small gland below the bladder and in front of the rectum in men. The prostate gland is key to the male reproductive system, making fluids that help sperm. When cells in the prostate gland grow too much and don’t stop, cancer forms. It can spread to other parts of the body.
How Prostate Cancer Spreads Throughout the Body
Prostate cancer spreading, or metastasis, is a complex process. Cancer cells break off, enter the bloodstream or lymphatic system, and grow in other organs. Prostate cancer often goes to bones, like in the pelvis, spine, and ribs. This can cause pain and fractures.
Common Sites of Metastasis
Prostate cancer can spread to many organs, but bone metastasis is the biggest problem. The bones most often affected are in the:
- Pelvis
- Spine
- Ribs
- Femur (thigh bone)
Knowing where prostate cancer often spreads is key to spotting symptoms like leg pain.
Prostate cancer’s outcome depends on the tumor’s genetics and type. Advanced prostate cancer can cause a lot of pain, mainly when it reaches the bones. It’s important to manage prostate cancer pain well to improve patients’ lives.
The Connection Between Prostate Cancer and Leg Symptoms
Prostate cancer and leg symptoms are linked in complex ways. This cancer can cause leg pain directly or indirectly. It’s important for patients and doctors to understand this to spot symptoms early and treat them well.
Direct vs. Indirect Effects on Legs
Prostate cancer can hit the legs in different ways. Direct effects happen when cancer spreads to leg bones or tissues, causing pain. For example, bone metastases in advanced cancer can lead to leg pain.
Indirect effects might include nerve compression or other systemic issues leading to leg symptoms. For instance, cancer spreading to the spine can cause spinal cord compression. This can lead to leg pain, numbness, or weakness.
Prevalence of Leg Symptoms in Prostate Cancer Patients
Many prostate cancer patients, often those with advanced disease, experience leg symptoms. Studies show that a big number of patients with metastatic prostate cancer have bone pain, which can show up as leg pain. The frequency of these symptoms depends on the cancer’s stage and if there are bone metastases.
Early-stage prostate cancer usually doesn’t cause leg symptoms directly. But as the disease gets worse, the chance of leg pain or other symptoms increases. Knowing how common these symptoms are helps in giving the right care and support to patients.
Early vs. Late-Stage Manifestations
Leg symptoms can show up at any stage of prostate cancer, but more often in advanced stages. Early-stage prostate cancer might not cause leg symptoms directly. But as cancer progresses and might spread to bones, leg pain or discomfort can become more common.
In late-stage prostate cancer, leg symptoms can really impact mobility and quality of life. It’s key to manage these symptoms well to keep patients comfortable and functional. We’ll look at treatment options and management strategies next.
Bone Metastasis: How Prostate Cancer Affects the Skeletal System
Prostate cancer often spreads to the bones, worrying both patients and doctors. This happens in many cases of advanced prostate cancer. It causes problems that can really hurt a person’s quality of life.
Prostate Cancer’s Affinity for Bone Tissue
Prostate cancer likes to grow in the bones, often in the pelvis and spine. This is because cancer cells and bone tissue interact in a special way. The bone environment is perfect for cancer cells to thrive, creating bone metastases.
The bone metastasis process is complex. It starts with cancer cells breaking away from the main tumor. They then enter the blood and settle in the bones. There, they can mess with bone growth, causing damage.
Common Bone Metastasis Sites Affecting Legs
Bones like the pelvis, spine, and femur (thigh bone) are common targets for prostate cancer. These areas can cause pain, weakness, and trouble moving. For example, cancer in the femur can hurt a lot and raise the chance of breaking a bone. Spinal metastases can also harm the spinal cord, leading to neurological problems.
- Pelvis: Pain in the groin or hip area
- Spine: Back pain, neurological symptoms
- Femur: Thigh pain, risk of fractures
Mechanisms of Bone Pain in Metastatic Disease
Bone pain from prostate cancer metastasis comes from several sources. It can be caused by cancer cells directly attacking the bone, releasing chemicals that hurt, or by bone damage. Knowing how these happen helps doctors find better ways to manage pain.
Pain management for bone metastasis includes treatments like hormone therapy and chemotherapy. Local treatments like radiation and bisphosphonates are also used. These methods aim to shrink tumors, ease pain, and prevent more bone problems.
Leg Cramps Cancer Symptoms: What You Need to Know

Leg cramps are common, but they can be a sign of cancer. These cramps, or nocturnal cramps at night, can point to several health issues, including cancer.
Differentiating Between Normal Leg Cramps and Cancer-Related Cramps
Telling normal leg cramps from cancer-related ones is hard. Cancer-related cramps often last longer and hurt more. It’s important to know what your cramps are like.
- How often and how long the cramps last
- How bad the pain is
- If you feel weak or numb
Normal cramps usually come from dehydration, muscle strain, or not enough minerals. But, cancer cramps might also mean you’re losing weight, feeling very tired, or having bone pain.
When Leg Cramps May Signal Prostate Cancer
Prostate cancer can spread to bones, causing leg cramps. Leg cramps by themselves don’t mean you have prostate cancer. But, if you have cramps and other problems like trouble peeing or sex issues, you should see a doctor.
| Symptom | Possible Relation to Prostate Cancer |
| Leg Cramps | May occur in advanced stages due to bone metastasis |
| Urinary Symptoms | Common in prostate cancer, includes difficulty urinating |
| Sexual Dysfunction | Can be associated with prostate cancer, includes erectile dysfunction |
Other Cancers Associated with Leg Cramps
Other cancers can also cause leg cramps, mainly through bone spread or nerve pressure. These include:
- Breast cancer
- Lung cancer
- Multiple myeloma
Cancers that spread to bones can cause too much calcium, leading to muscle cramps and other symptoms.
Nocturnal Leg Cramps in Cancer Patients
Nocturnal leg cramps can really disrupt sleep for cancer patients. These cramps can make it hard to sleep well and affect your life quality. Managing these cramps means finding and treating the cause, which could be from cancer treatment or the cancer itself.
It’s key to understand why cancer patients get leg cramps. This helps in treating the cramps and improving their life.
