Last Updated on November 26, 2025 by Bilal Hasdemir

If you have chronic back pain that medicines and physical therapy can’t fix, medial branch ablation might help. This procedure is a small surgery that aims at the nerves causing pain in the spine’s facet joints. It offers long-lasting pain relief.
At Liv Hospital, a team of top experts uses the latest technology for personalized care. They use advanced imaging and focus on patient care. This makes medial branch ablation a very effective treatment.
Key Takeaways
- Medial branch ablation is a minimally invasive procedure for chronic back pain relief.
- The procedure targets the medial branch nerves supplying the facet joints.
- Advanced imaging guidance enhances the effectiveness of the treatment.
- Personalized care ensures the best possible outcomes for patients.
- Liv Hospital’s team is internationally recognized for their expertise.
The Growing Problem of Chronic Back Pain in America

Chronic back pain is a big health problem in the United States. It affects 84% of adults at some point in their lives. This condition not only lowers the quality of life for millions but also costs a lot for healthcare.
There are many reasons why people get chronic back pain. Knowing these reasons is key to finding good treatments.
Common Causes of Persistent Spinal Pain
Many things can lead to chronic back pain. These include:
- Degenerative changes in the spine, such as those from aging or wear and tear.
- Injury or trauma to the back can start a pain cycle.
- Poor posture or biomechanics, causing strain on the spine.
- Medical conditions like arthritis or spinal stenosis.
These causes often send pain through specific nerve paths.
The Role of Facet Joints in Back Pain
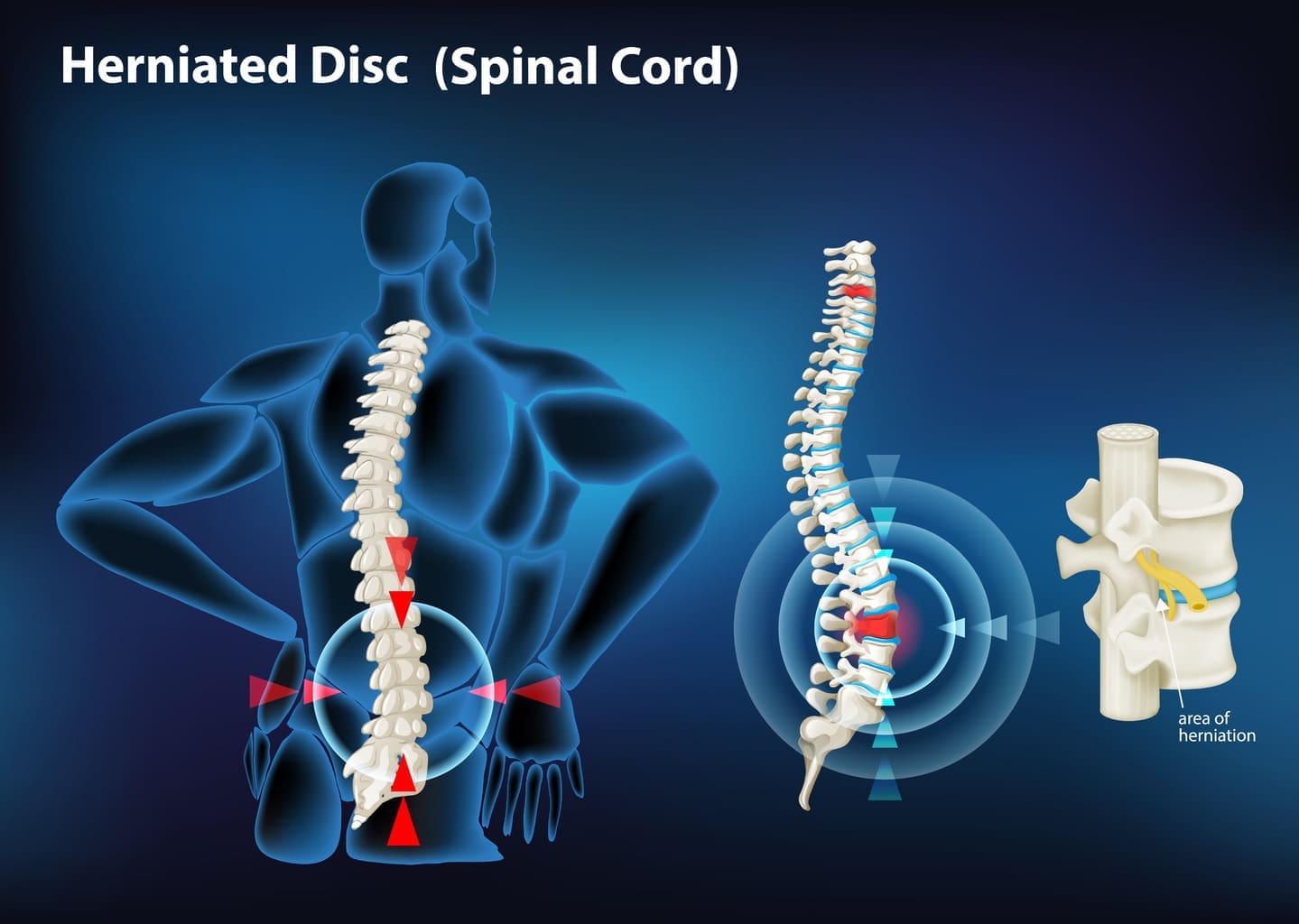
Facet joints, between the vertebrae, are key in chronic back pain. When these joints get inflamed or irritated, they cause pain. The nerves that connect to these joints, called medial branch nerves, send pain signals to the brain.
The role of facet joints and their nerves shows how complex chronic back pain is. It highlights the need for treatments that target these areas.
Medial Branch Ablation: A Breakthrough Procedure Explained

