
The ‘5-second test’ for lung cancer has become popular on social media. It claims a simple finger check can show if you have the disease. But, it’s important to know this method has no scientific proof.
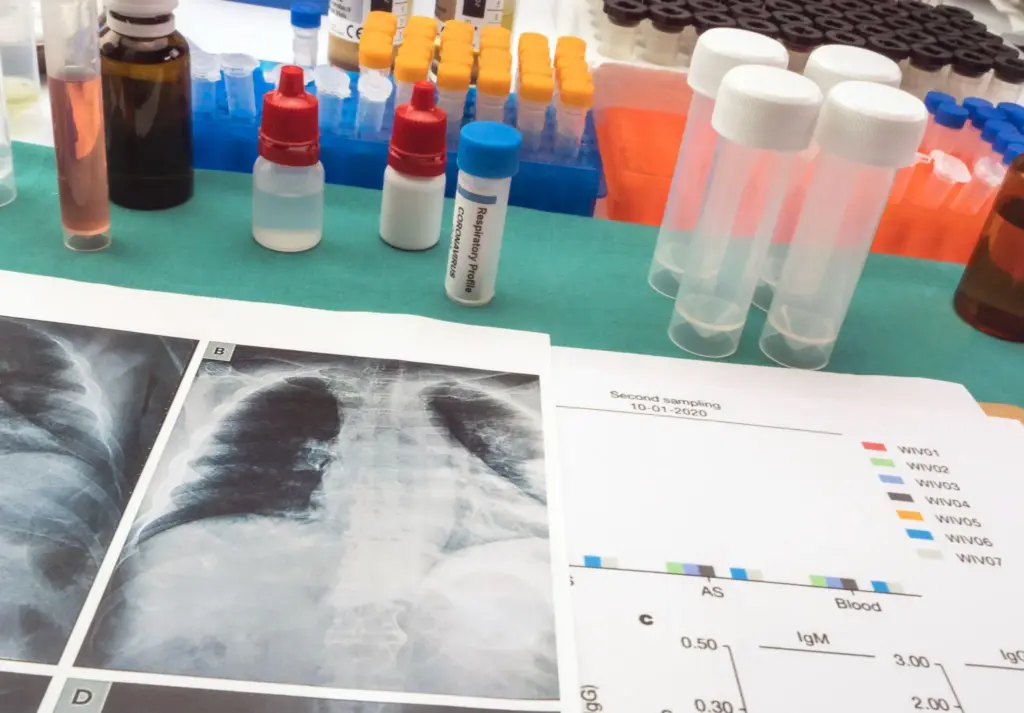
Healthcare experts say to stick with proven screening methods. Quest Diagnostics research shows Low-Dose Computed Tomography (LDCT) is great for catching lung cancer early.
Symptoms like finger clubbing might hint at lung cancer. But, only doctors can give a sure diagnosis. They use methods backed by science.
Key Takeaways
- The ‘5-second test’ lacks scientific backing and should not be relied upon for diagnosis.
- LDCT screening is a proven method for early detection of lung cancer.
- Symptoms like finger clubbing may indicate lung issues, but only medical professionals can provide an accurate diagnosis.
- Quest Diagnostics research supports the use of LDCT for lung cancer screening.
- Relying on evidence-based screening methods is key for finding diseases effectively.
The Viral 5-Second Breath Test: Myth vs. Reality

The ‘5-second breath test’ has become popular online, but its truth is debated. This test, where you hold your breath for five seconds, is said to show lung health. But where did this idea come from, and why do people like it so much?
Origins of the Social Media Claim
The ‘5-second breath test’ started on social media, where people share their results. But, there’s no scientific proof it works for lung cancer or other serious health issues. Social media can spread false information fast, without checking facts or credible sources.
Why People Are Drawn to Simple Tests
People like quick, easy solutions for health problems. The ‘5-second breath test’ is simple and offers quick answers. But, lung cancer needs a full medical check, not just a simple test. It involves detailed tests like imaging and biopsies, not just holding your breath.