Prostate Cancer and Hip Pain: A Common Connection
Prostate cancer can show up in many ways, including hip pain. This pain is a big deal and often surprises people. As prostate cancer grows, it can move to other parts of the body, like the bones. This can cause pain in the hips and other spots.
Why the Hip Joint is Frequently Affected
The hip joint is a favorite spot for prostate cancer to spread. This is because it has a lot of blood and special growth factors that draw cancer cells. When prostate cancer reaches the bones, it often picks areas with lots of bone activity, like the hip and pelvis.
This is because cancer cells like the bone environment. The hip, being a key joint that bears weight and has lots of bone activity, is a top spot for cancer to land.
Distinguishing Prostate Cancer Hip Pain from Other Causes
It can be hard to tell if hip pain is from prostate cancer or other issues like osteoarthritis or bursitis. But, there are clues that might point to prostate cancer.
- Pain that keeps getting worse or starts at night or with activity
- Pain that spreads to other places, like the groin or thigh
- Stiffness or trouble moving the hip joint
What Prostate Cancer Hip Pain Feels Like
Prostate cancer hip pain can feel different for everyone. Some might feel a dull ache, while others might get sharp pains. The pain can be steady or come and go, getting worse with movement or when you put weight on it.
If you have hip pain and have had prostate cancer, you should see your doctor. They can figure out why you’re in pain and help you get the right treatment.
Lymphatic Involvement: Swelling and Pain in the Legs
Prostate cancer can cause swelling and pain in the legs. This happens when the cancer reaches the lymph nodes. The lymphatic system is key to our immune response.
Impact on Lymph Nodes
Prostate cancer can spread to lymph nodes. This causes swelling and pain, often in the legs. Lymph nodes filter out harmful substances and fight infections.
When cancer cells invade these nodes, it disrupts their function. This leads to fluid buildup, causing swelling.
Lymphedema in Advanced Prostate Cancer
Lymphedema is a condition where fluid builds up in the body’s tissues. It usually affects an arm or leg. In prostate cancer, it happens when cancer blocks the lymphatic fluid flow.
This causes significant swelling in the legs. It makes movement uncomfortable and challenging for patients.
Swollen Groin Lymph Nodes in Male Patients
Male patients with prostate cancer often worry about swollen groin lymph nodes. These nodes can become enlarged when cancer spreads. Swelling can be painful and may come with redness or warmth.
It’s important for patients to tell their healthcare provider about these symptoms. This ensures proper evaluation.
Managing Cancer-Related Lymphedema
Managing lymphedema from prostate cancer requires a variety of treatments. These include:
- Compression garments to help reduce swelling
- Manual lymphatic drainage, a specialized massage technique
- Exercise programs tailored to the patient’s condition
- Education on proper skin care to prevent infections
| Treatment Option | Description | Benefits |
| Compression Garments | Specially designed to reduce swelling | Reduces discomfort, improves mobility |
| Manual Lymphatic Drainage | A gentle massage technique | Enhances lymphatic flow, reduces swelling |
| Exercise Programs | Tailored exercise regimens | Improves circulation, maintains flexibility |
Understanding how prostate cancer affects the lymphatic system is key. It helps manage symptoms like lymphedema and swollen lymph nodes. Patients and healthcare providers can work together to manage these conditions effectively.
Nerve Compression: When Prostate Cancer Affects the Nervous System
Prostate cancer can harm the nervous system, mainly through nerve compression. As it grows, it can press on nerves, causing symptoms. We’ll look at how prostate cancer impacts the nervous system, focusing on nerve compression and its effects.
Spinal Cord Compression and Leg Symptoms
Spinal cord compression is a serious issue with prostate cancer. It happens when cancer spreads to the spine and presses on the spinal cord. This can lead to leg pain, weakness, and numbness. In bad cases, it can cause paralysis and loss of bladder or bowel control.
The symptoms of spinal cord compression vary. They depend on where and how much the compression is. Common symptoms include:
- Leg pain or aching
- Weakness or numbness in the legs
- Difficulty walking or maintaining balance
- Loss of bladder or bowel control
Peripheral Nerve Involvement
Prostate cancer can also harm peripheral nerves. These are nerves outside the brain and spinal cord. Damage to these nerves can cause pain, numbness, and weakness in the affected areas. In some cases, it can lead to chronic pain and discomfort.
Radicular Pain Patterns in Prostate Cancer
Radicular pain happens when a nerve root is compressed or irritated. In prostate cancer patients, it can feel like shooting or stabbing pain. This pain goes from the lower back down to the legs and can be very severe.
Radicular pain patterns differ based on where the nerve root is compressed. Common patterns include:
- Pain radiating from the lower back to the buttocks and legs
- Numbness or tingling sensations in the legs
- Weakness in the muscles supplied by the affected nerve root
Neurological Emergencies Requiring Immediate Attention
Certain neurological symptoms need immediate medical help. These include sudden severe leg weakness, loss of bladder or bowel control, and severe pain that can’t be managed with medication. Quick treatment can help ease symptoms and prevent lasting damage.
If you or someone you know has these symptoms, seek medical help right away. Our healthcare team is committed to caring for prostate cancer patients. We help manage nerve compression and related symptoms.
Distinguishing Prostate Cancer Leg Pain from Other Conditions
It’s important to tell the difference between leg pain from prostate cancer and other causes. Leg pain can come from many things. Knowing what causes it helps in treating it right.
Common Non-Cancer Causes of Leg Pain
Many non-cancerous conditions can cause leg pain. Some common ones are:
- Musculoskeletal injuries
- Arthritis
- Peripheral artery disease
- Deep vein thrombosis
- Neurological disorders
These can often be treated without surgery. But, it’s key to check for prostate cancer, too, if you’ve had it before.
When to Suspect Cancer as the Underlying Cause
Leg pain is usually not from cancer. But, there are times when cancer might be the cause. Look out for these signs:
- Progressive pain that gets worse over time
- Pain that spreads to the legs or hips
- History of prostate cancer or known metastasis
- Unexplained weight loss or other systemic symptoms
If you see these signs, it’s important to get checked out.