The medial branch ablation procedure is a big step forward in treating chronic back pain. It focuses on the medial branch nerves. These nerves carry pain signals from the facet joints to the brain.
Understanding Medial Branch Nerves
Medial branch nerves are key in sending pain signals from the facet joints. They branch from the spinal nerves and connect to the facet joints. Knowing how these nerves work is key to the success of the procedure. The goal is to target these nerves to stop pain signals.
How Ablation Interrupts Pain Signals
Medial branch ablation uses radiofrequency ablation to create heat the nerves. This heat stops pain signals from reaching the brain. It helps relieve chronic pain from the facet joints. This method is precise, which means it’s safe and effective.
Different Approaches to Nerve Ablation
There are several ways to do nerve ablation, like traditional and cooled radiofrequency ablation. Cooled radiofrequency ablation makes bigger lesions, which might make treatment more effective. The choice depends on the patient’s needs and the doctor’s choice. Each method has its benefits, and the right one is chosen for each case.
The medial branch ablation procedure is a major leap in treating chronic back pain. By understanding the nerves and how ablation works, doctors can help patients with facet joint pain.
Key Fact #1: The Science Behind Radiofrequency Ablation
Radiofrequency ablation works by using high-frequency waves to block pain signals. This method has changed how we treat chronic back pain. It offers a less invasive way to find relief that can last a long time.
Medial Branch Radiofrequency Ablation Process
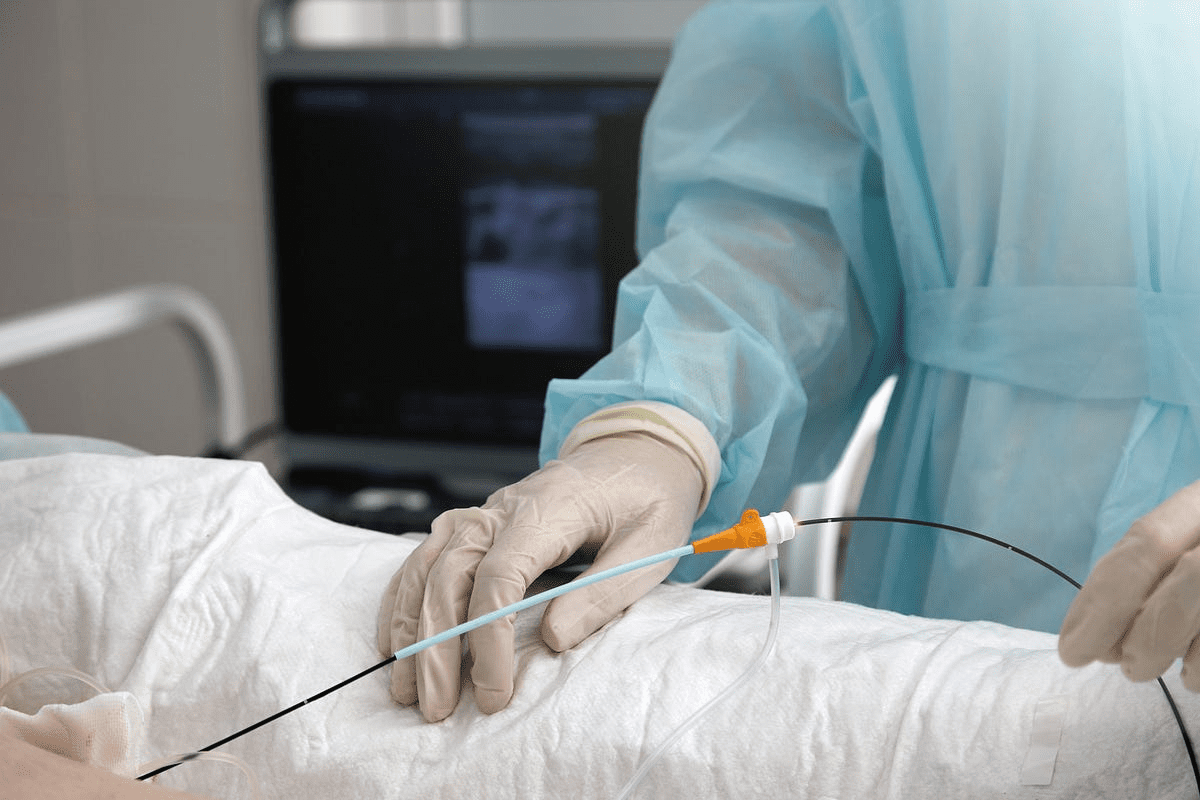
The process starts with the patient being placed in the right position. Then, local anesthesia is given to reduce pain during the procedure. A special needle is then guided to the nerves using X-ray images.
After that, the radiofrequency device is turned on. It sends out waves that heat the nerve tissue. This heat damages the nerve, stopping it from sending pain signals to the brain.
Creating Thermal Lesions for Pain Relief
When the nerve tissue is heated, it gets damaged. This stops pain signals from being sent. The damage is done carefully, thanks to modern imaging and technology.
