
Electromyography (EMG) is a comprehensive diagnostic procedure used to assess the health of muscles and the nerve cells (motor neurons) that control them. While often referred to collectively as “an EMG,” the evaluation typically consists of two distinct but complementary parts: the Nerve Conduction Study (NCS) and the Needle EMG proper. Together, they function as a “bio-electrical audit” of the peripheral nervous system.
The primary purpose of EMG is to pinpoint the source of neuromuscular symptoms such as unexplained weakness, tingling, numbness, or muscle cramping. It solves the diagnostic dilemma of distinguishing between a problem within the brain/spinal cord (central nervous system), a problem with the nerve root (radiculopathy), a malfunction of the peripheral nerve itself (neuropathy), or a disease of the muscle tissue (myopathy). For example, if a patient has a weak hand, an MRI might show a herniated disc in the neck, but it cannot prove if that disc is actually causing the weakness. EMG provides the functional proof, verifying whether the nerve signals are being blocked, slowed, or degraded, and determining the exact location of the injury.
How the EMG Works?
The human neuromuscular system operates on electricity. Nerves transmit signals like electrical wires, and muscles contract in response to these electrical impulses. EMG technology measures the speed and strength of these bio-electrical signals.
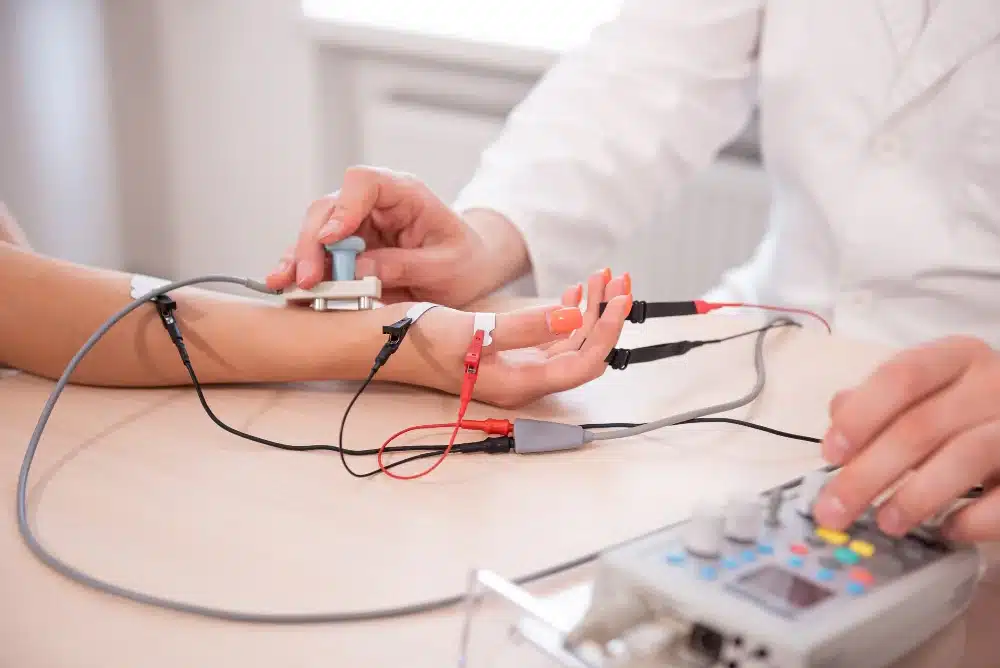
Part 1: Nerve Conduction Study (NCS)
This phase tests the “wires” (nerves) to see how fast and well they carry signals.
- Stimulation: The physician places small recording stickers (surface electrodes) on the skin over a specific muscle or nerve path. A handheld stimulator probe is then placed on the skin at a different point along the nerve.
- Velocity Calculation: The stimulator delivers a mild, brief electrical pulse. This artificial signal travels down the nerve to the recording electrode. The machine calculates the “Conduction Velocity” (speed in meters per second) and the “Amplitude” (strength of the signal). If the myelin sheath (insulation) around the nerve is damaged, the signal travels slowly. If the inner nerve fiber (axon) is damaged, the signal strength is reduced.
Part 2: Needle Electromyography (Needle EMG)
This phase tests the “engine” (muscle) to see how it responds to the ignition signal.
- Insertion: A very fine, sterile needle electrode is inserted directly into the belly of the muscle. This needle acts as a microphone; it does not inject medication or deliver shocks.
- Resting Activity: First, the muscle is tested at complete rest. Healthy muscle is electrically silent when resting. Spontaneous electrical bursts (fibrillations) while the muscle is relaxed indicate nerve damage or irritation.
- Motor Unit Recruitment: The patient is then asked to gently contract the muscle (e.g., “bend your elbow slightly”). The needle records the electrical discharge of individual motor units.
- Audio-Visual Translation: The EMG machine converts these electrical signals into both visual waves on a screen and audible sounds. A healthy muscle contraction sounds like a smooth, rhythmic thumping. A diseased muscle or a nerve-damaged muscle produces distinct, chaotic sounds often described as “rain on a tin roof” or a “hailstorm.”
Clinical Advantages and Patient Benefits
EMG provides objective, quantifiable data that imaging scans cannot offer, leading to more precise treatment plans and avoiding unnecessary surgeries.