Diagnostic Challenges in Identifying the Source
Finding the cause of leg pain in prostate cancer patients is hard. This is because prostate cancer can spread to many places. The challenges include:
| Diagnostic Challenge | Description |
| Multiple possible causes | Leg pain can come from many things, making it hard to find the cause. |
| Limited specificity of symptoms | Leg pain symptoms can be similar in different conditions, making it tough to diagnose. |
| Need for a complete evaluation | A detailed check-up, including scans and physical exams, is usually needed. |
Conditions That Mimic Prostate Cancer Leg Symptoms
Some conditions can seem like prostate cancer leg symptoms. These include:
- Osteoarthritis
- Spinal stenosis
- Peripheral neuropathy
- Musculoskeletal strain
Getting a correct diagnosis means looking at all the options carefully.
Diagnostic Approaches for Leg Symptoms in Prostate Cancer Patients
When prostate cancer patients have leg symptoms, finding the cause is key. Leg symptoms can come from bone metastasis, nerve compression, or other issues. Knowing the diagnostic tools helps patients and doctors find the cause and plan treatment.
Imaging Studies for Detecting Bone Metastasis
Imaging studies are important for finding bone metastasis in advanced prostate cancer. We use different imaging methods to spot bone metastasis, including:
- Bone Scintigraphy: This test is good at finding bone metastases all over the skeleton.
- Computed Tomography (CT) Scan: CT scans show detailed bone and tissue images, helping spot metastatic lesions.
- Magnetic Resonance Imaging (MRI): MRI is great for looking at the spine and finding spinal cord compression or other neurological problems.
- Positron Emission Tomography (PET) Scan: PET scans show areas of high metabolic activity, which means cancer spread.
| Imaging Modality | Sensitivity for Bone Metastasis | Clinical Utility |
| Bone Scintigraphy | High | Whole-body assessment |
| CT Scan | Moderate to High | Detailed bone and soft tissue imaging |
| MRI | High | Excellent for spinal and neurological evaluation |
| PET Scan | High | Assesses metabolic activity of metastases |
Blood Tests and Biomarkers
Blood tests and biomarkers are key in diagnosing and monitoring prostate cancer. These tests help us see how far the disease has spread and how well treatment is working.
- Prostate-Specific Antigen (PSA): High PSA levels can mean prostate cancer has come back or gotten worse.
- Alkaline Phosphatase: This enzyme is often high in patients with bone metastasis.
- Other Biomarkers: New biomarkers may give more info on disease outlook and treatment response.
Physical Examination Findings
A detailed physical exam is vital in diagnosing. We look for signs like:
- Leg Weakness or Paralysis: Shows neurological involvement.
- Swelling or Edema: May point to lymphedema or other circulatory problems.
- Pain on Palpation: Can mean bone metastasis or other muscle and bone issues.
By using imaging studies, blood tests, and physical exams, we can accurately find the cause of leg symptoms in prostate cancer patients. Then, we can create a treatment plan that fits each patient’s needs.
Treatment Options for Prostate Cancer-Related Leg Symptoms
Managing leg symptoms from prostate cancer needs a mix of treatments. As the cancer grows, it can cause bone problems and nerve issues. These lead to pain and discomfort in the legs.
Systemic Treatments Targeting the Cancer
Systemic treatments aim to fight cancer all over the body. For leg symptoms from prostate cancer, these treatments are key. They help reduce the tumor and ease symptoms.
- Hormone Therapy: This treatment lowers male hormones that help cancer grow.
- Chemotherapy: Drugs kill cancer cells and help manage advanced prostate cancer.
- Targeted Therapy: These drugs attack specific molecules that help cancer grow.
Local Treatments for Bone Metastases
Local treatments focus on bone metastases to ease pain and prevent more problems.
| Treatment | Description | Benefits |
| Radiation Therapy | High-energy rays target cancer cells in the bone | Pain relief, reduction in tumor size |
| Bone-Modifying Agents | Drugs that strengthen bones and reduce complications | Reduced risk of fractures, pain relief |
| Surgery | Operative procedures to stabilize or repair bone damage | Improved mobility, pain relief |
Interventional Procedures for Pain Relief
For those with severe leg pain, interventional procedures can help a lot.
- Nerve Blocks: Medication is injected around nerves to block pain signals.
- Spinal Cord Stimulation: A device is implanted to send electrical impulses to the spinal cord to reduce pain.
Emerging Therapies and Clinical Trials
New research is bringing new treatments for prostate cancer. These may help manage leg symptoms better.
Patients should talk to their doctors about clinical trials. This could lead to new treatment options.
Pain Management Strategies for Prostate Cancer Patients
Managing pain is key for prostate cancer patients to keep their quality of life good. As prostate cancer gets worse, pain can really affect patients. It impacts their physical health, emotions, and mind.
Pharmacological Approaches to Pain Control
Medicines are a big part of managing prostate cancer pain. We use many drugs, like NSAIDs, opioids, and other treatments, to help control pain. NSAIDs are good for mild to moderate pain. Opioids are for more severe pain that doesn’t get better with other treatments.
Choosing the right medicine depends on the pain’s severity, the patient’s health history, and possible side effects. We also think about using corticosteroids to lessen swelling and pain.
Non-Pharmacological Pain Management Techniques
There are also non-medical ways to manage pain. These include physical therapy, cognitive-behavioral therapy, and relaxation techniques like meditation. Physical therapy can make moving easier and reduce pain. Cognitive-behavioral therapy helps with the emotional side of pain.
Other non-medical methods are acupuncture, massage, and using heat or cold. These can help with pain when used with medicines.
Integrative Medicine Approaches
Integrative medicine mixes regular medical care with special therapies. For prostate cancer patients, this might include nutrition advice, mind-body therapies, and supplements. Nutritional counseling helps patients make food choices that can manage pain and improve health.
Mind-body therapies, like yoga and tai chi, can also help. They reduce stress and help relax, which can lessen pain.
Creating an Effective Pain Management Plan
Creating a good pain management plan needs teamwork. We work with patients, healthcare providers, and family to understand their pain and needs. A good plan considers the patient’s health, cancer stage, and past treatments.
