Managing a liver stent is key for those with bile duct blockages. A bile duct stent is a small tube that helps clear blockages in the bile ducts. These blockages can be due to tumors, stones, or strictures.
At Liv Hospital, we focus on advanced patient care. We ensure everyone gets expert and caring treatment. Biliary stenting uses plastic or metal stents to clear obstructions or fix biliary leaks. Knowing about the procedure, its benefits, risks, and aftercare is important for good management.
Key Takeaways
- Understanding the purpose and function of a liver stent is key for effective management.
- The procedure for placing a bile duct stent involves relieving obstructions or treating biliary leaks.
- Managing a liver stent includes knowing its benefits and risks.
- Proper aftercare is essential for the successful management of a liver stent.
- Liv Hospital provides complete care and guidance for those with liver stents.
Understanding Liver Stents and Their Function
Liver stents are tiny, hollow tubes put into the bile duct to clear blockages. They help bile flow into the intestine, which is key for digestion and liver health.
What Is a Bile Duct Stent?
A bile duct stent keeps the bile duct open, letting bile flow into the intestine. Stents can be plastic or metal, depending on the patient’s needs and how long they’ll be in place.
Biliary stenting is a way to fix obstructions or leaks in the biliary tree. The stents are made to fit well with the body and handle the bile flow and pressure.
How Stents Work in the Biliary System
The biliary system makes, stores, and moves bile, a key digestive fluid. A blockage in the bile duct can cause serious problems like jaundice, infection, and liver damage.
Stents keep the bile duct open, allowing bile to flow normally. This helps symptoms go away and prevents more problems. Doctors use endoscopic methods, like ERCP, to put in the stents, which is a less invasive way.
Common Conditions Requiring Biliary Stenting
Several conditions may need biliary stents, including:
- Bile duct obstruction caused by gallstones, tumors, or inflammation.
- Cholangitis, an infection of the bile duct, which can be a result of obstruction.
- Biliary leaks following surgery or trauma.
- Malignancies affecting the bile ducts, such as cholangiocarcinoma.
These issues can really affect a person’s life. Biliary stenting is a good way to manage symptoms and improve health outcomes.
Types of Liver Stents and Selection Criteria

Choosing the right liver stent is complex. It depends on the patient’s health and the type of blockage. There are two main types: plastic and metal bile duct stents.
Plastic Bile Duct Stents: Temporary Solutions
Plastic stents are for short-term use. They work well when the blockage might clear up or with treatment. Made from plastic, they are easy to put in and take out during a procedure. They’re good for benign conditions or temporary blockages. But, they might clog more often and need to be replaced more.
Metal Bile Duct Stents: Long-term Options
Metal stents are for long-term use, often for cancer blockages. Made from metal, they last longer. They’re more reliable and less likely to clog than plastic stents. This makes them better for patients needing long-term drainage.
Factors Influencing Stent Selection
Choosing between plastic and metal stents depends on several things. These include the blockage type, the patient’s health, and how long the stent will be needed. Other factors are the patient’s outlook, any underlying health issues, and future treatment needs. We team up with patients and doctors to pick the best stent for each person.
Understanding liver stents and how to choose them helps manage liver diseases better. The selection process looks at the patient’s condition, the blockage type, and the stent’s benefits and risks.
Medical Indications for Liver Stent Placement
Doctors decide to place a liver stent for several reasons. This procedure helps with many biliary issues. It improves patients’ lives and health.
Managing Jaundice and Bile Duct Obstruction
Jaundice is a big reason for using liver stents. It happens when bile can’t flow right. This causes yellow skin and eyes. A stent helps bile flow again, fixing jaundice and improving liver health.
A study in the Journal of Clinical Gastroenterology showed stents help with jaundice. They fix bile flow, easing symptoms and protecting the liver.
Treating Cholangitis and Preventing Infection
Cholangitis is another reason for stents. It’s an infection in the bile ducts. Stents help drain infected bile, treating the infection and stopping it from coming back.
