Getting ready for liver stent placement is key to fixing bile flow issues and avoiding problems. At Liv Hospital, we know how vital this step is. We’re here to offer top-notch care and help with all you need as an international patient.
Liver stent placement, or biliary stent placement, is a small surgery to fix bile duct blockages. These blockages can be from tumors, gallstones, or strictures. By putting in a biliary stent, we help bile flow right again. This improves liver function and relieves symptoms.
Key Takeaways
- Learn about the procedure and its benefits before surgery.
- Liver stent placement is a vital fix for bile duct blockages.
- The surgery involves putting in a biliary stent to fix bile flow.
- Liv Hospital offers full support and guidance for international patients.
- Our team is committed to giving you the best care possible.
Understanding Biliary Stent Procedures

Biliary stenting is a key medical procedure. It helps restore bile flow in blocked bile ducts. A thin, flexible tube called a biliary stent is placed to ensure bile flows well from the liver to the intestine. We’ll look into the details of biliary stents, why they’re needed, and the different types available.
What Is a Biliary Stent?
A biliary stent is a device that keeps the bile duct open. This allows bile to flow freely. Bile duct blockages can happen due to tumors, gallstones, or inflammation. A stent helps bypass these blockages, improving bile flow and easing symptoms like jaundice and itching.
Common Conditions Requiring Biliary Intervention
Several conditions may need a biliary stent. These include:
- Pancreatic cancer: Tumors can block the bile duct, requiring a stent.
- Gallstones: Large stones can block the bile duct, needing intervention.
- Bile duct strictures: Narrowing of the bile duct can block bile flow.
- Cholangiocarcinoma: Cancer of the bile duct can cause blockages.
Types of Biliary Stents Available
Biliary stents are made of plastic or metal. Plastic stents are cheaper but may need to be replaced often. Metal stents are more durable and come in uncovered and covered types. Uncovered metal stents can have tumor growth, while covered stents prevent this but may move more easily.
Choosing the right biliary stent is key for good patient care. Our medical team picks the best stent for each patient based on their condition and needs.
When Is Liver Stent Placement Necessary?

When bile ducts get blocked, a liver stent is often needed to fix the problem. This blockage can happen for many reasons. Knowing why it happened helps doctors choose the right treatment.
Diagnosing Bile Duct Blockages
Doctors use imaging and tests to find blockages in bile ducts. Ultrasound, CT scans, and MRI help see where and how bad the blockage is. Endoscopic Retrograde Cholangiopancreatography (ERCP) lets them look directly at the bile ducts to find the cause.
Symptoms Indicating Need for Intervention
Patients with blockages often show certain symptoms. These include jaundice, abdominal pain, pruritus (itching), dark urine, and clay-colored stools. Sometimes, they might also have signs of infection, like cholangitis, which is very serious and needs quick action.
Conditions Treated with Biliary Stenting
Biliary stenting helps with many problems that block bile ducts. Issues like pancreatic cancer, cholangiocarcinoma, and metastatic disease can press on or block the ducts. Even things like strictures or gallstones can cause problems and are treated with stents. Stenting helps bile flow again, making patients feel better and live better lives.
Benefits and Success Rates of Liver Stent Surgery
Liver stent surgery is a top choice for treating liver issues. It has high success rates and brings a lot of relief to patients. Thanks to new stenting methods, patient results have greatly improved.
Symptom Relief and Quality of Life Improvements
This surgery helps a lot, like easing jaundice and itching. It makes life better for those with liver problems. It helps bile flow again, easing the pain of blockages.
Key benefits include:
- Significant reduction in jaundice and itching
- Improved digestion and nutritional absorption
- Enhanced overall well-being and quality of life
Technical Success Rates
The success rate of liver stent placement is very high. Studies show bile flow is restored in most patients. This is thanks to better stents and skilled doctors.