It’s important to regularly check and update the plan as the patient’s situation changes. By using medicines, non-medical methods, and integrative approaches, we can help prostate cancer patients feel better and live better lives.
Physical Therapy and Exercise for Managing Leg Symptoms
Physical therapy and exercise can greatly help prostate cancer patients with leg symptoms. Symptoms like pain, weakness, or cramping can really affect a patient’s life. By adding physical therapy and exercise to their treatment, patients can see better mobility, strength, and function.
Benefits of Physical Therapy in Prostate Cancer
Physical therapy brings many benefits to prostate cancer patients with leg symptoms. It can lessen pain, improve movement, and boost muscle strength. A study in the Journal of Clinical Oncology found that physical therapy can greatly reduce leg symptoms in cancer patients.
Safe Exercise Recommendations
Prostate cancer patients with leg symptoms should do low-impact exercises. These exercises should help with flexibility and strength without making symptoms worse. Good exercises include:
- Gentle stretching to improve flexibility
- Resistance band exercises to build strength
- Short walks to maintain cardiovascular health
- Water-based exercises for low-impact mobility
It’s important for patients to talk to their healthcare provider or a physical therapist. They can create a personalized exercise plan that fits their needs and abilities.
Mobility Aids and Assistive Devices
Mobility aids and assistive devices are also key in managing leg symptoms. These can include:
- Canes or walkers to provide additional support
- Orthotics or shoe inserts to alleviate pain and improve mobility
- Braces to provide stability and support
Using these devices helps patients stay independent and do daily activities despite their leg symptoms.
Maintaining Function and Independence
The goal of physical therapy and exercise for prostate cancer patients is to keep them functioning and independent. By tackling leg symptoms early, patients can keep doing things they love and maintain a good quality of life.
By adding physical therapy, exercise, and mobility aids to their treatment, prostate cancer patients can manage leg symptoms well. This improves their overall well-being.
Does Prostate Cancer Affect Legs? Understanding Leg Cramps Cancer Symptoms
Prostate cancer can affect many parts of a patient’s life, including the legs. It can cause pain and cramps in the legs. This happens when cancer spreads or presses on nerves. We will look at how prostate cancer impacts the legs, including symptoms and ways to manage them.
It’s important for patients to know these symptoms to get medical help quickly. We will talk about how prostate cancer can lead to leg problems. We will also discuss ways to manage these symptoms, helping patients live better lives.
Key Takeaways
- Prostate cancer can cause leg pain and cramps, mostly in advanced stages.
- Understanding the symptoms is key for getting medical help on time.
- Managing leg symptoms can greatly improve a patient’s quality of life.
- Prostate cancer metastasis can cause discomfort in the legs.
- Nerve compression is another reason for leg pain in prostate cancer patients.
Understanding Prostate Cancer and Its Spread
Prostate cancer is a serious issue that needs to be understood. It involves the uncontrolled growth of abnormal cells in the prostate gland. This can lead to tumors, which might be benign or malignant.
The Nature of Prostate Cancer
Prostate cancer starts in the prostate gland and is a malignant tumor. The prognosis of prostate cancer is closely tied to the underlying genetics and histology of the tumor. Molecular characterization is key in determining the cancer’s aggressiveness and treatment options.
A leading oncologist noted, “The genetic makeup of prostate cancer cells can significantly influence the disease’s progression and response to treatment.”
“The future of prostate cancer treatment lies in understanding the molecular underpinnings of the disease,” said a renowned cancer researcher.
How Prostate Cancer Spreads Throughout the Body
Prostate cancer spreads through metastasis. Cancer cells break away, travel through the bloodstream or lymphatic system, and form new tumors. Common sites for prostate cancer metastasis include bones, lymph nodes, and less frequently, other organs like the lungs and liver.
| Site of Metastasis | Frequency | Symptoms |
| Bones | High | Pain, fractures |
| Lymph Nodes | Moderate | Swelling, pain |
| Lungs | Low | Cough, difficulty breathing |
| Liver | Low | Abdominal pain, jaundice |
Common Sites of Metastasis
The bones are a common site for prostate cancer metastasis, affecting hips, spine, and legs. This can cause pain, fractures, and mobility issues. Knowing these common sites helps in diagnosing and managing symptoms of advanced prostate cancer.
Understanding how prostate cancer spreads and affects the body helps patients and healthcare providers manage the disease. This improves quality of life.
The Connection Between Prostate Cancer and Leg Symptoms
It’s important to know how prostate cancer can affect the legs. This knowledge helps in giving better care. Prostate cancer can show up in many ways, including symptoms in the legs.
Direct vs. Indirect Effects on Legs
Prostate cancer can hit the legs in different ways. Direct effects happen when cancer spreads to leg bones or nearby tissues. This causes pain and discomfort.
Indirect effects come from nerve compression or other changes in the body due to cancer.
Direct effects often come from bone metastasis. This means cancer spreads to bones in the pelvis, femur, or other bones. It can cause pain, fractures, or other problems.
Prevalence of Leg Symptoms in Prostate Cancer Patients
Many prostate cancer patients, and those with advanced disease, experience leg symptoms. Research shows a big number of patients with metastatic prostate cancer have leg pain or other symptoms.
According to
“Prostate Cancer: Principles and Practice,” leg symptoms can occur in up to 30% of patients with advanced prostate cancer.
These symptoms can really affect a patient’s life. So, managing them well is key.
Early vs. Late-Stage Manifestations
Leg symptoms can show up at any stage of prostate cancer. They are more common in late stages but can also happen early.
Early symptoms might be from other conditions or indirect cancer effects. Late-stage symptoms are usually from metastasis or advanced disease.
It’s vital for patients and doctors to watch for leg symptoms in prostate cancer. Addressing them quickly helps keep quality of life high.
Bone Metastasis: How Prostate Cancer Affects the Skeletal System
It’s important to know how prostate cancer spreads to bones. This is key to managing the disease well. Prostate cancer often goes to the pelvis and spine, causing a lot of pain and problems.
Affinity for Bone Tissue
Prostate cancer has a special liking for bone tissue. This is why bone metastasis is common in advanced stages. The reasons behind this are complex, involving many molecular interactions.