The aim is to give durable pain relief without harming other tissues. This makes RFA a safe and effective treatment.
“Radiofrequency ablation has been shown to provide significant pain relief for patients with chronic back pain, improving their quality of life and functional ability.”
Precision and Effectiveness of RFA
RFA is precise and effective. It targets specific nerves to block pain. This reduces the chance of side effects and increases the chance of success.
Studies show RFA can greatly reduce pain for many people. But results can vary from person to person.
RFA’s success comes from creating long-lasting thermal lesions. These lesions block pain signals. This makes RFA a good choice for those who haven’t found relief with other treatments.
Key Fact #2: Diagnostic Blocks – The Critical First Step
Diagnostic blocks are a key first step in figuring out if medial branch ablation will help. Before the ablation, patients get a diagnostic block. This test checks if pain can be managed by blocking the medial branch nerves.
Medial Branch Blocks as Predictors of Success
Medial branch blocks help predict if radiofrequency ablation will work. They numb the nerves with a local anesthetic. This lets doctors see if the pain comes from these nerves.
If the block makes pain better, it shows the ablation might help too. The predictive value of diagnostic blocks is huge. They show if a patient is likely to benefit from the procedure.
The Diagnostic Block Procedure
The procedure involves injecting local anesthetic into the nerves under X-ray. This makes sure the anesthetic goes exactly where it should. It’s a quick process and can be done without staying overnight.
After the procedure, patients are watched to see how they react. They might rate their pain or report any changes in symptoms.
Interpreting Block Results
Understanding diagnostic block results is important. If pain goes away while the anesthetic is working, it means the nerves are likely causing the pain.
How long the pain relief lasts is also key. If relief lasts longer or is more intense, it points to the nerves asthe mainn pain source.
It’s important to remember that these tests aren’t 100% accurate. The placebo effect or anesthetic spreading can affect results. So, doctors must look at the whole picture when interpreting these tests.