“Biliary stenting is an effective method for managing cholangitis by ensuring proper drainage of the bile ducts and preventing bacterial growth.”
– Expert Opinion
Addressing Malignancies Affecting the Bile Ducts
Cancer can block bile ducts. Stents help manage symptoms in these cases. They improve life quality by fixing bile flow and easing symptoms.
| Malignancy Type | Symptoms | Benefits of Stenting |
| Pancreatic Cancer | Jaundice, weight loss, abdominal pain | Palliation of symptoms, improved quality of life |
| Cholangiocarcinoma | Jaundice, pruritus, weight loss | Restoration of bile flow, symptom relief |
Resolving Gallstone-Related Complications
Gallstones can block bile ducts, causing problems. Stents might be used to manage these issues. This is when other treatments don’t work.
Knowing these reasons helps doctors decide if a stent is right for a patient. It ensures the best care for biliary problems.
Preparing for Your Liver Stent Procedure
To get ready for your liver stent procedure, you’ll need to do some tests and follow certain steps. Your healthcare provider will tell you what to do. This is key for a successful procedure and your safety.
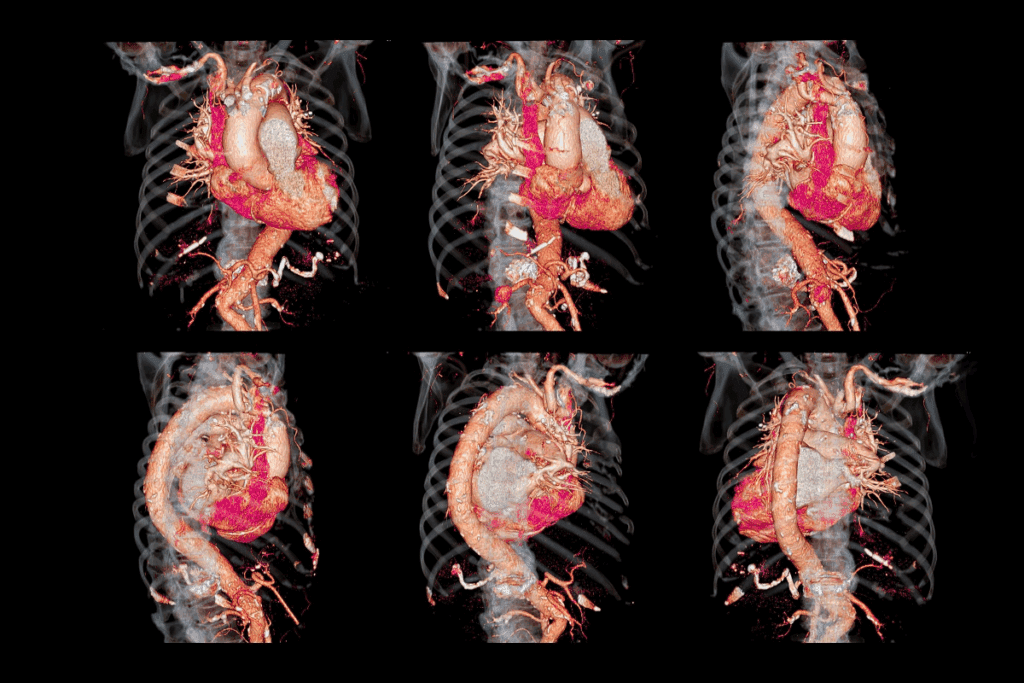
Required Diagnostic Tests and Imaging
Before your procedure, you’ll have to go through some tests and imaging. These help check your bile ducts and the area around them. You might have:
- Ultrasound: This test shows pictures of your bile ducts and finds any blockages.
- CT Scan: It gives detailed pictures of your abdomen to find where the blockage is.
- MRCP (Magnetic Resonance Cholangiopancreatography): This MRI focuses on your bile and pancreatic ducts without dye.
- ERCP (Endoscopic Retrograde Cholangiopancreatography): It’s used to see inside your bile and pancreatic ducts.