Clinical Outcomes Data
Data shows biliary stenting helps in cancer blockages. It improves patient results. Studies confirm high success rates, leading to better survival and life quality.
| Outcome Measure | Success Rate | Clinical Benefit |
| Technical Success | 95% | Effective bile flow restoration |
| Symptom Relief | 85% | Reduction in jaundice and itching |
| Quality of Life | 80% | Improved overall well-being |
Potential Risks and Complications
Like any medical treatment, liver stent placement has risks and complications. The procedure is usually safe and works well. But knowing these risks helps you make smart choices about your health.
Short-Term Complications
Right after or soon after the procedure, you might face some issues. These can include:
- Infection: There’s a chance of getting an infection with a biliary stent.
- Bleeding: Some people might bleed during or after the procedure.
- Pancreatitis: This is inflammation of the pancreas, more likely with certain procedures.
A study in the Journal of Clinical Gastroenterology found early complications in 5% to 15% of patients. This depends on the patient and the procedure details.
Long-Term Complications
Complications can also show up later, weeks, months, or even years after the stent is placed. These might include:
- Stent Occlusion: The stent can get blocked, needing more procedures to fix.
- Stent Migration: The stent might move, causing more problems.
| Complication | Description | Typical Management |
| Stent Occlusion | Blockage of the stent, potentially causing jaundice or cholangitis. | Clearing or replacing the stent via endoscopic procedures. |
| Stent Migration | Movement of the stent from its intended position. | Repositioning or removing the stent, potentially requiring additional stents. |
Risk Factors to Discuss with Your Doctor
Some things can make complications more likely. Talk about these with your doctor:
- Previous history of pancreatitis or biliary disorders.
- Presence of other medical conditions, such as diabetes or heart disease.
- Any allergies or sensitivities to materials used in the stent or procedure.
“Understanding the risks and complications of biliary stent placement is key for patient education and informed consent. Doctors should talk about these with patients to ensure they know what to expect.”
— Medical Expert, Gastroenterologist
Knowing about these risks helps patients prepare for the procedure and recovery. It’s also important to follow your doctor’s advice carefully to lower these risks.
Pre-Procedure Medical Evaluations
Before starting a liver stent placement, we do important checks. These help us figure out the best way to help you. We look at your health and what’s causing the blockage.
Required Blood Tests
Blood tests are key in these checks. They show how well your liver is working. We check for signs of blockage, like high bilirubin and alkaline phosphatase levels. Medical Expert, a top gastroenterologist, says, “Blood tests tell us a lot about your liver. They help us make a treatment plan just for you.”
Imaging Studies
We use CT scans or MRI to see the bile ducts. These images help us find where the blockage is. Thanks to new imaging, we can do better treatments. This means better results for you.
Consultation with Specialists
Talking to specialists is important. They include gastroenterologists and interventional radiologists. They look at your history and test results together. They make a plan just for you.
We make sure you’re ready for the stent placement. This way, we can avoid problems and get the best results. “A good plan is essential for a smooth recovery,” Medical Expert, an expert in interventional radiology, says.
Preparing for Your Liver Stent Placement
Getting ready for your liver stent placement is key. Your healthcare team will help you with everything you need to do. This includes changing your medications, following special diets, and more.
Medication Adjustments
Some medicines might need to be changed or stopped before your procedure. Blood thinners, like warfarin or clopidogrel, may be paused to lower bleeding risks. Tell your doctor about all your medicines, including ones you buy without a prescription, to get the right advice.
“Always listen to your doctor about changing medicines to stay safe during the procedure,” advises a top gastroenterologist.
Dietary Restrictions
What you eat before your procedure is also important. You might need to not eat for a few hours before, usually starting at midnight the night before. This makes sure your stomach is empty, which is safer during the procedure.
Your doctor will tell you exactly how to fast and what else to avoid eating. It’s very important to follow these rules to avoid problems.
What to Bring to the Hospital
When you go to the hospital for your procedure, bring a few things to make your stay better. These include:
- Your insurance cards and ID
- A list of your current medicines
- Comfortable clothes
- Any personal items you might need
Being prepared helps you relax and focus on getting better.
By following these tips and working with your healthcare team, your liver stent placement will go well.
