Last Updated on November 13, 2025 by
Managing a child with sickle cell disease (SCD) needs a detailed plan. SCD changes the shape of red blood cells, causing problems with blood flow, pain, and health issues. Along with medical care, lifestyle changes with sickle cell play an important role in reducing complications and improving daily life.
Symptoms of SCD can start as early as 5 months old. Parents are key in managing their child’s care. They make important decisions for their child’s health.
Managing SCD well requires a team effort. This includes medical care, lifestyle changes, and emotional support. Knowing about SCD’s genetics and symptoms helps parents face the challenges of caring for a child with this condition.
Key Takeaways
- Early diagnosis and intervention are key in managing SCD.
- A detailed care plan is needed for a child with SCD.
- Parents are vital in managing their child’s SCD through informed decisions.
- Lifestyle changes are important in managing SCD symptoms.
- Emotional support is critical for children with SCD and their families.
Understanding Sickle Cell SS Disease in Children
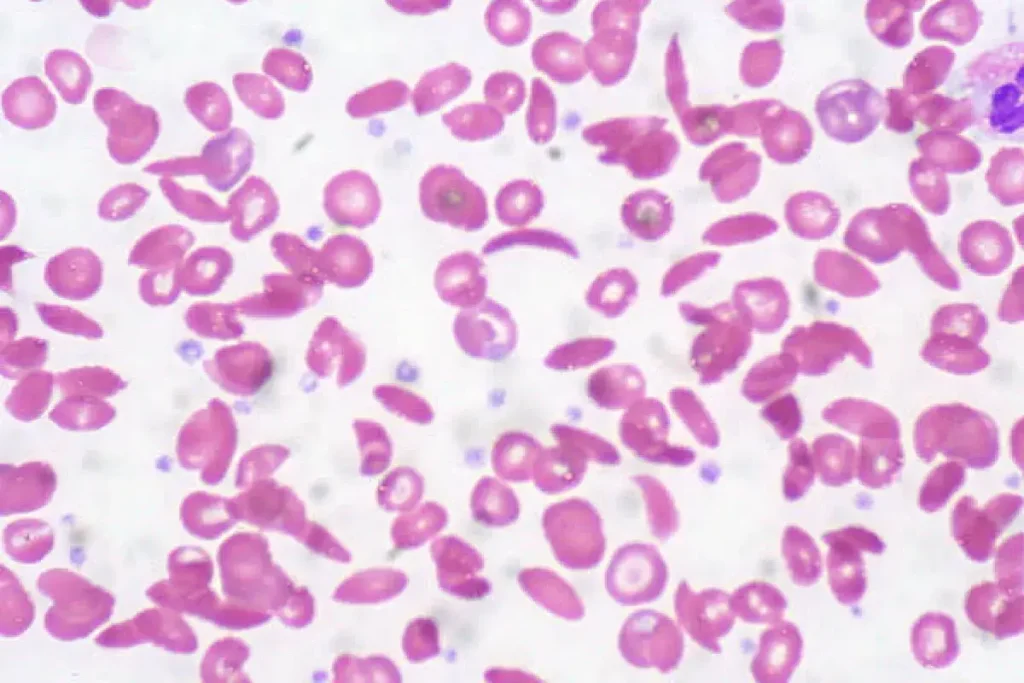
Sickle Cell SS disease, also known as Sickle Cell Anemia, is a severe form of Sickle Cell Disease. It affects children’s health deeply. This genetic disorder changes the hemoglobin in red blood cells, making them sickle-shaped.
This shape makes it hard for the cells to move through small blood vessels. This can lead to many health problems.
What is Sickle Cell Anemia SS Genotype
Sickle Cell Anemia SS genotype happens when a child gets two sickle cell genes, one from each parent. This is the most severe form of Sickle Cell Disease. Knowing the genetic makeup is key to managing the condition well.
Children with this genotype often face more severe symptoms than others. Early detection through newborn screenings is vital for better outcomes.
Recognizing Sickle Cell Disease Symptoms in Infants
It’s important to spot Sickle Cell Disease symptoms in infants early. Common signs include anemia, jaundice, and swelling in the hands and feet. They might also have pain crises, which can be hard to spot because they can’t tell us how they feel.
Parents should watch for signs of infections, as these children are more at risk. Quick medical help is needed if they show fever, lethargy, or trouble breathing.
How Sickle Cell Disease Affects Daily Life
Sickle Cell Disease greatly affects the daily lives of children and their families. It can cause pain crises, anemia, and delayed growth, among other issues. A good care plan is needed, including medical treatment, lifestyle changes, and emotional support.
