Last Updated on November 13, 2025 by
The relationship between blood cancer and low platelets is discussed, including the role of autoimmune thrombocytopenia in some cases.
Thrombocytopenia, or low platelet count, can be a sign of lymphoma, mainly in blood cancers. Platelets are key for blood clotting. Without enough, bleeding can become a serious issue.
We look into how thrombocytopenia and lymphoma are linked. This includes what causes it, its symptoms, and how to treat it. Research shows that about 25% of lymphoma patients with VTE face severe thrombocytopenia.
It’s important for both patients and doctors to understand this link. Thrombocytopenia means not enough platelets in the blood. This can cause serious bleeding problems.
Key Takeaways
- Thrombocytopenia can be a symptom and complication in lymphoma.
- Low platelet count is associated with bleeding complications.
- Severe thrombocytopenia occurs in about 25% of lymphoma patients with VTE.
- Understanding thrombocytopenia and lymphoma is key for effective management.
- Thrombocytopenia affects patient outcomes and guides management decisions.
Understanding Thrombocytopenia and Lymphoma
To understand the link between thrombocytopenia and lymphoma, we need to know about both. Thrombocytopenia means having too few platelets in the blood, which can cause bleeding. Lymphoma is a cancer that affects the immune system, mainly the lymphatic system.
What is thrombocytopenia?
Thrombocytopenia happens when platelets are below 150,000 per microliter of blood. It can be caused by many things, like not making enough platelets or losing them too fast. Severe thrombocytopenia is a big worry because it can cause bleeding on its own. About 25% of lymphoma patients with VTE have severe thrombocytopenia.
What is lymphoma?
Lymphoma is a cancer of the lymphatic system, which is part of our immune system. It happens when lymphocytes grow out of control. There are two main types: Hodgkin lymphoma and non-Hodgkin lymphoma, each needing different treatments.
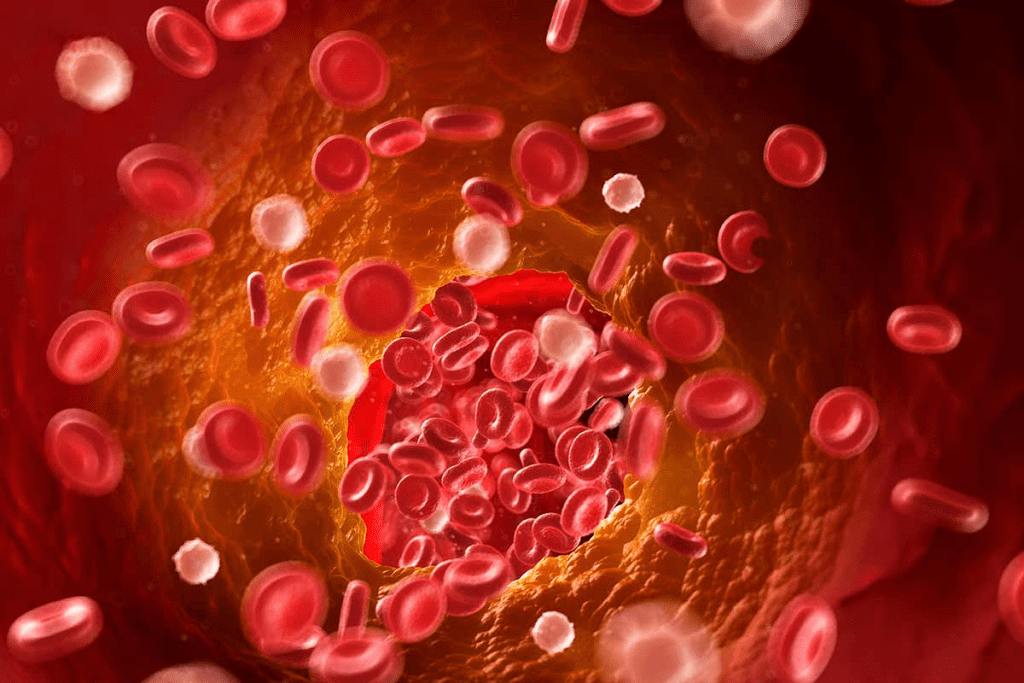
The relationship between blood disorders and cancer
The connection between thrombocytopenia and lymphoma is complex. In lymphoma patients, thrombocytopenia can be caused by many things. These include lymphoma cells in the bone marrow, the spleen holding onto platelets, and side effects from treatments like chemotherapy and radiotherapy. Knowing these causes is key to managing thrombocytopenia in lymphoma patients.
The Prevalence of Thrombocytopenia in Lymphoma Patients
Thrombocytopenia, or low platelet count, is a big worry for lymphoma patients. It makes treating lymphoma harder and can hurt the patient’s quality of life.