The Day Before Biliary Stent Surgery
Your biliary stent surgery is just a day away. It’s important to follow the final preparation guidelines. We want to make sure you’re ready for a smooth procedure and recovery.
Final Preparation Steps
The day before your surgery, finish any remaining tasks. This includes:
- Confirming your arrival time and hospital details
- Arranging for someone to drive you home after the procedure
- Packing a small bag with essentials like comfortable clothing and any necessary documents
By doing these tasks, you can focus on resting and preparing mentally.
Fasting Requirements
Fasting is a key part of preparing for your surgery. You will typically be asked to stop eating and drinking by midnight the night before. This makes sure your stomach is empty, which is safer during the procedure. We know fasting can be hard, but it’s very important for your safety.
Mental Preparation and What to Expect
Mental preparation is as important as physical. Knowing what to expect can help reduce anxiety. We suggest:
- Reviewing the steps involved in the biliary stent placement
- Discussing any concerns or questions with your healthcare provider
- Visualizing a positive outcome and focusing on your recovery
As one of our patients said,
“Knowing what to expect made all the difference; it helped me stay calm and focused on my recovery.”
By following these guidelines and staying informed, you’ll be ready for your surgery. If you have any questions or concerns, reach out to your healthcare team.
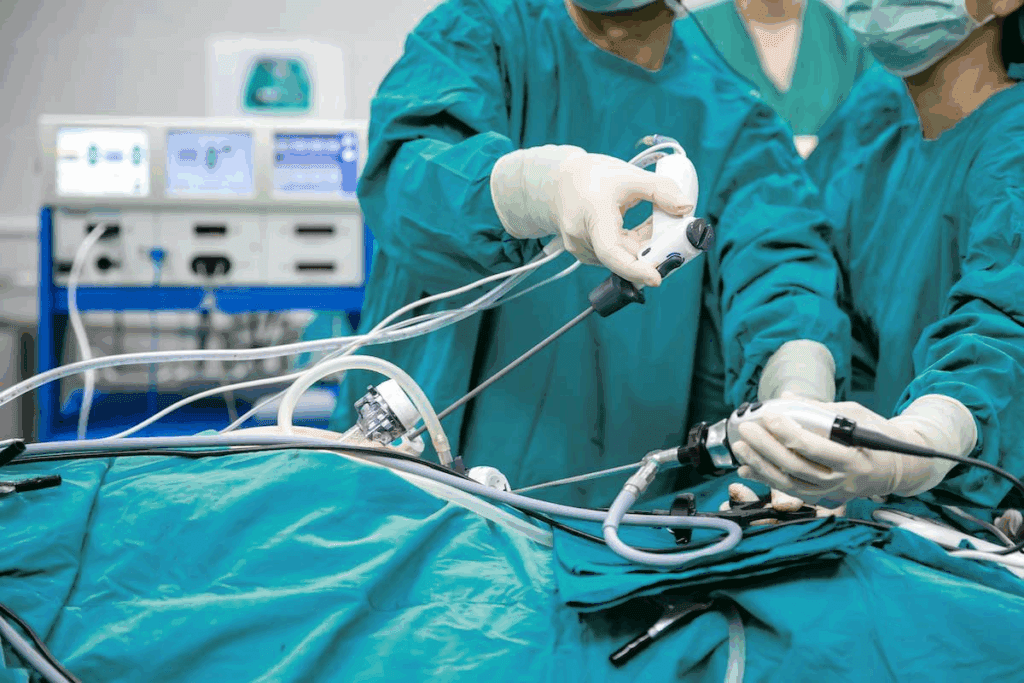
Step-by-Step Liver Stent Placement Procedure
Liver stent placement is a new way to treat biliary obstructions. It’s a minimally invasive procedure with several key steps. These steps are important for its success.
Anesthesia Administration
The first step is giving anesthesia to make sure the patient is comfortable. We use conscious sedation or general anesthesia, based on the patient’s condition and the procedure’s complexity.
Accessing the Biliary System
To access the biliary system, we use ERCP or PTC. ERCP is a common method that lets us see and access the bile ducts directly.