Managing the disease means regular doctor visits, taking medicine, and watching for complications. Families must work with healthcare providers to create a care plan that fits their child’s needs.
Early action and support can help children with Sickle Cell Disease do well in school and socially. By understanding the disease, families can help their child have a happy and fulfilling life.
Essential Lifestyle Changes with Sickle Cell
Children with sickle cell disease can greatly improve their lives by making some lifestyle changes. These changes include staying hydrated, eating right, being active, and managing their environment.
Maintaining Optimal Hydration Levels
It’s very important for kids with sickle cell to drink lots of water. Hydration helps prevent sickle cell crises by keeping blood vessels flexible. They should drink at least 8-10 glasses of water a day. Avoid drinks with caffeine and sugar, as they can make dehydration worse.
Here are some tips for staying hydrated:
- Encourage your child to drink water often, more so after they’ve been active.
- Check if their urine is pale yellow or clear. If it is, they’re drinking enough water.
- Stay away from very hot or cold temperatures to prevent dehydration.
Developing a Balanced Nutrition Plan
A balanced diet is key to managing sickle cell disease. Foods rich in nutrients can help keep your child healthy and reduce crisis frequency. Focus on fruits, veggies, whole grains, and lean proteins. Avoid foods that can make symptoms worse.
Here’s what a balanced diet should include:
- More folate from leafy greens and fortified cereals.
- A variety of colorful fruits and veggies.
- Lean proteins like poultry, fish, and legumes.
Safe Physical Activity Guidelines
Doing the right kind of physical activities can boost health and happiness for kids with sickle cell. But it’s important to balance activity with rest to avoid a crisis. Swimming, cycling, and yoga are good choices because they’re low-impact.
Here are some guidelines for safe physical activity:
- Talk to your child’s doctor to create a personalized exercise plan.
- Make sure your child drinks water before, during, and after exercising.
- Watch for signs of getting too tired or overheating.
Managing Environmental Factors
Managing environmental factors is also key to preventing sickle cell crises. Extreme temperatures, high altitudes, and other stressors can trigger crises. Parents should be careful and take steps to protect their children.
How to Prevent Sickle Cell Crises
To prevent sickle cell crises, we need to make lifestyle changes and follow medical advice. Knowing what causes these crises helps us find ways to avoid them.
Identifying and Avoiding Common Triggers
First, we must find and stay away from common triggers. These include very hot or cold temperatures, not drinking enough water, and getting sick. Staying hydrated is key, so drink lots of water, more so in hot weather or when you’re active.
It’s also important to avoid extreme temperatures. Stay inside when it’s very hot or cold. Wear layers to keep your body temperature steady.
Creating Daily Preventive Routines
Having daily routines can help a lot. Eat well, exercise gently, and get enough sleep. These habits help keep crises away.
- Eat a diet full of fruits, veggies, and whole grains.
- Do gentle exercises like walking or swimming.
- Make sure to sleep well each night.
Medication Management Strategies
Managing your medicines is key to avoiding crises. Stick to your doctor’s plan, including vaccines and antibiotics. Watch out for any side effects.
Working closely with your doctor is vital. This means regular check-ups and changing your meds if needed.
Stress Reduction Techniques
Stress can lead to crises, so finding ways to relax is important. Try meditation, deep breathing, and yoga to lower stress.
Adding these to your daily life can help manage stress. This reduces the chance of having a crisis.
Recognizing and Managing Pain Crises in Sickle Cell
It’s key to know how to handle pain crises in Sickle Cell Disease (SCD) to make life better for kids. Pain crises happen when sickled red blood cells block blood flow. This causes pain and tissue damage.
What Does Sickle Cell Pain Feel Like
Pain from Sickle Cell can be very different for each child. It’s often very intense and can stop them from moving. The pain usually hits the bones, joints, and belly.
- Characteristics of Sickle Cell Pain: Sharp, throbbing, or stabbing
- Common Locations: Back, arms, legs, and abdomen
- Triggers: Cold weather, dehydration, stress, and infections
Home-Based Pain Management Approaches
At home, managing pain crises needs both medicine and other methods. It’s important to work with your doctor to make a plan that fits your child.
- Hydration: Make sure your child drinks lots of water to avoid dehydration.
- Medication: Use pain medicines as your doctor says.
- Comfort Measures: Use warm compresses or warm baths to ease pain.