Key Fact #3: Regional Applications in the Spine
Medial branch RFA has changed how we treat spinal pain. It targets pain in the neck, chest, and lower back. This makes it a great choice for many people with chronic back pain.
Cervical Medial Branch Radiofrequency Ablation
Cervical medial branch RFA helps those with chronic neck pain. It aims at nerves that control the facet joints in the neck. Precision is key here because of the area’s delicate structures.
“This method has been shown to greatly reduce pain in the neck,” studies say. It needs careful planning and skill to work best.
Thoracic Applications and Considerations
Thoracic medial branch RFA is less common but just as effective for chest pain. The thoracic spine’s unique shape, with ribs attached, makes it tricky. Getting the needle in the right spot is vital.
- It’s used for thoracic facet syndrome.
- Knowing the thoracic spine’s layout is essential.
- Though rare, possible side effects must be thought about.
Lumbar Medial Branch RFA Techniques
Lumbar medial branch RFA treats chronic lower back pain from facet joints. It creates heat lesions on the nerves that control the painful joints. Choosing the right patients is key to success.
Experts say, “Lumbar medial branch RFA is a lasting fix for those with chronic back pain who’ve tried other treatments.” Its success depends on accurate tests before the treatment.
Key Fact #4: The Procedure Experience Step by Step
Understanding the medial branch ablation procedure is key for those considering it. This treatment aims to relieve chronic back pain. It involves several steps that patients should know about.
Pre-Procedure Preparation
Before the procedure, patients go through a preparation phase. This includes a detailed medical check to see if they’re a good fit. They should tell their doctor about any medications, allergies, or medical conditions. It’s also wise to have someone drive them home, as they might be under local anesthesia.
During the Ablation: What to Expect
During the procedure, patients lie on their stomach or back, depending on the area being treated. The skin is cleaned, and a local anesthetic is used to numb the area. A special needle electrode is then placed near the nerve. Radiofrequency energy heats the nerve, creating a lesion that blocks pain signals.
Immediate Post-Procedure Care
After the procedure, patients are watched for any immediate issues. They might feel discomfort or pain at the needle site, which can be managed with over-the-counter pain meds. Most patients are sent home the same day, advised to rest and avoid hard activities for a bit. Follow-up visits are set to check how the treatment is working and to address any concerns.
Key Fact #5: Duration and Extent of Pain Relief
Knowing how long pain relief lasts is key for those thinking about medial branch ablation. This method can greatly reduce pain for many, but how long and how much relief varies.
Typical Timeline for Pain Reduction
Research shows that pain relief starts a few weeks after the procedure. It can take up to 6-8 weeks to see the full effect. Studies say pain relief can last from 9 to 12 months, with some feeling relief for 2 years or more.
A study in the Journal of Pain Research found that at 12 months, many patients had a lot of pain relief. A researcher said, “Our study shows that medial branch ablation is effective for long-term pain relief in chronic facet joint pain.”
Factors Affecting Treatment Success
Several things can affect how well medial branch ablation works. These include:
- The accuracy of the initial diagnosis
- The precision of the ablation procedure
- Patient selection criteria
- The presence of other spinal conditions
It’s important to carefully evaluate patients to predict treatment success. A pain management expert said, “Choosing the right patients is key to the best results with medial branch ablation.”
| Factor | Impact on Treatment Success |
| Accurate Diagnosis | High |
| Procedure Precision | High |
| Patient Selection | High |
| Presence of Other Spinal Conditions | Moderate |
Long-term Outcomes and Repeat Procedures
Medial branch ablation can greatly reduce pain, but it’s not permanent for everyone. The nerves targeted can grow back, causing pain again. But more procedures can be done to achieve pain relief.
A study on long-term results found that repeat procedures can keep pain relief going. The researchers said, “Repeat RFA procedures can be a good option for those whose pain comes back after initial success.”
In summary, medial branch ablation is a promising option for chronic back pain. Understanding what affects pain relief duration and extent helps patients make better choices about their treatment.
Key Fact #6: Safety Profile and Possible Complications
It’s important to look at the safety and possible problems of medial branch ablation. This is key for making smart choices about managing back pain. While it’s usually safe, like any medical treatment, it can have risks and side effects.