Finger clubbing, or nail clubbing, might hint at lung cancer, but it’s not enough to diagnose. Club fingers and lung cancer have been linked, but this symptom alone is not enough. A real diagnosis needs a doctor’s evaluation, imaging, and lab tests.
We should be careful about online tests, like the ‘5-second breath test’, for serious diseases like lung cancer. It might seem harmless, but it can cause worry or false peace. Always talk to doctors for the right diagnosis and treatment.
Scientific Evidence Against the 5-Second Test
The 5-second test is popular on social media but lacks scientific proof. Medical experts worry it might spread wrong information. This could cause people to delay getting a real diagnosis or try to diagnose themselves.
Lack of Clinical Validation
The 5-second test hasn’t been tested in clinical trials. It’s not as reliable as low-dose computed tomography (LDCT). LDCT has been shown to lower lung cancer death rates through studies like the National Lung Screening Trial.
LDCT can find lung cancer early, which helps people live longer. But the 5-second test has no scientific backing. It’s based on untested claims and lacks research support.
|
Diagnostic Method |
Clinical Validation |
Impact on Mortality |
|---|---|---|
|
Low-Dose CT (LDCT) |
Proven through National Lung Screening Trial |
Reduces lung cancer mortality |
|
5-Second Test |
No clinical validation |
Potential for delayed diagnosis |
Potential Dangers of Self-Diagnosis
Using untested methods like the 5-second test can be risky. It might give people false peace of mind or cause too much worry. This could make them wait too long to see a doctor, which might harm their health.
We urge people not to try to diagnose themselves. Instead, follow the medical guidelines for screening. Using proven methods like LDCT is key to catching lung cancer early and saving lives.
Understanding Lung Cancer: Basic Facts
Lung cancer is a common cancer worldwide. Knowing its types and risk factors helps improve treatment. It’s key to understand this disease well for better early detection and treatment.
Types of Lung Cancer
Lung cancer is mainly divided into two types: Non-Small Cell Lung Cancer (NSCLC) and Small Cell Lung Cancer (SCLC). NSCLC makes up about 85% of cases. It includes adenocarcinoma, squamous cell carcinoma, and large cell carcinoma. SCLC is more aggressive and often linked to smoking.
Risk Factors and Prevalence
Many factors increase lung cancer risk. Smoking is the biggest cause, leading to 80-90% of lung cancer deaths. Exposure to asbestos, radon gas, and secondhand smoke also raises risk. Genetic mutations and family history matter too.
In the U.S., only 6.6% of eligible patients get screened for lung cancer. Knowing these risk factors is vital for prevention and early detection. Symptoms like a persistent cough, chest pain, and unexplained weight loss may signal lung cancer. Finger clubbing, where fingertips enlarge, is a sign of lung cancer, often in advanced stages.
With more awareness and screening, we can tackle lung cancer better. By learning about lung cancer, including its types and risk factors, we aim to improve patient care and reduce the disease’s impact worldwide.
Medically Approved Screening Methods for Lung Cancer
Early detection is key in fighting lung cancer. A specific screening method has become the top choice. Lung cancer is a common cancer globally, and screening high-risk people is vital.
Low-Dose Computed Tomography (LDCT)
Low-Dose Computed Tomography (LDCT) is a top tool for lung cancer screening. It uses less radiation than standard CT scans, making it safer for regular use. Research shows LDCT can cut lung cancer deaths in high-risk groups.
We suggest LDCT for those who fit certain criteria. It can find lung cancer early, when it’s easier to treat. The National Lung Screening Trial found LDCT can lower lung cancer death rates by up to 20% in high-risk people.
Who Should Get Screened and When
Not everyone needs lung cancer screening. We advise LDCT for those at high risk. This includes current or former smokers, aged 55 to 74, with a history of heavy smoking.
Deciding to get screened should be a talk with a healthcare provider. They’ll consider your risk and medical history. It’s also key to know the benefits and risks of screening, like false positives and the need for more tests.
By catching lung cancer early, we can improve treatment success and survival rates. LDCT screening is a big step forward in early lung cancer detection and care.