Medication Adjustments Before the Procedure
Your doctor might change your medicines before the procedure. This is important for:
- Blood Thinners: You might stop or lower your dose to avoid bleeding risks.
- Diabetes Medications: Your doctor will adjust these to keep your blood sugar right during fasting.
Fasting and Other Pre-procedure Instructions
You’ll need to fast for a few hours before the procedure. This is to keep your stomach empty during sedation. Your doctor will tell you:
- Fasting Duration: How long you should not eat or drink.
- Hydration: You might be allowed to drink clear liquids until a certain time.
- Pre-procedure Medications: You might take special medicines to get ready.
Here’s a table with a typical pre-procedure plan:
| Pre-procedure Instruction | Details |
| Fasting | Avoid food and drink for at least 8 hours before the procedure |
| Medication Adjustment | Stop blood thinners 2 days prior; adjust diabetes medications as advised |
| Arrival Time | Arrive at the hospital 2 hours before the scheduled procedure time |
Questions to Ask Your Healthcare Provider
It’s important to ask your doctor any questions you have. This will help you feel more ready and comfortable. You might ask:
- About the Procedure: What does it involve? What are the expected results?
- About Risks and Complications: What could go wrong, and how will it be handled?
- Post-procedure Care: What do you need to do after the procedure? How can you manage any pain?
By following these steps, you can make sure you’re ready for your liver stent procedure. This will help reduce risks and improve your chances of a good outcome.
The Liver Stent Procedure: What to Expect
Getting a liver stent can seem scary, but knowing what to expect helps a lot. We’ll walk you through each step, from getting ready to getting better.
Endoscopic Placement via ERCP
Endoscopic Retrograde Cholangiopancreatography (ERCP) is a common way to put in a liver stent. It uses a flexible tube with a camera and tools to reach the bile duct through your mouth.
We use dye to see the bile duct and find the blockage. Then, we put in the stent to help bile flow again.
“ERCP has revolutionized the management of bile duct obstructions, making it a minimally invasive solution with high success rates.”
Percutaneous Transhepatic Approach
For some, a percutaneous transhepatic approach is better. This method goes through the skin to reach the bile duct with imaging help.
This is good for high obstructions or when ERCP can’t be used. We’ll talk about the best option for you.
| Procedure | Description | Advantages |
| ERCP | Endoscopic access through the mouth | Minimally invasive, high success rate |
| Percutaneous Transhepatic | Access through the skin | Useful for high obstructions, alternative to ERCP |
Anesthesia Options and Sedation
We offer different anesthesia options and sedation to keep you comfortable. The choice between sedation and general anesthesia depends on your health and the procedure’s complexity.
Our anesthesiologists work with our gastroenterologists to make sure you’re safe and comfortable.
Typical Duration and Hospital Stay
The duration of the liver stent procedure varies, usually from 30 minutes to a few hours. It depends on how complex the case is.
Most patients can go home the same day or after a short stay. But, some might need to stay longer if they have other health issues.
Getting a liver stent is tough, but with the right info and care, you can face it with confidence. Our team is here to give you the best care and support every step of the way.
Benefits and Outcomes of Liver Stent Management
Effective liver stent management is key for the best patient results and a better life quality. Knowing the benefits and outcomes helps patients make smart choices about their care.
Immediate Symptom Relief
Liver stent placement quickly relieves symptoms like jaundice and pruritus. It restores bile flow, reducing discomfort from bile duct blockage. Patients often see a quick improvement, making daily activities easier.
Restoration of Bile Flow and Liver Function
Liver stents are vital for bile flow, essential for digestion and liver health. They ensure bile flows freely into the intestine, keeping liver function good. This leads to better nutrient absorption and overall health.
Quality of Life Improvements
Liver stent placement greatly improves a patient’s life quality. It eases symptoms and restores bile flow, allowing for a better life. Many patients feel more energetic and need less hospital time, living more normally and actively.