The cancer cells from the prostate gland move to bones. There, they can damage or grow abnormally. This can cause prostate bone pain, a symptom many patients with bone metastasis face.
Common Sites of Bone Metastasis
Bone metastasis from prostate cancer often happens in the pelvis, spine, and ribs. These areas have a lot of bone marrow, which is perfect for cancer cells to grow.
| Site of Metastasis | Frequency | Common Symptoms |
| Pelvis | High | Hip pain, difficulty walking |
| Spine | High | Back pain, neurological symptoms |
| Ribs | Moderate | Chest pain, discomfort |
Mechanisms of Bone Pain
The reasons for prostate cancer and bone pain are complex. Bone metastasis can cause pain in several ways. This includes the release of chemicals that stimulate nerves, damage to bone tissue, and stretching of the periosteum.
It’s important to understand these mechanisms for effective pain management. Patients with hip pain prostate cancer need a treatment plan that tackles both the cancer and the pain.
Leg Cramps Cancer Symptoms: What You Need to Know
Exploring prostate cancer symptoms, we find leg cramps play a role. These sudden muscle contractions can be very uncomfortable. While often linked to common issues, they might also hint at serious health problems, like cancer.
Differentiating Between Normal Leg Cramps and Cancer-Related Cramps
Telling normal leg cramps from cancer-related ones is tricky. Yet, some signs might point to a more serious issue. For example:
- Frequency and Persistence: Cramps that keep coming back or don’t get better with usual treatments might need a closer look.
- Associated Symptoms: Other symptoms like leg pain, swelling, or weakness, or general symptoms like weight loss or tiredness, could mean something more serious.
- Timing: Cramps at night that mess with sleep or come with other nighttime symptoms are worth paying attention to.
When Leg Cramps May Signal Prostate Cancer
Leg cramps aren’t a direct sign of prostate cancer. But, if prostate cancer spreads to bones, it can cause pain and muscle spasms. The chance of leg cramps being linked to prostate cancer goes up if the cancer reaches the bones near nerves controlling the legs.
Other Cancers Associated with Leg Cramps
Other cancers can also cause leg cramps, either directly or through side effects. These include:
- Bone Cancer: Both primary and metastatic bone cancer can lead to pain and cramping in the affected limbs.
- Neurological Cancers: Tumors in the nervous system can mess with nerve function, causing muscle cramps and other symptoms.
Nocturnal Leg Cramps in Cancer Patients
Nocturnal leg cramps can be very upsetting as they disrupt sleep. In cancer patients, these cramps might be due to the cancer, its treatment, or other health issues. Treating these cramps often requires looking at the root cause and finding ways to ease symptoms.
Prostate Cancer and Hip Pain: A Common Connection
Prostate cancer can cause hip pain, affecting a patient’s life quality. The hip joint is a common site for cancer spread in prostate cancer patients. This leads to pain and discomfort, impacting mobility and well-being.
Frequency of Hip Joint Involvement
The hip joint is often affected in prostate cancer patients. This is because of its closeness to the prostate gland and the many blood vessels around it. Cancer cells from the prostate often spread to the bones, and the hip is a common place for this to happen.
Several factors make the hip joint more likely to be affected by prostate cancer metastasis:
- The hip joint bears weight, making it more prone to stress and cancer spread.
- The bone structure in the hip area is rich in cancellous bone, which is more vascular and susceptible to metastasis.
- The hip’s close proximity to the prostate gland makes it easier for cancer cells to spread through the bloodstream or lymphatic system.
Distinguishing Prostate Cancer Hip Pain
It can be hard to tell if hip pain is from prostate cancer or something else. But, some signs may point to cancer:
| Characteristic | Prostate Cancer Hip Pain | Other Causes of Hip Pain |
| Location | Typically deep-seated and radiates to the groin or thigh | Often localized to the hip joint or surrounding areas |
| Nature | Dull ache or sharp pain, often worse at night or with movement | Varies; can be sharp, dull, or aching |
| Duration | Progressive and persistent | Can be intermittent or constant |
Description of Prostate Cancer Hip Pain
Prostate cancer hip pain can feel different, but it’s often a deep ache that spreads to the groin or thigh. The pain might be sharp or dull and get worse with movement or at night. Patients may also feel stiff and have trouble moving the affected hip, affecting their daily life.
Understanding the link between prostate cancer and hip pain is key for diagnosis and treatment. Healthcare providers should think of prostate cancer as a possible cause of hip pain in male patients, even more so for those with a history of the disease.
Lymphatic Involvement: Swelling and Pain in the Legs
Prostate cancer can spread and affect the lymphatic system. This leads to leg swelling and discomfort. The lymphatic system is key for our immune response and fluid drainage. Knowing how prostate cancer impacts this system helps manage symptoms.
Impact on Lymph Nodes
Prostate cancer can spread to lymph nodes. These small, bean-shaped structures are part of our lymphatic system. When cancer cells invade, it can cause fluid buildup and swelling in the legs.
Swollen lymph nodes are a sign of advanced prostate cancer. The swelling happens because the lymph nodes are involved with cancer cells or reacting to cancer elsewhere in the body.
Lymphedema in Advanced Prostate Cancer
Lymphedema is a chronic condition causing swelling due to fluid buildup. It often results from surgery, radiation, or lymph node metastasis in prostate cancer.
Managing lymphedema is vital for quality of life. It involves physical therapy, compression garments, and sometimes manual lymphatic drainage.
Swollen Groin Lymph Nodes in Male Patients
Swollen groin lymph nodes are concerning for male patients with prostate cancer. These nodes are in the inguinal region and drain fluid from the legs. When prostate cancer spreads here, it can make them enlarge and become tender.
| Symptoms | Causes | Management |
| Swollen legs, pain, and discomfort | Prostate cancer metastasis to lymph nodes | Physical therapy, compression garments |
| Swollen groin lymph nodes | Cancer spread to inguinal lymph nodes | Monitoring, possible surgical intervention |
Managing Cancer-Related Lymphedema
Managing lymphedema needs a multi-faceted approach. This includes:
- Physical therapy to improve lymphatic flow
- Use of compression garments to reduce swelling
- Manual lymphatic drainage by trained therapists
- Patient education on self-management techniques
Working with healthcare professionals is key to developing a personalized plan. This helps patients control symptoms and improve their quality of life.