Statistical Overview
Research shows thrombocytopenia is common in lymphoma patients. About 7% of those with diffuse large B-cell lymphoma (DLBCL) get severe thrombocytopenia from chemotherapy. The exact rate varies based on the type of lymphoma and treatment.
Thrombocytopenia can come from the lymphoma itself, chemotherapy, or autoimmune issues. Knowing these causes helps doctors manage it better.
Variations Across Lymphoma Subtypes
Thrombocytopenia rates differ among lymphoma types. For example, aggressive lymphomas like DLBCL often see more cases due to the disease and strong chemotherapy.
On the other hand, some slow-growing lymphomas might see fewer severe cases. But the risk is always there, and treatments can play a big role. Autoimmune thrombocytopenia (ITP) is rare but serious, needing special care.
Risk Factors for Developing Low Platelet Counts
Several factors increase the risk of thrombocytopenia in lymphoma patients. These include the lymphoma’s type and stage, how intense the chemotherapy is, past treatments, and the bone marrow’s health.
Patients with advanced lymphoma or those getting very strong chemotherapy are at higher risk. Keeping a close eye on platelet counts is key to catching and treating thrombocytopenia early.
Knowing how common and what causes thrombocytopenia in lymphoma patients helps doctors plan better treatments. This approach aims to fight the lymphoma well and reduce the risks of low platelet counts.
Mechanisms Behind Lymphoma-Associated Thrombocytopenia
Thrombocytopenia in lymphoma comes from many factors. These include direct and indirect effects on platelet production and survival. Knowing these factors is key to helping lymphoma patients.
Bone Marrow Infiltration
Lymphoma cells in the bone marrow cause thrombocytopenia. These cells take over the bone marrow, stopping normal platelet production. This leads to fewer platelets in the blood.
“The bone marrow is the factory where platelets are produced,” says, a hematologist. “When lymphoma cells infiltrate the marrow, it’s like a factory shutdown “ platelet production comes to a halt.”
Splenic Sequestration
The spleen can also play a role in thrombocytopenia. An enlarged spleen due to lymphoma traps more platelets. This reduces the number of platelets in the blood, causing thrombocytopenia.
“Splenomegaly, or enlargement of the spleen, is a common complication in lymphoma patients. It can lead to sequestration of platelets, contributing to thrombocytopenia.”
Treatment-Related Causes
Lymphoma treatments, like chemotherapy and radiation, can also affect platelet production. These treatments weaken the bone marrow, causing thrombocytopenia. It’s important to manage this to avoid bleeding problems.
- Chemotherapy can suppress bone marrow, reducing platelet production.
- Radiation therapy, when aimed at the spleen or bone marrow, can also cause thrombocytopenia.
- Supportive care, like platelet transfusions, may be needed to manage treatment-related thrombocytopenia.
In conclusion, lymphoma-related thrombocytopenia is complex. Understanding its causes is vital for effective management.
Autoimmune Thrombocytopenia and Lymphoma Connection
The link between autoimmune thrombocytopenia (ITP) and lymphoma is complex. It’s important to understand how these conditions interact. In lymphoma patients, ITP is a rare but serious issue. It happens when the immune system attacks platelets, causing their destruction.
Definition and Pathophysiology
ITP is when the immune system mistakenly attacks platelets. Platelets are key to blood clotting. This leads to low platelet counts and can cause bleeding.
Key aspects of ITP pathophysiology include:
- Autoantibody production against platelet surface glycoproteins
- Platelet destruction mainly occurs in the spleen
- Impaired platelet production due to immune effects on megakaryocytes
Incidence Rates in Different Lymphoma Types
ITP’s occurrence varies among lymphoma subtypes. Some lymphomas are more likely to have ITP. This makes it important to consider each subtype.
Chronic lymphocytic leukemia (CLL), a non-Hodgkin lymphoma, often sees autoimmune issues like ITP. The exact rates vary, but it’s key to watch for ITP in lymphoma patients.
“The development of autoimmune thrombocytopenia in lymphoma patients shows the complex relationship between the immune system and cancer.”
Autoimmune ITP as a Paraneoplastic Syndrome
ITP can be a paraneoplastic syndrome with lymphoma. This means ITP might be linked to the cancer. It could be due to immune system issues or other factors.
It’s vital to grasp the connection between ITP and lymphoma for better patient care. We need to be ready to handle ITP as a complication in lymphoma patients.
Types of Lymphoma Associated with Low Platelet Count
Thrombocytopenia, or low platelet count, is a big worry in many lymphoma types. Lymphoma can mess with how platelets are made and destroyed. This leads to a low platelet count.
Non-Hodgkin Lymphoma and Thrombocytopenia
Non-Hodgkin lymphoma (NHL) often leads to low platelet counts. This is because lymphoma cells can fill up the bone marrow. They can also get stuck in the spleen.