The National Lung Screening Trial: Evidence for LDCT
The National Lung Screening Trial (NLST) was a key study that showed LDCT’s benefits in lung cancer screening. It was done in the United States. It compared LDCT with chest X-ray to see which was better at lowering lung cancer deaths in high-risk groups.
Study Design and Findings
The NLST included over 53,000 people aged 55-74. They were either smokers or had quit in the last 15 years. They were split into two groups: one got LDCT scans, and the other got chest X-rays for three years.
The study found that LDCT led to a 20% drop in lung cancer deaths compared to chest X-rays. The LDCT group also saw a 6.7% drop in all deaths.
Impact on Screening Guidelines
The NLST’s results changed lung cancer screening rules. It showed that LDCT is better for those at high risk. Now, the U.S. Preventive Services Task Force (USPSTF) suggests LDCT for people aged 50-80 with a 20 pack-year smoking history.
These guidelines are based on the NLST’s findings. LDCT is now a key part in finding and treating lung cancer early.
Lung Cancer Early Stage Finger Clubbing: An Important Warning Sign
Finger clubbing can be a warning sign for lung cancer. It’s a condition where fingers and fingernails change shape. We’ll look into what it is, its link to lung cancer, and how to spot it.
What is Finger Clubbing?
Finger clubbing makes fingers look bigger and nails curved. It’s a sign of health problems, like lung cancer. The exact cause is not known, but it might be related to blood flow and oxygen.
The Physiological Connection to Lung Cancer
The link between finger clubbing and lung cancer is not fully understood. Some think lung cancer changes blood flow, causing clubbing. Others believe tumor chemicals might play a role. While research continues, it’s key to see clubbing as an early warning.
How to Identify Clubbing
To spot finger clubbing, look for specific signs. These include:
- Enlargement of the fingertips
- Curvature of the nails
- Softening of the nail bed
- An increased angle between the nail and the nail bed
The Schamroth window test can help check for clubbing. Place fingernails of opposite fingers together. If there’s no diamond-shaped window, it might be clubbing.
While clubbing can hint at lung cancer, it’s not the only cause. If you notice unusual finger or nail changes, see a doctor for a check-up.
The Complete Finger Clubbing Assessment
Checking for finger clubbing is key in spotting lung cancer early. Clubbing makes the fingertips bigger and can mean several health issues, including lung cancer. To assess clubbing well, we need to know the methods and what they mean.
The Schamroth Window Test Technique
The Schamroth Window Test is a well-known way to check for clubbing. It’s done by placing the fingernails of opposite hands together. Without clubbing, a diamond shape shows between the nails. If this shape is missing or smaller, it means clubbing is present.
This test is simple and doesn’t hurt, making it great for doctors and non-doctors alike. But, it’s important to look at it with other tests too.
Digital Photography for Monitoring Changes
Digital photos are also used to watch for clubbing changes. Doctors take clear pictures of the fingers often. This is good for people who have had lung cancer or are at high risk.
Photos help see small changes in the fingers early. This is very helpful when used with other tests. It makes checking for clubbing better.
|
Assessment Method |
Description |
Advantages |
|---|---|---|
|
Schamroth Window Test |
A technique involving the comparison of fingernails to assess clubbing |
Simple, non-invasive, and effective |
|
Digital Photography |
Monitoring changes in finger morphology through photographs |
Allows for detailed comparison and tracking of changes over time |
In summary, checking for finger clubbing needs both old and new methods. The Schamroth Window Test and digital photos help doctors find lung cancer early. This way, they can catch and watch the disease better.
Other Physical Signs and Symptoms of Early Lung Cancer
It’s important to know the physical signs and symptoms of early lung cancer. This knowledge helps in getting medical help early. Some people might not show symptoms early on, but others may notice signs that point to lung cancer.
Respiratory Symptoms
Respiratory symptoms are often the first signs of lung cancer. These can include:
- A persistent cough that does not go away
- Coughing up blood or rust-colored sputum
- Shortness of breath or wheezing
- Chest pain that worsens with deep breathing, coughing, or laughing
It’s essential to note that these symptoms can also be associated with other less serious conditions. If you have any of these symptoms that last, see a healthcare professional for an evaluation.