Nerve Compression: When Prostate Cancer Affects the Nervous System
Prostate cancer can harm the nervous system, leading to nerve compression. This happens when cancer spreads to nerves, causing pain and numbness. It also leads to other neurological symptoms.
Spinal Cord Compression and Leg Symptoms
Spinal cord compression is a serious issue with prostate cancer. It occurs when cancer spreads to the spine, pressing on the spinal cord. This can cause severe back pain, leg weakness, and even paralysis if not treated quickly.
Symptoms include trouble walking, numbness or tingling in the legs, and loss of bladder or bowel control. Early detection is key to prevent long-term damage. Seek medical help if symptoms get worse or don’t go away.
Peripheral Nerve Involvement
Prostate cancer can also affect peripheral nerves. These nerves are outside the brain and spinal cord. Symptoms include pain, weakness, and numbness in the areas served by the affected nerves.
For example, peripheral nerve involvement can cause radicular pain. This is pain that follows the nerve pathway.
Radicular Pain Patterns in Prostate Cancer
Radicular pain from prostate cancer varies based on the nerves affected. It can be sharp, shooting, or burning. It may also include muscle weakness or atrophy.
Understanding the pattern of radicular pain helps diagnose nerve involvement.
Neurological Emergencies Requiring Immediate Attention
Certain neurological issues from prostate cancer are emergencies. For example, severe spinal cord compression can cause cauda equina syndrome. This is marked by sudden severe pain, weakness, and loss of bladder and bowel control.
Prompt treatment, often surgery or radiation therapy, is vital to avoid permanent damage.
We stress the need to recognize these symptoms early. Seeking medical care quickly is essential for effective management.
Distinguishing Prostate Cancer Leg Pain from Other Conditions
It’s important to tell the difference between leg pain from prostate cancer and other causes. Leg pain can come from many things. Knowing the cause helps find the right treatment.
Common Non-Cancer Causes of Leg Pain
Many non-cancerous conditions can cause leg pain. For example, injuries, artery disease, and nerve problems. Osteoarthritis, tendinitis, and muscle strains are common. Restless leg syndrome and peripheral neuropathy also cause leg pain.
When checking leg pain in prostate cancer patients, think of these other causes. This helps avoid mistaking symptoms for cancer.
When to Suspect Cancer as the Underlying Cause
Some leg pain might be cancer, but not all. Look out for signs like pain that gets worse or spreads. Pain with weakness or numbness could mean cancer.
Prostate cancer patients should watch for new or getting worse leg pain. It might mean cancer has spread.
Diagnostic Challenges in Identifying the Source
Finding the cause of leg pain in prostate cancer patients is hard. It needs a detailed check-up, including scans and physical exams. This helps figure out where the pain comes from.
Doctors must look at the patient’s history, symptoms, and test results. This helps tell if the pain is from cancer or not.
Conditions That Mimic Prostate Cancer Leg Symptoms
Some conditions can look like prostate cancer leg symptoms. For example, degenerative disc disease, spinal stenosis, and osteoporotic fractures. They can cause similar pain.
Doctors need to know about these look-alikes. They must do a thorough check to find the real cause of leg pain in prostate cancer patients.
Diagnostic Approaches for Leg Symptoms in Prostate Cancer Patients
It’s important to find out why prostate cancer patients have leg symptoms. Doctors use many tools to figure out what’s causing these symptoms.
Imaging Studies for Detecting Bone Metastasis
Imaging studies are key in finding bone metastasis, a common reason for leg symptoms in prostate cancer patients. Common imaging modalities include:
- Computed Tomography (CT) scans
- Bone scans
- Magnetic Resonance Imaging (MRI)
- Positron Emission Tomography (PET) scans
These methods help see if there are bone metastases and how far they’ve spread. This helps doctors decide on treatment.
Blood Tests and Biomarkers
Blood tests and biomarkers are vital in checking prostate cancer activity and its effect on bones. Key markers include Prostate-Specific Antigen (PSA) levels and other signs of bone activity.
Physical Examination Findings
A detailed physical exam is key in checking leg symptoms. Doctors check muscle strength, reflexes, and any noticeable issues. They use this info, along with the patient’s history and symptoms, to make a diagnosis.
Doctors combine findings from imaging, blood tests, and physical exams to accurately diagnose leg symptoms in prostate cancer patients. This helps them create a treatment plan.
Treatment Options for Prostate Cancer-Related Leg Symptoms
Managing prostate cancer-related leg symptoms needs a full plan. This plan should tackle the cancer and its body effects. We’ll look at treatments like systemic and local options, pain relief methods, and new therapies and trials.
Systemic Treatments Targeting the Cancer
Systemic treatments aim to fight cancer all over the body. Hormone therapy is common, aiming to lower testosterone that helps cancer grow. Chemotherapy is used for advanced cases. Newer options like PARP inhibitors and immunotherapies are also being tested.
Local Treatments for Bone Metastases
Local treatments help those with bone metastases. Radiation therapy targets specific bone areas, easing pain and preventing fractures. Radiopharmaceuticals deliver radiation to bone metastases all over. Sometimes, surgical stabilization is needed to fix or prevent fractures.
Interventional Procedures for Pain Relief
Interventional procedures can help with severe pain. Nerve blocks and ablation techniques can manage pain well. Kyphoplasty or vertebroplasty can also stabilize vertebrae and lessen pain from fractures.
Emerging Therapies and Clinical Trials
The field of prostate cancer treatment is always changing. Emerging therapies and clinical trials bring new hope. These include new hormonal and targeted therapies, and immunotherapies. Joining clinical trials can give access to the latest treatments and help improve care.
Knowing all the treatment options helps patients and doctors create a detailed plan. This plan can effectively manage prostate cancer-related leg symptoms.
Pain Management Strategies for Prostate Cancer Patients
Managing pain is key for prostate cancer patients to keep their quality of life good. As the disease progresses, pain can become a big problem. It affects not just the body but also the mind and emotions.