When to Contact Your Doctor vs. Emergency Room
Knowing when to get help is important. Call your doctor if home treatments don’t work or if you see signs of infection. Go to the emergency room for severe pain, trouble breathing, or any neurological issues.
“Prompt recognition and treatment of pain crises can significantly improve the quality of life for children with Sickle Cell Disease.”
Creating an Effective Pain Management Plan
Creating a good pain plan needs teamwork with your healthcare team. You need to know your child’s pain patterns and what works best. This plan should be checked and updated often to keep it working well.
- Keep a Pain Diary: Record pain details like when, how bad, and what causes it.
- Medication Adherence: Make sure your child takes their medicine as told.
- Regular Follow-Ups: See your healthcare provider often to update the pain plan.
By understanding and managing pain crises well, we can greatly improve life for kids with Sickle Cell Disease.
Addressing Fever and Infections in Sickle Cell Disease
Managing fever and infections is key for kids with Sickle Cell Disease (SCD). Fever can mean an infection, and kids with SCD are more at risk. We’ll look at why quick medical help is needed, how to prevent infections, and the role of vaccines and meds in SCD care.
Why Fever in Sickle Cell Disease Requires Immediate Attention
Fever in SCD kids can mean a serious infection. This needs quick medical help. Infections can cause sickle cell crises, leading to serious problems. We stress the importance of acting fast when a child with SCD gets a fever.
Immediate actions to take when a child with SCD develops a fever include:
- Contacting the child’s healthcare provider immediately
- Monitoring the child’s temperature closely
- Ensuring the child stays hydrated
Implementing Infection Prevention Measures
Stopping infections is key in SCD care. We suggest several steps to lower infection risk. These include good hygiene, avoiding sick people, and keeping up with vaccines.
Good hygiene practices include:
- Frequent handwashing
- Avoiding close contact with anyone who is sick
- Keeping the child’s environment clean
Essential Vaccinations and Preventive Medications
Vaccines and meds are vital for SCD kids. We talk about sticking to the vaccine schedule and using antibiotics to prevent infections like pneumococcal disease.
Key vaccinations and medications for children with SCD include:
- Pneumococcal conjugate vaccine (PCV)
- Pneumococcal polysaccharide vaccine (PPV)
- Meningococcal vaccine
- Penicillin prophylaxis
Developing an Emergency Fever Protocol
Having a fever emergency plan is vital for SCD families. This plan should cover when to get medical help, how to handle a fever at home, and emergency plans.
Components of an emergency fever protocol include:
- Knowing the threshold for seeking immediate medical attention
- Having a list of emergency contact numbers
- Understanding how to administer fever-reducing medications
Building a Comprehensive Medical Support Team
Creating a strong medical support team is key to managing Sickle Cell Disease in kids. A team of different healthcare experts is needed to meet the complex needs of children with SCD.
Essential Healthcare Specialists for SS Children
Children with Sickle Cell SS Disease need care from many specialists. This includes hematologists, pediatricians, and sometimes mental health professionals. Integrated mental health services are very important for addressing their emotional and behavioral needs.
- Hematologists: They specialize in blood disorders and help manage SCD.
- Pediatricians: They provide primary care and watch over the child’s overall health.
- Mental Health Professionals: They support the child’s emotional and psychological well-being.
Coordinating Care Between Providers
It’s important for healthcare providers to work well together for seamless care. We suggest having a shared care plan that all providers can access.
- Choose a primary contact to coordinate care.
- Use a shared electronic health record system.
- Hold regular team meetings to discuss the child’s care plan.
Preparing for Hospital Visits and Admissions
Hospital visits and admissions can be tough for kids with SCD. Preparing them ahead of time and having a plan can help reduce stress and anxiety.
- Bring a copy of the child’s medical history and current medications.
- Have a bag ready with essentials like favorite toys or comfort items.
- Talk to the child about the hospital visit beforehand to ease their fears.
Medication Management and Adherence
Managing medications is a big part of SCD care. Making sure the child takes their medications as prescribed can prevent problems and reduce crisis frequency.
Medication adherence strategies include:
- Using pill boxes or reminders on smartphones.
- Creating a routine for taking medications at the same time every day.
- Watching for side effects and adjusting medications as needed.
Supporting Educational and Social Development
Helping kids with Sickle Cell Disease (SCD) grow is key to their happiness. They might need special help at school. This is important for their future.
Working with Schools on Accommodation Plans
Kids with SCD might need special help at school. Working with schools to make a plan is very important. This plan helps them manage their health during school.