Systemic Symptoms
Systemic symptoms affect the whole body and can be signs of lung cancer. Some symptoms include:
|
Symptom |
Description |
|---|---|
|
Unexplained weight loss |
Losing weight without trying, which can be a sign of advanced cancer |
|
Loss of appetite |
A decrease in appetite can lead to weight loss and other complications |
|
Fatigue |
Feeling extremely tired or weak, which can interfere with daily activities |
These systemic symptoms can be non-specific and may not immediately suggest lung cancer. If you’re experiencing a mix of these symptoms, it’s important to get medical advice.
Knowing the physical signs and symptoms of early lung cancer can help in early detection and treatment. If you’re worried about symptoms, don’t wait to talk to a healthcare professional.
Early Detection and Survival Rates
Lung cancer survival rates greatly depend on when it’s found. Finding it early is key to better survival chances.
Stage 1 Lung Cancer Survival Statistics
Being diagnosed with Stage 1 lung cancer means a much better chance of survival. The 5-year survival rate for Stage 1 is much higher than for Stage 4.
Here are some important statistics:
|
Stage at Diagnosis |
5-Year Survival Rate |
|---|---|
|
Stage 1 |
60-80% |
|
Stage 4 |
5-10% |
The Dramatic Difference in Late-Stage Diagnosis
The difference in survival rates between early and late stages is huge. Finding lung cancer late makes the outlook much worse. This shows how vital early detection is.
Early detection is key to better lung cancer survival rates. Knowing about lung cancer stages and the importance of early detection helps us improve patient outcomes.
Lung Cancer Staging and Its Importance
Knowing the stage of lung cancer is key to finding the right treatment. Staging lung cancer means checking how far the disease has spread. This helps doctors guess how well a patient will do and plan their care.
The TNM Classification System
The TNM system is a common way to stage lung cancer. It looks at three main things: the tumor’s size and spread (T), nearby lymph nodes (N), and if the cancer has spread (M). This helps doctors stage lung cancer accurately and plan the best treatment.
The TNM system works like this:
|
TNM Factor |
Description |
|---|---|
|
T (Tumor) |
Size and extent of the primary tumor |
|
N (Node) |
Involvement of nearby lymph nodes |
|
M (Metastasis) |
Presence of metastasis |
How Staging Affects Treatment Decisions
Lung cancer staging is very important for treatment choices. The disease’s stage tells doctors what treatments to use. For example, early-stage lung cancer might just need surgery. But for more advanced cases, treatments like chemotherapy and radiation might be needed too.
“Accurate staging is essential for selecting the most effective treatment strategy and improving patient outcomes.” –
A leading oncologist
We use the TNM system to make treatment choices. This way, we make sure our patients get the best care for their lung cancer. Knowing the stage helps us predict how well a patient will do and tailor their treatment plan.
Barriers to Proper Lung Cancer Screening
Many people at risk for lung cancer don’t get screened. This is a big problem. Early detection through screening can save lives, but many don’t get checked.
Low Screening Rates in the United States
In the U.S., not enough people get lung cancer screenings. Only a small number of those who should get screened actually do. This shows a big problem in healthcare.
There are many reasons for this:
- Not enough people know about lung cancer screening.
- It’s hard to find places to get screened, mainly in rural areas.
- Cost is a big issue, with high prices and not enough insurance.
- Some people don’t understand what screening is or how it helps.
Access and Awareness Issues
We need to make lung cancer screening more accessible and well-known. Special efforts are needed to fix these problems. Here are some ideas:
- Start public education campaigns to teach more about screening.
- Make screening easier to get by using community programs or mobile units.
- Make it easier for doctors to recommend screenings.
- Help with the cost by changing policies or providing financial help.
By working on these issues, we can help more people get screened. This could lead to finding lung cancer earlier and saving lives.
The Diagnostic Journey After a Suspicious Finding
When a suspicious finding happens, doctors work together to find the right diagnosis and treatment. They use many tests to see if lung cancer is present and how far it has spread.