Common Side Effects After Spinal Ablation
Most people who get medial branch ablation have some side effects. But these are usually mild and don’t last long. Common side effects include:
- Temporary discomfort or pain at the procedure site
- Slight swelling or bruising
- Numbness or altered sensation in the treated area
These side effects usually go away in a few days to a week after the procedure.
Rare but Serious Complications
Even though they’re rare, serious problems can happen with medial branch ablation. These may include:
- Infection at the procedure site
- Nerve damage resulting in persistent numbness or weakness
- Allergic reactions to the materials used in the procedure
Patients need to know about these possible complications. They should talk about them with their healthcare provider.
Risk Minimization Strategies
To lower the risks of medial branch ablation, several steps can be taken:
- Careful patient selection based on thorough diagnostic evaluation
- Use of advanced imaging techniques during the procedure
- Strict adherence to sterile technique to prevent infection
- Proper post-procedure care and follow-up
Here is a summary of the safety profile and possible complications in a tabular format:
| Complication Type | Frequency | Management |
| Temporary discomfort | Common | Conservative management |
| Infection | Rare | Antibiotics, possible drainage |
| Nerve damage | Rare | Physical therapy, possible further intervention |
| Allergic reactions | Rare | Medical treatment, possibly hospitalization |
By knowing the possible complications and using strategies to lower risks, healthcare providers can help patients get the best results from medial branch ablation.
Key Fact #7: Technological Advances in Medial Branch RFA
Technological innovations have changed the game for medial branch RFA. Now, patients get better and longer-lasting pain relief. These new tools make the procedure more precise and reliable for chronic back pain.
Multi-Needle Approaches for Better Coverage
Using multiple needles is a big step forward in medial branch RFA. Doctors can now target a wider area. This means more nerves are covered, leading to better pain relief for patients.
Benefits of multi-needle approaches include:
- Increased precision in targeting medial branch nerves
- Improved coverage of the affected area
- Enhanced pain relief outcomes
Cooled Radiofrequency Technology
Cooled radiofrequency technology is another big leap. It uses cooled electrodes to make bigger, more consistent lesions. This can lead to more effective and lasting pain relief.
“Cooled radiofrequency ablation has shown promise in providing sustained pain relief for patients with chronic back pain.”
The use of cooled radiofrequency technology has been linked to:
- Larger lesion sizes potentially iincreasethe effectiveness of the treatment
- More consistent results, as the cooling mechanism helps to prevent overheating and promotes uniform heating
Emerging Research and Future Directions
New research and technologies are shaping the future of medial branch RFA. Studies are looking into new methods like pulsed radiofrequency and high-voltage radiofrequency to improve results.
As Expert, a leading pain management specialist, says, “The field of medial branch RFA is rapidly evolving. New technologies and techniques are being developed to better patient outcomes.”
Looking ahead, medial branch RFA might see:
- Advancements in imaging technologies to improve needle placement accuracy
- Development of new electrode designs for more efficient energy delivery
- Integration of artificial intelligence to personalize treatment protocols
Comparing Ablation to Other Back Pain Treatments
Medial branch ablation is a standout in treating chronic back pain. It has benefits that traditional methods don’t. Knowing how different treatments compare is key for patients and doctors.
Conservative Management Options
First, doctors often try conservative management for back pain. This includes:
- Physical therapy to improve flexibility and strength
- Exercise programs tailored to the patient’s condition
- Lifestyle modifications such as weight loss and stress reduction
- Chiropractic care and spinal manipulation
Butsome patients’ pain doesn’t go away with these methods. Then, treatments like medial branch ablation might help.
Medication-Based Approaches
Medication is a big part of treating chronic back pain. Common treatments include:
- Over-the-counter pain relievers such as NSAIDs
- Prescription medications like muscle relaxants or stronger painkillers
- Corticosteroid injections to reduce inflammation
Medication can help, but it doesn’t fix the pause. It can also have side effects and lead to addiction. Medial branch ablation, though, goes straight to the pain’s source.
Surgical Alternatives for Spinal Pain
When other treatments don’t work, surgery might be considered. Options include:
- Spinal fusion
- Laminectomy or discectomy
- Artificial disc replacement
Surgery is risky and takes a long time to recover from. Medial branch ablation, being less invasive, offers a quicker recovery. This makes it a good choice for many.