Functional Verification
MRI and CT scans are structural; they show anatomy. EMG is functional; it shows physiology. An MRI might show a “pinched nerve” that looks severe but is actually old and inactive. Conversely, it might miss a subtle nerve compression that is causing significant pain. EMG verifies if the structural abnormality seen on a scan is actually the cause of the patient’s symptoms. This prevents patients from undergoing spine surgery for a disc herniation when their pain is actually caused by a peripheral nerve trap like Carpal Tunnel Syndrome.
Precise Localization
EMG can localize a nerve injury with centimeter-level precision. In cases of traumatic nerve injury or compression, knowing exactly where the signal stops allows surgeons to plan the incision precisely, minimizing tissue disruption and reducing recovery time.
Severity Grading and Prognosis
Beyond diagnosis, EMG grades the severity of the condition (mild, moderate, or severe). This is critical for predicting recovery.
- Recovery Timeline: It can differentiate between neuropraxia (a temporary conduction block that recovers in weeks) and axonotmesis (physical damage to the nerve fiber that takes months to heal). This allows physicians to give patients realistic expectations about their recovery timeline.
Targeted Medical Fields and Applications
EMG is utilized primarily by neurologists and physiatrists (PM&R specialists), but its findings dictate treatment across orthopedics, neurosurgery, and rheumatology.
Neurology
- Amyotrophic Lateral Sclerosis (ALS): EMG is the definitive test for diagnosing Motor Neuron Disease. It detects widespread denervation (loss of nerve connection) in muscles that may still appear strong, allowing for early diagnosis.
- Myasthenia Gravis: Specialized “Single Fiber EMG” or “Repetitive Nerve Stimulation” tests detect the breakdown in communication between the nerve and the muscle, confirming this autoimmune disorder.
Orthopedics and Spine Surgery
- Radiculopathy (Sciatica/Pinched Nerve): It differentiates between back pain caused by muscle strain vs. back pain caused by nerve root compression. It confirms which specific spinal level (e.g., L5 vs. S1) is involved, guiding the surgeon to the correct disc.
- Peripheral Nerve Entrapment: It is the gold standard for diagnosing Carpal Tunnel Syndrome (wrist), Cubital Tunnel Syndrome (elbow), and Tarsal Tunnel Syndrome (ankle).
Rheumatology
- Myopathy and Myositis: In conditions like Polymyositis, the muscle tissue itself is inflamed. EMG shows a distinct “myopathic pattern” (short, small, abundant spikes), helping distinguish inflammatory muscle disease from nerve disease.
Patients EEG Experiences
An EMG study typically lasts between 30 to 60 minutes. It is an interactive procedure, requiring patient cooperation.
Preparation
Patients are advised to arrive with clean skin, free of lotions, oils, or creams, as these can interfere with the electrical sensors. Loose-fitting clothing allows easy access to the arms and legs. There is no need for sedation; the patient must be awake to follow commands like “push against my hand.”
Experience During NCS (The Shocks)
During the nerve conduction study, patients feel a sensation often described as a static shock or a strong vibration.
- Sensation: It is startling but generally not painful. The pulse lasts only a fraction of a millisecond. The muscle may twitch involuntarily, which is normal.
- Repetition: Several nerves in the arms or legs will be tested, requiring multiple pulses.
Experience During Needle EMG (The Stick)
- The Needle: The needle used is solid and incredibly thin (similar to an acupuncture needle), much finer than a hypodermic needle used for drawing blood.
- Discomfort: There is a small pinch when the needle penetrates the skin. Once in the muscle, the sensation is usually described as pressure or a dull ache. It is not excruciating.
- Activity: The physician may move the needle slightly to record from different depths of the muscle. This can cause brief discomfort. The patient hears the static sounds of their own muscles on the machine’s speaker, which helps them understand what the doctor is testing.
After the Procedure
There is no recovery time. Patients can drive themselves home immediately. Some minor bruising or soreness at the needle insertion sites is common but typically resolves within a day or two.
Safety and Precision Standards
EMG is a safe, low-risk procedure, but strict technical protocols ensure the data is reliable and the patient is protected.
Sterility and Single-Use Needles
Modern EMG strictly utilizes single-use, disposable needle electrodes. A new, sterile needle is opened for every patient and disposed of immediately after the test. This completely eliminates the risk of transmitting blood-borne infections like Hepatitis or HIV.
Anticoagulation Management
Safety protocols require a review of the patient’s medications. While EMG is safe for most patients on blood thinners (like aspirin or warfarin), the physician must be informed to apply extra pressure after needle removal to prevent hematoma (bruising). In rare cases of therapeutic-level anticoagulation, deeply located muscles may be avoided to prevent internal bleeding.
Temperature Control
Precision in EMG is highly dependent on limb temperature. Cold limbs conduct nerve signals slower, which can mimic disease.
- Warming Protocol: Standards of care dictate that the patient’s skin temperature must be measured before the test. If the arm or leg is cold (below 32°C), it must be warmed with heating pads or warm water immersion. This standardization prevents false-positive diagnoses of nerve entrapment.
Electrical Safety
The equipment is electrically isolated. The current used in nerve conduction studies is very low amperage and is strictly direct current (DC), making it safe for the heart. However, special precautions are taken for patients with implanted cardiac defibrillators (ICD) or pacemakers. The electrical pulses are kept away from the device and the ground electrode is positioned to ensure the current does not cross the chest.