Bone marrow infiltration by lymphoma cells messes up how blood cells are made. Splenic sequestration happens when the spleen gets too big. Both of these can lower platelet counts.
Hodgkin Lymphoma and Platelet Disorders
Thrombocytopenia can happen in Hodgkin lymphoma, too, but it’s less common. It might be because the immune system attacks platelets. Or it could be because the bone marrow is not working properly.
Diffuse Large B-Cell Lymphoma (DLBCL)
DLBCL is a fast-growing type of NHL that can cause low platelet counts. Its quick growth can fill up the bone marrow. This makes it hard to make enough platelets.
- DLBCL can cause bone marrow infiltration, disrupting platelet production.
- Treatment regimens for DLBCL may also impact platelet counts.
T-Cell Lymphomas and Platelet Abnormalities
T-cell lymphomas are a mix of different lymphomas. They can also lead to low platelet counts. This is because of immune problems and bone marrow issues.
Knowing the type of lymphoma is key to managing low platelet counts. It helps doctors treat the problem better.
Clinical Presentation and Symptoms
It’s important to know how thrombocytopenia shows up in lymphoma patients. This condition, where platelet counts are low, can cause serious symptoms. These symptoms can be life-threatening.
Common Signs of Thrombocytopenia
People with thrombocytopenia might see bleeding issues. Some common signs include:
- Bruising: Easy bruising or purpura can occur due to minor trauma.
- Petechiae: Small, pinpoint spots on the skin, often appearing on the lower extremities.
- Bleeding Gums: Gingival bleeding, especially during brushing or flossing.
- Nosebleeds: Frequent or prolonged epistaxis.
- Heavy Menstrual Bleeding: Menorrhagia in women can be a significant concern.
These symptoms can vary in severity. They might be more noticeable in those with severe thrombocytopenia.
When to Suspect Lymphoma in Patients with Low Platelets
Thrombocytopenia can have many causes, but in lymphoma patients, it’s a red flag. We should think about lymphoma if a patient has low platelets and shows:
- Unexplained Weight Loss: Significant weight loss without a clear cause.
- Night Sweats: Recurring night sweats, often accompanied by fever.
- Lymphadenopathy: Swollen lymph nodes, which can be tender or painless.
- Fatigue: Persistent and unexplained tiredness.
These symptoms, along with thrombocytopenia, might point to lymphoma.
Severity Classification
The severity of thrombocytopenia depends on the platelet count:
- Mild: Platelet count between 100,000 and 150,000/ µL.
- Moderate: Platelet count between 50,000 and 100,000/ µL.
- Severe: Platelet count below 50,000/ µL.
- Life-threatening: Platelet count below 20,000/ µL, associated with a high risk of spontaneous bleeding.
Diagnostic Approach to Thrombocytopenia in Lymphoma
To diagnose thrombocytopenia in lymphoma patients, we use several tools. We combine lab tests, bone marrow exams, and imaging studies. This helps us find the cause of thrombocytopenia.
Laboratory Tests
Laboratory tests are key in diagnosing thrombocytopenia. A complete blood count (CBC) is the first step. It counts platelets, red blood cells, and white blood cells.
A study in the American Academy of Family Physicians says, “thrombocytopenia is diagnosed when the platelet count is less than 150,000/μL” . We also do blood smears to check platelet shape and rule out other issues.
Bone Marrow Examination
A bone marrow exam is essential for lymphoma patients with thrombocytopenia. It looks at the bone marrow’s cells to see how they’re made and if there are any problems. Experts say, “bone marrow biopsy is key for diagnosing and staging lymphoma” and helps find thrombocytopenia’s cause.
Imaging Studies
Imaging studies like CT and PET scans help us see how far lymphoma has spread. They show how the spleen and other organs might be affecting platelet counts. “Imaging is vital for diagnosing and staging lymphoma,” helping us plan the best treatment.
Treatment Strategies for Lymphoma Patients with Low Platelet Count
Managing lymphoma with low platelet counts is complex. It involves treating the cancer and the low platelet count. A good plan looks at the cancer, how low the platelets are, and the patient’s health.
Managing the Underlying Lymphoma
It’s key to treat the lymphoma to help the platelet count. Chemotherapy, radiation, and immunotherapy are common ways to fight cancer. They can also help with the low platelet issue.
Platelet Transfusions
Platelet transfusions are often used for low platelet counts. They add platelets to the blood to prevent bleeding. They’re used in emergencies or when bleeding risk is high.
Thrombopoietin Receptor Agonists
Thrombopoietin receptor agonists (TPO-RAs) boost platelet production. They help increase platelet counts, reducing the need for transfusions. They’re a good choice for lymphoma patients with low platelets.