In summary, while many treatments exist for back pain, medial branch ablation is unique. It’s effective, safe, and minimally invasive. Knowing how it stacks up against other options helps patients make better choices.
Ideal Candidates for Medial Branch Nerve Ablation
Finding the right candidates for medial branch nerve ablation is key. This method is for those who haven’t found relief from chronic back pain through other treatments.
Medical Conditions Most Responsive to Treatment
Those with facet joint pain are top picks for this procedure. Facet joint pain is a big cause of chronic back pain. The nerves in the facet joints send pain signals.
Here’s a table showing who might benefit from medial branch nerve ablation:
| Condition | Description | Responsiveness to Treatment |
| Facet Joint Pain | Pain from the facet joints in the spine | High |
| Chronic Back Pain | Long-term pain in the back | Moderate to High |
| Failed Conservative Treatments | Patients who didn’t get better with physical therapy or meds | High |
When Ablation May Not Be Appropriate
Medial branch nerve ablation works for many, but not everyone. It’s not for those with certain health issues or who are pregnant or breastfeeding.
Also, the technology behind it, radiofrequency ablation, needs a careful look at the patient’s health and past medical history.
The Patient Evaluation Process
The evaluation for medial branch nerve ablation is detailed. It includes looking at the patient’s medical history, physical check-up, and tests. This helps figure out if the procedure is right for them.
Diagnostic blocks are a big part of this. They help find out if the facet joints are causing the pain. This is key to knowing who will likely get better from the treatment.
Conclusion: Making an Informed Decision About Medial Branch Ablation
Medial branch ablation is a key treatment for chronic back pain. Knowing the facts about it helps patients decide on their treatment.
This procedure is safe and effective in giving lasting pain relief. It’s a good choice for those who haven’t found help with other treatments.
It works by stopping pain signals to the brain. Radiofrequency ablation, used in this procedure, helps many patients feel less pain.
Before trying medial branch ablation, talk to a healthcare professional. They can help figure out if it’s right for you. This way, you can understand the benefits and risks and make a smart choice.
FAQ
What is medial branch ablation?
Medial branch ablation is a small procedure that uses radiofrequency energy. It aims to stop pain signals from the facet joints to the brain. This helps relieve chronic back pain.
How does radiofrequency ablation work?
It uses heat from radiofrequency energy to damage the nerves. This creates a block in pain signal transmission.
What are diagnostic blocks, and why are they necessary?
Diagnostic blocks are injections to find pain sources. They check if the nerves are causing pain. This step is key to ensuring the right nerves are treated.
Can medial branch ablation be performed on any part of the spine?
Yes, it can be done on the cervical, thoracic, and lumbar spine. Each area has its own method and care.
What can I expect during the medial branch ablation procedure?
You’ll lie on your stomach or side, depending on the area. The doctor will use X-rays to guide needles to the nerves. Then, radiofrequency energy is applied.
How long does pain relief from medial branch ablation last?
Relief can last from 6 to 24 months or more. It varies by person. Repeat treatments may be needed.
What are the possible risks and complications of medial branch ablation?
You might feel temporary discomfort, swelling, or bruising. But serious issues like infection, nerve damage, or allergic reactions are rare.
How does medial branch ablation compare to other back pain treatments?
It’s a non-surgical, minimally invasive option. It offers longer pain relief than some other treatments. It’s often considered before surgery.
Who is a good candidate for medial branch ablation?
It’s for those with chronic back pain from facet joints. They should have tried other treatments and had diagnostic blocks to confirm pain sources.
What is the role of cooled radiofrequency technology in medial branch ablation?
Cooled radiofrequency technology makes the procedure more precise. It allows for larger lesions, which might improve results.
Can medial branch ablation be repeated if pain returns?
Yes, it can be done again if pain comes back. The procedure can be adjusted based on how you respond and change over time.
Reference
- Kwon, B. S., et al. (2014). The effectiveness of endoscopic radiofrequency denervation of medial branch in patients with chronic low back pain originating from facet joints. Asian Spine Journal, 8(5), 567-573. https://pmc.ncbi.nlm.nih.gov/articles/PMC4219193/