Comparison with Alternative Treatment Options
When looking at treatments for bile duct blockage, comparing liver stent benefits with other options is key. While surgery and other methods have their uses, liver stenting is a less invasive option with fewer risks and quicker recovery. This comparison helps patients and doctors choose the best treatment.
Potential Risks and Complications of Liver Stents
It’s important for patients to know about the risks of liver stents before they decide to get one. Liver stents are usually safe and work well, but there can be problems.
Infection and Cholangitis Risk Factors
Infection is a big risk after getting a liver stent. Cholangitis, an infection of the bile duct, can happen because of bacteria on the stent. Risks include not cleaning the stent well, placing it wrong, and having a blockage in the bile duct.
Risk factors for cholangitis include:
- Incomplete drainage of bile
- Stent occlusion
- Previous history of cholangitis
Bleeding and Perforation Concerns
Bleeding and perforation can happen during or after the procedure. Bleeding might happen because of the bile duct being touched during the procedure. Perforation is a risk when putting in the stent or guidewire.
| Complication | Description | Risk Factors |
| Bleeding | Hemorrhage during or after procedure | Anticoagulant use, trauma during procedure |
| Perforation | Tear or hole in the bile duct or surrounding tissue | Difficulty during stent placement, guidewire trauma |
Stent Migration and Displacement
Stent migration is when the stent moves from where it was placed. This can cause problems like not draining well or blocking the bile duct. Reasons for migration include the wrong size stent, not fixing it right, and changes in the bile duct.
Stent Occlusion and Blockage
Stent occlusion is when the stent gets blocked. This can cause jaundice or cholangitis to come back. Blockage can happen from sludge, tumors, or food. It’s important to keep an eye on the stent and clean it out to avoid this.
Knowing about these risks helps doctors and patients work together to avoid them. Regular check-ups and care are key to managing liver stents well.
Essential Aftercare Following Liver Stent Placement
After a liver stent is placed, care is key. It helps avoid problems and ensures the best results. We’ll cover the important steps of aftercare, from the first hours to getting back to normal.
Immediate Post-Procedure Recovery
The first hours after a liver stent are very important. Patients are watched closely for any issues. “It’s vital to catch and fix problems quickly,” doctors say.
Patients might feel some pain, which doctors can help with. It’s a good idea to have someone with you at home for a few hours. Rest for the rest of the day, and slowly start doing things again as you feel better.
Medication Management and Pain Control
Managing your meds is key for pain and to avoid problems. Doctors will give you meds for pain, infection, or other needs. Always take your meds as told, and talk to your doctor about any side effects.
- Take medications exactly as prescribed, without skipping doses.
- Report any side effects or concerns to your healthcare provider.
- Do not stop medication without consulting your doctor.
Dietary Guidelines and Nutritional Considerations
Your diet is important after a liver stent. Eating light, balanced meals can help you feel better and heal faster. Start with small meals and slowly get back to your usual diet.
Nutritional Considerations:
- Stay hydrated by drinking plenty of fluids.
- Avoid heavy, greasy, or spicy foods that can cause discomfort.
- Choose foods that are high in nutrients and easy to digest.
Activity Restrictions and Gradual Return to Normal
Start doing more as you feel better. Rest is important, but too much can cause problems. Here’s what to do:
- Avoid heavy lifting, bending, or strenuous activities for a few days.
- Gradually resume normal activities, including work, as advised by your healthcare provider.
- Listen to your body and not push beyond what feels comfortable.
By following these tips, you can recover smoothly and avoid complications. Always talk to your doctor for specific advice.
When to Seek Medical Attention After Stent Placement
It’s important to know when to get medical help after a liver stent is placed. You should watch out for complications and know when to get urgent care.
Warning Signs of Infection
Infection is a serious issue after a liver stent is put in. Look out for fever, chills, and stomach pain. If you have these symptoms, get medical help fast. Also, watch for jaundice, as it could mean infection or a blocked stent.
Symptoms of Stent Blockage
A blocked stent is a big problem that needs quick action. Watch for dark urine, light-colored stools, and jaundice coming back. If you see these signs, call your doctor right away.