Immunosuppressive Therapies
Immunosuppressive therapies can also help with low platelet counts. They calm the immune system’s attack on platelets. They’re used when the low platelets are caused by the immune system.
Using these strategies, we can manage low platelet counts in lymphoma patients. This reduces bleeding risks and improves their health.
Chemotherapy-Induced Thrombocytopenia in Lymphoma Treatment
Chemotherapy-induced thrombocytopenia is a big worry for lymphoma patients. It happens when platelet levels drop too low, causing bleeding. We’ll look at how certain treatments lead to this, why it’s important to watch platelet counts, and how to handle the risks.
Common Chemotherapy Regimens and Their Impact on Platelets
Some chemotherapy plans are more likely to cause low platelet counts. For example, treatments with gemcitabine and cisplatin can increase this risk. Knowing which drugs are used can help predict and manage this side effect.
Monitoring Protocols During Treatment
It’s key to keep an eye on platelet counts during chemo. Blood tests are done regularly to check these levels. Doctors might change how often these tests are done based on how well the treatment is working and the specific drugs used.
Dose Modifications and Treatment Delays
If thrombocytopenia gets too bad, treatments might need to be adjusted or delayed. This balance helps treat the lymphoma without risking too much bleeding. Changing treatment plans can help manage low platelet counts while keeping up the fight against lymphoma.
Managing Bleeding Risks During Therapy
It’s vital to manage bleeding risks for lymphoma patients on chemo. Patients are taught to recognize signs of bleeding, like bruises or tiny spots. Sometimes, platelet transfusions are needed to quickly raise platelet counts and lower bleeding risks.
Conclusion
It’s important to understand how thrombocytopenia and lymphoma are connected. Thrombocytopenia is when you have too few platelets in your blood. This is a big problem for people with lymphoma.
We’ve looked into how common thrombocytopenia is in lymphoma patients. We’ve also talked about how it happens and how to treat it. Knowing the signs of low platelets helps doctors give better care and reduce bleeding risks.
To manage thrombocytopenia well, doctors use several methods. They treat the lymphoma, give platelet transfusions, and use special medicines. A treatment plan made just for each patient can help them live better with lymphoma.
FAQ’s:
What is thrombocytopenia, and how is it related to lymphoma?
Thrombocytopenia is when you have too few platelets in your blood. This can cause bleeding problems. It’s a big issue for people with lymphoma, and how common it is depends on the type of lymphoma.
What are the mechanisms behind lymphoma-associated thrombocytopenia?
Lymphoma can cause low platelet counts in a few ways. The cancer can fill up the bone marrow, or the spleen can hold onto platelets. Treatment can also play a role.
What is autoimmune thrombocytopenia (ITP), and how is it related to lymphoma?
Autoimmune thrombocytopenia (ITP) is when your immune system attacks your platelets. This can lead to low platelet counts. It’s a rare but serious problem for lymphoma patients.
Which types of lymphoma are associated with low platelet count?
Some types of lymphoma, like non-Hodgkin and Hodgkin lymphoma, can cause low platelet counts. This includes diffuse large B-cell lymphoma (DLBCL) and T-cell lymphomas. Each type has its own risks and complications.
What are the common signs and symptoms of thrombocytopenia?
Signs of thrombocytopenia include bleeding easily, such as bruising or bleeding gums. How bad it is can vary. If you have low platelets, lymphoma could be a possibility.
How is thrombocytopenia diagnosed in lymphoma patients?
To diagnose thrombocytopenia in lymphoma patients, doctors use several tests. These include blood tests, bone marrow exams, and imaging studies. These help figure out why the platelet count is low.
What are the treatment strategies for lymphoma patients with low platelet count?
Treating lymphoma patients with low platelets involves a few steps. First, manage the lymphoma itself. Then, use treatments to boost platelet counts, like transfusions or special medicines.
How is chemotherapy-induced thrombocytopenia managed in lymphoma treatment?
Managing low platelets from chemotherapy means keeping an eye on platelet counts. Doctors might change the treatment plan or delay it to avoid bleeding. This helps keep patients safe.
What is the relationship between lymphoma treatment and autoimmune ITP?
Lymphoma treatment can impact autoimmune ITP. It’s important to manage ITP in these patients. Treatment for ITP might include medicines that suppress the immune system.
Can lymphoma patients with thrombocytopenia receive platelet transfusions?
Yes, platelet transfusions are an option for lymphoma patients with low platelets. But it depends on how low the platelets are and the patient’s overall health.
References
- Marin, L., et al. (2019). Immune thrombocytopenia and lymphoma: A rare but serious association. Hematology Reports, 11(2), 8059. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6935784/
- Hauswirth, A. W., et al. (2008). Autoimmune thrombocytopenia in non-Hodgkin’s lymphoma. Blood, 112(8), 3457-3463. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2491149/