Pharmacological Approaches to Pain Control
Medicine is often the first step in fighting prostate cancer pain. This includes:
- Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): Good for mild to moderate pain, NSAIDs cut down inflammation and ease pain.
- Opioids: For severe pain, opioids are used. They bind to opioid receptors in the brain and body, making pain less felt.
- Adjuvant Medications: Certain drugs, like anticonvulsants and antidepressants, help with specific pain types, like neuropathic pain.
A study in the Journal of Clinical Oncology shows the need for a personalized medicine plan. It found that plans made just for each patient can greatly improve pain management for prostate cancer patients
“Pain management in cancer patients requires a multifaceted approach, incorporating both pharmacological and non-pharmacological strategies to address the complex nature of cancer pain.”
Nadolski, et al., Journal of Clinical Oncology
Non-Pharmacological Pain Management Techniques
There are also non-medical ways to manage pain:
- Physical Therapy: Gentle exercises and physical therapy help keep muscles moving and pain down.
- Cognitive Behavioral Therapy (CBT): CBT helps patients deal with pain’s emotional side and find better ways to manage it.
- Relaxation Techniques: Activities like meditation, deep breathing, and progressive muscle relaxation can lower stress and pain.
| Technique | Description | Benefits |
| Physical Therapy | Gentle exercises to maintain mobility | Reduces pain, improves function |
| Cognitive Behavioral Therapy | Coping strategies for emotional aspects of pain | Enhances pain management, improves mental well-being |
| Relaxation Techniques | Meditation, deep breathing, progressive muscle relaxation | Reduces stress, alleviates pain |
Integrative Medicine Approaches
Integrative medicine mixes traditional treatments with complementary therapies. For prostate cancer patients, this can include:
- Acupuncture: This ancient Chinese method uses thin needles in specific body points to help heal and relieve pain.
- Massage Therapy: Massage can ease muscle tension, boost blood flow, and help relax.
- Yoga and Tai Chi: These practices mix physical movement with deep breathing and meditation to improve well-being and reduce pain.
Creating an Effective Pain Management Plan
Creating a good pain management plan needs teamwork between patients, doctors, and family. It’s important to:
- Assess Pain Regularly: Checking pain often helps adjust treatment plans as needed.
- Communicate Openly: Patients should talk freely about their pain and any worries with their healthcare team.
- Tailor the Plan: The plan should fit the patient’s needs, using a mix of medicines, non-medicines, and integrative methods as needed.
By taking a full and patient-focused approach to pain management, prostate cancer patients can live better lives and have better results.
Physical Therapy and Exercise for Managing Leg Symptoms
Managing leg symptoms from prostate cancer needs a mix of physical therapy and exercise. We know how important it is to tackle these symptoms. This helps improve life quality for those with prostate cancer.
Benefits of Physical Therapy in Prostate Cancer
Physical therapy is key for prostate cancer patients with leg symptoms. It helps with improved mobility and reduced pain. Physical therapists create exercise plans to help patients get stronger and more flexible. This makes everyday tasks easier.
- Enhanced muscle strength
- Improved flexibility and range of motion
- Better balance and coordination
- Reduced risk of falls
Safe Exercise Recommendations
Exercising with prostate cancer needs to be safe. Low-impact activities like walking, swimming, and cycling are good choices. Always talk to your doctor before starting any new exercise. This ensures it fits your health and needs.
Mobility Aids and Assistive Devices
Along with physical therapy and exercise, mobility aids help a lot. Items like canes, walkers, or orthotics offer support and stability. They improve life quality for those with leg symptoms from prostate cancer.
| Device | Purpose | Benefit |
| Canes | Provide additional support | Enhance balance |
| Walkers | Offer stability | Reduce fall risk |
| Orthotics | Support and align | Improve mobility |
Maintaining Function and Independence
Keeping function and independence is key in prostate cancer rehab. Physical therapy, exercise, and mobility aids help. This way, patients can do daily tasks with little help. We focus on a plan that fits each patient’s needs.
Adding physical therapy and exercise to treatment plans helps prostate cancer patients. They can manage leg symptoms and stay independent. We’re here to support them every step of the way.
End-Stage Prostate Cancer Symptoms Affecting the Legs
Prostate cancer in its final stages can cause many symptoms. These symptoms can really affect a person’s quality of life, mainly their legs. It’s hard for both patients and caregivers to deal with these symptoms, so they need good management plans.
Progressive Symptoms in Advanced Disease
In the last stages of prostate cancer, symptoms get worse and harder to handle. Leg pain, weakness, and swelling are common. It’s important to understand these symptoms to manage them well.
A study in the Journal of Clinical Oncology found that bone metastasis causes a lot of pain and trouble for advanced prostate cancer patients.
Managing Severe Leg Symptoms in Palliative Care
Palliative care is key in dealing with severe leg symptoms from end-stage prostate cancer. It aims to ease symptoms, pain, and stress from serious illnesses. Palliative care teams work with patients and families to create care plans that fit their needs.
| Palliative Care Approach | Description |
| Pain Management | Using medicines and other methods to control pain well. |
| Symptom Control | Handling symptoms like swelling, weakness, and numbness in the legs. |
| Emotional Support | Offering psychological support to patients and their families. |
Quality of Life Considerations
Keeping quality of life high is a main goal for patients with end-stage prostate cancer. It’s not just about physical symptoms but also emotional and social needs. Care plans are made to help patients stay independent and keep their dignity.
“The goal of palliative care is to improve the quality of life for both the patient and the family.”
NATIONAL INSTITUTE ON AGING
Supporting Caregivers of Patients with Mobility Limitations
Caregivers are very important for patients with end-stage prostate cancer, and those with mobility issues. It’s key to give caregivers the right resources, education, and emotional support. Support groups and respite care are very helpful for caregivers.
When to Seek Medical Attention for Leg Symptoms
Leg symptoms can worry prostate cancer patients. It’s important to know when to get help. Prostate cancer can cause leg symptoms from mild to severe.