Stent Deployment Techniques
After gaining access, we deploy the stent. Stent deployment techniques use a balloon to widen the blocked area. Then, a stent is placed to keep the bile duct open. The stent can be plastic or metal, depending on the patient’s needs.
Procedure Duration and Patient Experience
The procedure’s length varies, from 30 minutes to a few hours. Patients are closely monitored, and we do our best to reduce discomfort. The experience can differ based on the case’s complexity and the patient’s health.
| Procedure Step | Description | Duration |
| Anesthesia Administration | Conscious sedation or general anesthesia | 15-30 minutes |
| Accessing Biliary System | ERCP or PTC | 30-60 minutes |
| Stent Deployment | Balloon dilation and stent placement | 30-60 minutes |
Common Bile Duct (CBD) and Gallbladder Stenting Techniques
Stenting procedures for the CBD and gallbladder are key in treating biliary obstructions. These methods help restore bile flow into the intestine. This relieves symptoms caused by bile duct blockages.
Endoscopic Retrograde Cholangiopancreatography (ERCP)
ERCP is a common method for reaching the biliary system. It uses an endoscope to go through the mouth, esophagus, and stomach to the duodenum. This allows us to place CBD stents directly into the bile duct without skin puncture.
ERCP has many benefits:
- It’s a minimally invasive procedure.
- It lets us see the bile ducts directly.
- It allows for both diagnosis and treatment at the same time.
Percutaneous Transhepatic Cholangiography (PTC)
PTC is used when ERCP isn’t possible. It involves inserting a needle through the skin into the liver to reach the bile ducts. We use PTC for external drainage or when ERCP can’t relieve the obstruction.
PTC has its advantages:
- It’s effective for certain bile duct obstructions.
- It allows for bile drainage outside the body.
- It can be used with other treatments.
Gallbladder Stent Placement Methods
Gallbladder stenting is for patients who can’t have cholecystectomy or other treatments. We use different methods for gallbladder stent placement, guided by imaging. The method chosen depends on the patient’s condition and the type of obstruction.
Important things to consider for gallbladder stenting include:
- Choosing patients based on clinical criteria.
- Using imaging for precise stent placement.
- Watching for possible complications.
Understanding these techniques helps us choose the best treatment for CBD and gallbladder obstructions in each patient.
Immediate Post-Procedure Care
After your liver stent placement, taking care of yourself is key. We watch over you closely to catch any problems early.
Recovery Room Monitoring
After the procedure, you’ll go to the recovery room. Our team will keep an eye on your health and look for any issues. This is important for a smooth start to your recovery.
Key aspects of recovery room monitoring include:
- Watching your heart rate, blood pressure, and oxygen levels
- Checking how much pain you’re in and helping with pain relief
- Looking out for signs of bleeding or allergic reactions
Pain Management Strategies
Managing your pain is a big part of your care after the procedure. We know everyone feels pain differently. Our team will work to make you as comfortable as possible. We might use medicine, other therapies, or a mix of both.
Some ways we manage pain include:
- Giving you pain medicine
- Using PCA pumps for you to control your pain
- Trying non-medical ways to help you relax or change your position
Initial Activity Restrictions
After your procedure, you’ll need to follow some activity rules. These rules are temporary and help you heal safely.
Initial activity restrictions may include:
- Not lifting heavy things or doing hard work
- Not bending or straining too much
- Not driving or using heavy machinery until your doctor says it’s okay
When You Can Return Home
When you can go home depends on how you’re doing and if you can take care of yourself. Usually, people go home the same day or the next day, depending on their situation.
Before you leave, we’ll give you all the details on how to care for yourself at home. This includes how to take your medicine, when to come back for follow-ups, and what to watch for. It’s important to follow these instructions to have a good recovery.
Recovery Timeline After Biliary Tract Stent Placement
After getting a biliary tract stent, patients go through a recovery process. This includes care right after the procedure and changes over time. Knowing this timeline helps manage expectations and ensures a smooth recovery.