Follow-up Tests and Procedures
Several tests are done after a suspicious finding. These tests help confirm lung cancer and understand its stage. Some of these include:
- Imaging Tests: Tests like PET scans, MRI, or CT scans are used to see the lungs clearly. They check if the cancer has spread.
- Biopsy: A biopsy takes a lung tissue sample for a microscope check. It’s the best way to confirm lung cancer.
- Pulmonary Function Tests (PFTs): PFTs check how well the lungs work. They help decide the best treatment.
Here’s a table showing common tests and their purposes:
|
Test |
Purpose |
|---|---|
|
PET Scan |
Checks metabolic activity in the body, helping find cancer spread |
|
Biopsy |
Provides a definitive diagnosis by examining tissue samples |
|
PFTs |
Evaluates lung function to guide treatment decisions |
The Multidisciplinary Approach to Diagnosis
A team of experts is key in lung cancer diagnosis and treatment. This team includes:
- Pulmonologists
- Thoracic Surgeons
- Medical Oncologists
- Radiation Oncologists
- Radiologists
- Pathologists
They review test results, talk about treatment options, and create a plan for the patient. This teamwork ensures the patient gets the best care possible.
Treatment Options for Different Stages of Lung Cancer
The stage of lung cancer is key in choosing the right treatment. Every patient’s journey with lung cancer is different. Treatment plans are made to fit the specific needs of each disease.
Early-Stage Treatment Approaches
For early-stage lung cancer, the goal is to cure the disease. Surgery is often the first step to remove the tumor and affected lymph nodes. For those who can’t have surgery, stereotactic body radiation therapy (SBRT) is sometimes used.
After surgery, chemotherapy or targeted therapy might be added. This is to kill any cancer cells left behind. The choice of treatment depends on the lung cancer type and its genetic makeup.
Advanced-Stage Treatment Strategies
For advanced-stage lung cancer, the focus is on controlling the disease and improving life quality. Systemic therapies like chemotherapy, targeted therapy, and immunotherapy are common. The treatment choice depends on the tumor’s genetic profile and the patient’s health.
In some cases, palliative care is added to the treatment plan. It helps manage pain, shortness of breath, and other symptoms. This improves the patient’s comfort and well-being.
|
Lung Cancer Stage |
Primary Treatment Options |
Additional Therapies |
|---|---|---|
|
Early Stage (I-II) |
Surgery, SBRT |
Adjuvant chemotherapy, targeted therapy |
|
Advanced Stage (III-IV) |
Systemic therapies (chemotherapy, targeted therapy, immunotherapy) |
Palliative care, symptom management |
Lung cancer treatment is complex and tailored to each patient. Our teams work with patients to create personalized plans. These plans address the unique needs and situations of each patient.
Liv Hospital’s Approach to Lung Cancer Detection and Treatment
Liv Hospital focuses on finding lung cancer early and treating it with a team effort. We aim to give top-notch healthcare to everyone, including international patients. This ensures that each person gets the best care possible.
Multidisciplinary Pathways
At Liv Hospital, we know that treating lung cancer well needs a team effort. Our team includes experts in oncology, surgery, radiology, and pathology. We create treatment plans that fit each patient’s needs.
Our team works together smoothly to give patients full care from start to finish. This means every patient gets the best care possible.
|
Specialty |
Role in Lung Cancer Care |
|---|---|
|
Oncology |
Develops and implements chemotherapy and targeted therapy plans. |
|
Thoracic Surgery |
Performs surgical interventions for lung cancer, including tumor resections. |
|
Radiology |
Provides diagnostic imaging and image-guided interventions. |
|
Pathology |
Conducts tissue diagnosis and molecular testing to guide treatment decisions. |
Advanced Screening Protocols
Liv Hospital uses the latest technology for lung cancer screening, like low-dose CT scans. Our screening methods are designed to find lung cancer early. This makes it easier to treat.
Early detection is key to improving survival rates. We work hard to find lung cancer early through our screening and education programs.