Indications of Stent Migration
Stent migration means the stent moves from where it was placed. Signs include bad stomach pain, vomiting, and trouble breathing. If you have these symptoms, get medical help fast.
Emergency Situations Requiring Immediate Care
Some situations need you to get medical help right away. These include severe stomach pain, heavy bleeding, or signs of shock like dizziness and fainting. If you’re experiencing these, don’t wait to get help.
Watching your health after a liver stent and knowing when to get medical help is key. It can help prevent serious problems. Always talk to your doctor if you’re worried about your symptoms or health.
Conclusion
Managing a liver stent well is key for those with biliary blockage. We’ve talked about the different stents, like plastic and metal ones. Each has its own good points and downsides.
The way to put in a stent, through ERCP or a direct approach, needs careful thought and skill.
Good liver stent care means knowing the risks, like infections and bleeding. Following aftercare advice helps avoid these problems. This includes taking medicine, eating right, and not overdoing it.
Biliary stenting is a big help for those with blockages. Knowing the pros and cons of stent placement helps patients make smart choices. Taking care of a liver stent right means a team effort. We hope this article helps both patients and doctors.
FAQ
What is a liver stent and what is its purpose?
A liver stent, also known as a bile duct stent, is a small, hollow tube. It is inserted into the bile duct to restore bile flow into the intestine. This treats obstructions caused by various conditions.
What are the types of liver stents available?
There are two main types of liver stents: plastic and metal. Plastic stents are used for temporary relief. Metal stents are used for long-term management, mainly for malignant obstructions.
How is a liver stent placed?
A liver stent can be placed through endoscopic retrograde cholangiopancreatography (ERCP) or a percutaneous transhepatic approach. Both methods are effective for restoring bile flow.
What are the benefits of having a liver stent?
The benefits of liver stent management include immediate relief from symptoms like jaundice and pruritus. It restores bile flow and improves liver function. This leads to a better quality of life.
What are the potentials risks and complications associated with liver stents?
Potential risks and complications include infection and cholangitis, bleeding, stent migration, and stent occlusion. Understanding these risks is key to minimizing them and managing them effectively.
How do I prepare for a liver stent procedure?
To prepare for a liver stent procedure, you’ll undergo diagnostic tests and imaging. You’ll also adjust medications as needed, fast, and follow other pre-procedure instructions from your healthcare provider.
What aftercare is required following liver stent placement?
Proper aftercare includes immediate post-procedure recovery care and effective medication management. You should follow dietary guidelines and gradually return to normal activities. This ensures a smooth recovery and minimizes the risk of complications.
When should I seek medical attention after liver stent placement?
You should seek medical attention if you experience warning signs of infection, symptoms of stent blockage or migration, or other emergency situations that require immediate care.
What are the signs of stent blockage or migration?
Signs of stent blockage or migration include recurring jaundice, abdominal pain, fever, or other symptoms that indicate a problem with the stent. Prompt medical attention is necessary if you experience these symptoms.
Can I manage my liver stent at home?
While many aspects of liver stent management can be handled at home, it’s important to follow the specific instructions provided by your healthcare provider. Seek medical attention if you experience any concerning symptoms.
How does a liver stent impact my quality of life?
A liver stent can significantly improve your quality of life. It relieves symptoms, restores bile flow, and improves liver function. This allows for a more normal and active life.
Are there alternative treatment options to liver stents?
Alternative treatment options may be available depending on the underlying cause of the bile duct obstruction. Your healthcare provider can discuss the most appropriate treatment options for your specific condition.
What is the role of ERCP in liver stent placement?
ERCP is a procedure used to place a liver stent. It allows direct access to the bile ducts through the mouth. This enables the restoration of bile flow without the need for external incisions.
References
- Parlak, E., & Yilmazlar, T. (2015). Biliary stenting for benign and malignant biliary obstruction: A review of current status and future prospects. World Journal of Gastroenterology, 21(26), 7860-7872.