Immediate Post-Procedure Care
The first 24 hours are key for watching for any problems. Patients stay in a recovery room for a few hours. Pain management is a big focus, with meds given as needed to reduce pain.
“The first 24 hours are critical,” says a medical expert. “We watch closely to catch any issues early and keep the patient safe and comfortable.”
First Week of Recovery
In the first week, patients might need to slow down and manage any pain or side effects. It’s important to follow the dietary guidelines given by doctors. This helps avoid putting too much stress on the biliary system.
- Start doing normal activities again as your doctor says.
- Watch for signs of problems like fever, severe pain, or jaundice.
- Stick to the medication plan given by your doctor.
Long-Term Adjustment
After the first recovery phase, patients start to get used to the stent. This involves making lifestyle changes and regular check-ups. These visits are key for making sure the stent works right and for catching any new problems.
Follow-up Appointments Schedule
Follow-up visits are a big part of care after the procedure. They let doctors check how the stent is doing and watch for any issues. The schedule for these visits is made just for the patient’s needs and the details of their procedure.
“Regular follow-up is essential to ensure the stent is working as intended and to address any concerns or complications early on,” emphasizes a healthcare professional.
By following the recovery timeline, patients can get the best results and lower the chance of problems after getting a biliary tract stent.
Conclusion
Liver stent placement is a key treatment for bile duct blockages. It brings relief and boosts quality of life. Knowing what to expect before, during, and after can help patients feel more prepared.
At Liv Hospital, we focus on giving our patients the best care. Our team helps address concerns and guides each patient through the process. This ensures the best results from biliary stent surgery.
With the right preparation and care, patients can see big improvements in their health and life quality. We aim to provide top-notch healthcare and support. Our goal is to make a real difference in our patients’ lives.
FAQ
What is a biliary stent and how is it used in liver stent placement?
A biliary stent is a thin, flexible tube put in the bile duct. It helps bile flow again. This is used to treat blockages like tumors, gallstones, and strictures. It improves liver function and relieves symptoms.
What are the different types of biliary stents available for liver stent placement?
There are plastic and metal stents, each with its own benefits. The right stent depends on the patient’s condition and the blockage type.
What are the symptoms that indicate the need for liver stent placement?
Symptoms like jaundice, itching, and abdominal pain show the need for biliary intervention. These signs are often due to blockages from tumors, gallstones, or strictures.
What are the benefits of liver stent surgery?
Liver stent surgery brings relief from jaundice and itching. It also improves quality of life. Most patients see effective bile flow restoration.
What are the potentials risks and complications associated with liver stent placement?
While safe, risks include infection, bleeding, pancreatitis, stent blockage, or migration. Discussing these risks with a doctor is key.
How do I prepare for liver stent placement?
Preparation involves adjusting medications and following dietary restrictions. Knowing what to bring and expect can reduce anxiety.
What happens during the liver stent placement procedure?
The procedure includes anesthesia, accessing the biliary system, and stent deployment. Understanding these steps helps patients know what to expect.
What is the recovery timeline after biliary tract stent placement?
The recovery time varies but follows a general pattern. The first 24 hours are critical for monitoring. Recovery continues over the next week and beyond.
What is the difference between ERCP and PTC for biliary stent placement?
ERCP accesses the biliary system directly without skin puncture. PTC uses skin access under imaging. The choice depends on the patient’s needs and blockage type.
How is pain managed after liver stent placement?
Pain management is tailored to each patient. It may include medication and other interventions to ensure comfort during recovery.
When can I return home after liver stent placement?
The decision to go home depends on the patient’s condition and any complications. Patients are monitored before discharge. They must follow doctor’s instructions for care and follow-up.
What follow-up care is required after biliary stent placement?
Follow-up appointments are essential to check the stent’s function and manage complications. The schedule is based on individual needs.
References
- Centers for Disease Control and Prevention. (2023). Management of biliary tract infections and complications. CDC Liver Health Facts. Retrieved from https://www.cdc.gov/liverdisease/biliary-management.html