By using the latest technology and focusing on the patient, Liv Hospital aims to improve lung cancer detection and treatment. Our goal is to give the best care to our patients every step of the way.
Preventive Measures and Risk Reduction
To lower lung cancer risk, we need to change our lifestyle and know about environmental dangers. Understanding and tackling key risk factors can greatly reduce disease chances.
Smoking Cessation Programs
Smoking causes most lung cancer deaths, about 80 to 90 percent. Smoking cessation programs are key to preventing lung cancer. They provide support and tools to help quit, like counseling and medication.
Good smoking cessation programs can help smokers quit more often. We suggest using both behavioral therapy and medication to handle withdrawal and cravings.
Environmental Risk Management
Other environmental factors can also raise lung cancer risk. These include radon, asbestos, and harmful substances. Radon, a gas found naturally, is a big risk after smoking.
Managing these risks means testing homes for radon and avoiding asbestos. We also need to limit exposure to harmful substances at work and home. Stronger rules and awareness campaigns can help.
Combining smoking cessation with managing environmental risks can cut lung cancer cases. It’s a team effort that needs everyone’s help.
Conclusion
Lung cancer is a serious and often deadly disease. It needs quick attention and the right screening. Early detection is key to better survival rates.
Knowing the risks and symptoms is important. Using tests like Low-Dose Computed Tomography (LDCT) helps. This way, we can fight lung cancer better.
Spreading the word about lung cancer is vital. Education helps people take care of their health. This includes getting screened for lung cancer early.
Early detection leads to better treatment and more lives saved. It’s a big step in the fight against lung cancer.
Places like Liv Hospital use a team approach to fight lung cancer. They use the latest in screening and treatment. This helps a lot in managing lung cancer.
Our aim is to create a culture of health awareness. We want to use new medical tools to help patients live longer. This is our goal.
FAQ
What is the “5 second test” for lung cancer?
The “5 second test” is a claim on social media. It says a simple breath test can find lung cancer. But, this test has no scientific proof and is not a real way to diagnose lung cancer.
Is finger clubbing a reliable indicator of lung cancer?
Finger clubbing might be an early sign of lung cancer. But, it’s not only found in lung cancer. If you see any odd changes in your fingers or nails, see a doctor.
What is the Schamroth Window Test, and how is it used?
The Schamroth Window Test checks for finger clubbing. You place your fingernails together to see if there’s a diamond-shaped window. If it’s smaller or missing, it might mean clubbing.
What are the risk factors for developing lung cancer?
Lung cancer risks include smoking and being around harmful substances like asbestos and radon. Family history and some genetic changes also play a part. Knowing these risks helps in preventing and catching lung cancer early.
How is lung cancer staged, and why is it important?
Lung cancer is staged using the TNM system. It looks at the tumor size, lymph nodes, and if it has spread. Knowing the stage helps doctors choose the best treatment and predict the outcome.
What is Low-Dose Computed Tomography (LDCT), and who should undergo screening?
LDCT is a safe way to screen for lung cancer. It uses low radiation to see the lungs clearly. People who smoked a lot or have other risk factors should get screened between 55 and 74 years old.
What are the treatment options for lung cancer?
Lung cancer treatments depend on the cancer’s stage and type, and the patient’s health. Options include surgery, chemotherapy, radiation, targeted therapy, or a mix of these.
How can I reduce my risk of developing lung cancer?
To lower lung cancer risk, avoid smoking and harmful substances, live healthily, and get screened if needed. Also, manage environmental risks and stay up-to-date on lung health.
What is the significance of early detection in lung cancer?
Finding lung cancer early greatly increases survival chances. Early diagnosis means treatment is more likely to work, leading to better survival rates.
How does Liv Hospital approach lung cancer detection and treatment?
Liv Hospital uses a team effort for lung cancer care. We use the latest screening methods and tailor treatment plans for each patient to get the best results.
References:
• National Cancer Institute. (n.d.). Lung cancer detection, diagnosis, and staging. Retrieved from https://www.cancer.org/cancer/types/lung-cancer/detection-diagnosis-staging/screening.html