Red Flag Symptoms Requiring Immediate Care
Certain leg symptoms need quick medical attention. These red flag symptoms include:
- Severe, sudden-onset pain
- Swelling or redness in the leg
- Weakness or numbness in the legs
- Difficulty walking or maintaining balance
- Loss of bladder or bowel control
Discussing Leg Symptoms with Your Healthcare Provider
Talking openly with your healthcare provider is key when you have leg symptoms. Keep a symptom journal. This helps your healthcare provider understand and manage your symptoms better.
When talking about your leg symptoms, share:
- The location and nature of the pain or discomfort
- Any factors that relieve or worsen the symptoms
- Any recent changes in your symptoms
Follow-up Monitoring of Leg Symptoms
Regular check-ups with your healthcare provider are important. They can check your symptoms, review your journal, and order tests. This helps track your condition.
Report any changes in your leg symptoms. This info helps in making treatment decisions.
Advocating for Proper Symptom Management
You are a key part of your care. If leg symptoms affect your life, talk to your healthcare provider. Ask questions like:
- What are the possible causes of my leg symptoms?
- What treatment options are available to manage my symptoms?
- Are there any lifestyle changes I can make to alleviate my symptoms?
Working with your healthcare provider helps manage your symptoms well.
Psychological Impact of Dealing with Prostate Cancer Leg Symptoms
Living with prostate cancer leg symptoms can be tough emotionally. People may feel anxious, depressed, isolated, and frustrated.
Emotional Challenges of Mobility Limitations
Mobility issues from prostate cancer can really affect a person’s life. Losing independence and needing help with daily tasks can make one feel sad and hopeless.
As one patient noted,
“It’s hard to accept that I can no longer do things on my own. It feels like I’ve lost a part of myself.”
This emotional battle is common for those facing mobility problems due to prostate cancer.
Coping Strategies for Patients and Families
Finding ways to cope is key for patients and their families. This can include getting support from loved ones, joining groups, and seeking therapy.
- Practicing mindfulness and relaxation techniques
- Staying connected with friends and family
- Engaging in activities that bring joy and fulfillment
These strategies can help lessen the emotional toll of prostate cancer leg symptoms.
Support Resources and Groups
Support groups and resources are vital for coping with prostate cancer’s emotional impact. They offer a sense of community and understanding.
| Resource | Description |
| Support Groups | Face-to-face or online groups where patients can share their experiences |
| Counseling Services | Professional therapy to address emotional and psychological needs |
| Online Forums | Platforms for patients to connect and share information |
Maintaining Mental Well-being During Treatment
It’s important to keep mental health in check during prostate cancer treatment. Patients should seek support, practice self-care, and enjoy activities they love.
By recognizing the emotional effects of prostate cancer leg symptoms and using available support, patients can manage their treatment better.
Conclusion: Living Well Despite Prostate Cancer Leg Symptoms
Understanding the link between prostate cancer and leg symptoms is key. This knowledge helps manage the disease better and improves life quality. We’ve looked at how prostate cancer can cause leg cramps, pain, and swelling.
Managing prostate cancer symptoms requires a full approach. Patients can work with their healthcare team to tackle symptoms. This way, they can keep their overall health in check.
We urge patients to watch for any unusual or ongoing leg symptoms. If they notice anything odd, they should see a doctor. With proper care, it’s possible to live well even with prostate cancer.
FAQ
Does prostate cancer cause leg pain?
Yes, prostate cancer can cause leg pain. This is more common in advanced stages when it spreads to bones or affects nerves.
What are the common symptoms of prostate cancer affecting the legs?
Symptoms include leg pain, hip pain, and leg cramps. Swelling and numbness or tingling sensations can also occur due to nerve compression.
How does prostate cancer metastasize to the bones?
Prostate cancer cells spread to bones through the bloodstream or lymphatic system. They often target the spine, pelvis, and femur.
Can leg cramps be a symptom of prostate cancer?
Leg cramps can have many causes. But, in some cases, they might be linked to prostate cancer, if they’re persistent or severe.
How can I differentiate between normal leg cramps and those related to prostate cancer?
Cancer-related cramps are often more severe and persistent. They might also be accompanied by pain or numbness. Always consult a healthcare provider for evaluation.
What is the connection between prostate cancer and hip pain?
Prostate cancer can spread to the hip bones or affect surrounding tissues. This causes hip pain. The hip’s rich blood supply makes it a common site for metastasis.
How does prostate cancer affect the lymphatic system?
Prostate cancer can spread to lymph nodes. This causes swelling and pain in areas like the groin and legs.
What is lymphedema in the context of prostate cancer?
Lymphedema is swelling in the legs or other areas due to impaired lymphatic drainage. It often occurs in advanced prostate cancer.
Can prostate cancer cause nerve compression?
Yes, prostate cancer can compress nerves. This happens when it metastasizes to the spine or pelvis. It leads to symptoms like pain, numbness, or weakness in the legs.
How is leg pain diagnosed in prostate cancer patients?
Diagnosis involves imaging studies (like bone scans or MRI), blood tests, and physical examinations. These help determine the cause of leg pain.
What are the treatment options for managing prostate cancer-related leg symptoms?
Treatments include systemic therapies targeting the cancer and local treatments for bone metastases. Pain management strategies and physical therapy also help maintain mobility and function.
How can patients manage pain associated with prostate cancer?
Pain management includes pharmacological approaches and non-pharmacological techniques like physical therapy. Integrative medicine approaches are also beneficial.
What role does physical therapy play in managing leg symptoms?
Physical therapy helps maintain mobility, strength, and function. It reduces the risk of complications and improves quality of life for prostate cancer patients.
When should I seek medical attention for leg symptoms?
Seek medical attention for persistent or severe leg pain, swelling, numbness, or other concerning symptoms. This is important, even more so if you have a history of prostate cancer.
How can I cope with the emotional challenges of prostate cancer leg symptoms?
Coping strategies include seeking support from healthcare providers, support groups, and loved ones. Prioritizing mental well-being through stress management techniques is also key.
Reference
- Kratzer, T. B., et al. (2025). Prostate cancer statistics: Trends and future directions. CA: A Cancer Journal for Clinicians. https://pubmed.ncbi.nlm.nih.gov/35454378/