Key components of an accommodation plan:
- Identifying triggers and developing strategies to avoid them
- Creating a protocol for managing pain crises and other emergencies
- Providing access to necessary medications and treatments
- Ensuring the child has regular breaks and stays hydrated
Helping Your Child Explain Their Condition to Others
Kids with SCD need to talk about their condition. This helps others understand and reduces stigma. Help them find a simple way to explain it.
Tips for helping your child explain their condition:
- Use age-appropriate language to explain SCD
- Role-play different scenarios to build confidence
- Encourage your child to ask questions and seek support when needed
Building Resilience and Independence
Teaching kids with SCD to be strong and independent is very important. This means teaching them to handle their condition and make good choices.
Strategies for building resilience:
- Encouraging self-advocacy and self-care
- Promoting positive relationships with family and friends
- Developing problem-solving skills and coping mechanisms
Connecting with Support Groups and Resources
Connecting with others who understand SCD is very helpful. Look for local and online groups, as well as educational resources.
Benefits of support groups:
- Sharing experiences and advice with others who understand SCD
- Accessing educational materials and resources
- Building a network of supportive peers and families
Conclusion: Empowering Your Child for a Healthy Future with Sickle Cell SS
Helping children with SCD is key to their well-being and future. Knowing about the condition and making lifestyle changes are important. A strong support system also helps them live fulfilling lives.
Early diagnosis and the use of technology can greatly help children with SCD. With the right care and support, they can achieve their goals. We need to keep teaching them how to manage their condition well.
Working together with healthcare, schools, and support groups is vital. We can create a supportive environment for children with SCD. This effort needs dedication, compassion, and a focus on top-notch care.
FAQ
What is Sickle Cell Anemia SS Genotype?
Sickle Cell Anemia SS genotype, also known as Sickle Cell Disease (SCD), is a genetic disorder. It affects how red blood cells make hemoglobin. This happens when a person gets two bad hemoglobin genes, one from each parent.
These genes make sickle hemoglobin or hemoglobin S. This is an abnormal form of hemoglobin.
How does Sickle Cell Disease affect daily life?
Sickle Cell Disease can really change daily life. It causes pain episodes, a higher risk of infections, and other problems. Kids with SCD might need to stay hydrated and avoid extremetemperaturesh They also need to manage stress to prevent crises.
What are the symptoms of Sickle Cell Disease in infants?
Infants with Sickle Cell Disease might have fever, fussiness, and swelling in the hands and feet. They might also have pale skin. Early treatment is key to managing the disease and avoiding complications.
How can I prevent Sickle Cell crises?
To prevent Sickle Cell crises, stay hydrated and avoid extreme temperatures. Manage stress and follow your medication plan. Knowing and avoiding common triggers can also help.
What does Sickle Cell pain feel like?
Sickle Cell pain can feel sharp, stabbing, or throbbing. It can be intense or ongoing. It might also come with fever, swelling, or shortness of breath.
How can I manage pain crises at home?
To manage pain crises at home, use medication, stay hydrated, and rest. Having a pain management plan is important. This might include over-the-counter pain relievers, prescription meds, and alternative therapies like heat or cold.
Why is fever a concern in Sickle Cell Disease?
Fever is a big worry in Sickle Cell Disease. It can mean an infection is present, which is dangerous if not treated quickly. Kids with SCD are more likely to get infections because their immune system is weak.
How can I support my child’s educational and social development with Sickle Cell?
To support your child’s education and social life, work with their school to make a plan. Help them explain their condition to others. Encourage them to be independent and resilient.Also, connect them with support groups and resources.
What are the essential lifestyle changes for managing Sickle Cell Disease?
Key lifestyle changes include staying hydrated and eating well. Engage in safe physical activities and manage your environment to prevent crises.
How can I build a compassionate medical support team for my child?
To build a supportive medical team, gather specialists like hematologists and pediatricians. Coordinate care and prepare for hospital visits. Managing medications is also important.
References
- Whittington Health NHS Trust. (2023). Sickle Cell Disease (SCD) in childhood – Management. https://www.whittington.nhs.uk/document.ashx?id=6257
- McGann, P. T., & Ware, R. E. (2013). Current management of sickle cell anemia. Hematology/Oncology Clinics of North America, 27(2), 173“189. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3721270/
- West London Haemoglobinopathy Coordinating Centre. (2023). Guidelines for the management of sickle cell disorders in children. https://www.imperial.nhs.uk/-/media/hcc/documents/hcc-draft-paediatric-sickle-cell-guideline-version-10-september-2023.pdf?rev=11f205efce134b62a4550d0158d0ae26