Learn the 5 alarming melanoma in mouth symptoms. This guide covers the critical early signs of this rare but dangerous oral cancer. Finding malignant melanoma in the mouth and tongue early is key. This rare and aggressive cancer can be very serious. But catching it early can greatly improve treatment chances.
In the U.S. and Europe, oral malignant melanoma is less than 1% of all melanomas. It mostly hits people over 40. Knowing the warning signs is very important.
We will look at the important signs of melanoma mouth cancer. We will also talk about new ways to treat it. By knowing the risks and spotting symptoms early, we can help improve treatment results.
Key Takeaways
- Early detection of oral malignant melanoma is critical for improved prognosis.
- This rare cancer predominantly affects individuals over 40 years old.
- Males are more likely to be diagnosed with oral malignant melanoma.
- Recognizing the warning signs is essential for effective treatment.
- Advanced multidisciplinary treatment approaches can improve outcomes.
Understanding Oral Melanoma

It’s important to know about oral melanoma for early detection and treatment. Oral melanoma, also known as melanoma of the mouth or gum melanoma, is a rare but aggressive cancer in the mouth.
What Is Oral Melanoma?
Oral melanoma is a malignant melanoma in the mouth’s mucous membranes. It can happen on the gums, palate, and tongue. It’s different from skin melanoma.
Prevalence and Demographics
Oral melanoma is more common in some groups. In Japan, it’s found in 11% to 12.4% of people. It usually starts when people are around 56 years old, but it can happen at any age. Older adults are more likely to get oral cancer, including melanoma.
Things like smoking, drinking a lot of alcohol, and HPV infection increase the risk of oral cancer.
Why Early Detection Matters
Finding oral melanoma early is key to better treatment. Early detection can mean less surgery and better survival chances. Regular self-checks and doctor visits are important for catching it early.
Demographic Factor | Prevalence/Characteristic |
Average Age at Diagnosis | 56 years |
Prevalence in Japan | 11-12.4% |
Common Risk Factors | Tobacco use, heavy alcohol consumption, HPV infection |
Knowing about oral melanoma helps us spot and manage it better. This knowledge is key to early detection and treatment.
Common Sites of Oral Cancer Melanoma

Knowing where oral melanoma often starts is key for catching it early. It can pop up in different spots in the mouth. Spotting these common areas early can help a lot.
Hard Palate (Most Common at 34.29%)
The hard palate is hit the most, making up about 34.29% of cases. This shows why checking this area often is so important.
Buccal Gingiva
The area next to the cheeks, called the buccal gingiva, is also a hotspot. Malignant melanoma on gums can be very aggressive. So, it’s vital to keep an eye on it.
Tongue
The tongue is another key spot for oral melanoma. It’s easy to see and can be caught early. But, melanoma here can spread fast.
Other Oral Mucosal Surfaces
Oral melanoma can also show up on other mouth surfaces. This includes the lips, floor of the mouth, and the alveolar ridge. Knowing about these spots is important for a full check-up.
Common Sites | Frequency | Clinical Significance |
Hard Palate | 34.29% | Most common site, high incidence |
Buccal Gingiva | Variable | Significant due to high risk of cancer |
Tongue | Common | Easy to spot, good chance for early catch |
Other Mucosal Surfaces | Less common | Important for full check-up |
Risk Factors for Developing Oral Melanoma
Oral melanoma is caused by genetics, environment, and demographics. Knowing these factors helps us spot who’s at risk. This knowledge can help prevent the disease.
Age and Gender Considerations
Oral melanoma can happen at any age, but most people are diagnosed at 56. Men are more likely to get it than women, with a 2:1 ratio. This shows men face a higher risk.
Genetic Predispositions
Genetics play a big role in oral melanoma. If your family has a history of melanoma or other cancers, you might be at higher risk. Some genetic mutations can also increase your risk.
Environmental Influences
Things like smoking and drinking can raise your risk of oral melanoma. Viruses like HPV can also play a part in oral cancer.
Pre-existing Oral Conditions
Having certain oral conditions can also increase your risk. Regular dental visits are key to managing these conditions.
To summarize the risk factors, we can look at the following table:
Risk Factor | Description | Impact |
Age | Average age at diagnosis is 56 years | Higher risk with increasing age |
Gender | Male-to-female ratio is 2:1 | Males are at higher risk |
Genetic Predispositions | Family history of melanoma or other cancers | Increased risk with genetic mutations |
Environmental Influences | Tobacco use, alcohol consumption, HPV infection | Significant increase in risk |
Understanding these risk factors helps us identify who’s at risk. This can lead to better outcomes through early detection and prevention.
Early Warning Signs of Oral Melanoma
It’s key to spot the early signs of oral melanoma to get help fast. Oral melanoma can show up in many ways. So, it’s important to watch for any changes in your mouth.
Unusual Pigmentation Changes
One big sign is unusual pigmentation changes. You might see new or changing spots in your mouth. These spots can be brown, black, or even not show color at all. Melanoma in the mouth often looks like this.
Unexplained Oral Pain or Discomfort
Feeling pain or discomfort in your mouth without a reason is another sign. This pain can keep coming back and not have a clear cause. It’s important to check any ongoing pain, as oral cancer melanoma can cause it.
Bleeding, Swelling, or Ulceration
Bleeding, swelling, or ulcers in your mouth without a clear cause might mean oral melanoma. These signs happen as the tumor grows and might ulcerate. Checking your mouth regularly can help catch it early.
Changes in Sensation or Function
Feeling numb or noticing changes in how you can use your mouth are also signs. As the melanoma grows, it can harm nerves and tissues. Being mindful of these changes is key to catching it early.
Spotting these signs early is very important for your health. We stress the need to know these signs and see a doctor if you notice anything odd.
How to Perform Oral Self-Examinations
Oral self-examinations are a simple way to spot issues like oral melanoma. By checking your mouth regularly, you can find early signs. This can lead to better treatment results. We’ll show you how to do these exams right.
Step-by-Step Examination Process
To do an oral self-examination, follow these steps:
- Start by standing in front of a mirror with good lighting.
- Remove any dentures or oral appliances.
- Examine your lips for any unusual pigmentation or lesions.
- Open your mouth wide and look at the roof of your mouth, checking for any abnormalities.
- Pull your cheeks out to inspect the inner lining and the buccal mucosa.
- Examine your tongue, including the top, bottom, and sides.
- Check the floor of your mouth and the gingiva (gums).
What to Look For
Look for these things during your self-examination:
- Unusual pigmentation or color changes.
- Lesions, sores, or ulcers that do not heal.
- Swelling or thickening of the oral mucosa.
- Bleeding or pain in the mouth without an apparent cause.
- Changes in the sensation or function of your mouth.
If you see any of these signs, get a healthcare professional’s opinion right away.
When to Seek Professional Help
If you find any unusual changes or symptoms, get help fast. Catching malignant melanoma oral early is key. A dentist or doctor can do a detailed check and suggest the right steps.
Tools and Lighting Recommendations
For an effective oral self-examination, you’ll need:
- A good quality mirror that allows you to see clearly.
- Adequate lighting, preferably natural light or a bright LED light.
- A clean and comfortable environment to conduct the examination.
By following these tips and staying alert to your oral health, you can help find melanoma of the mouth early. Regular self-checks and visits to the dentist can greatly improve your oral health and overall well-being.
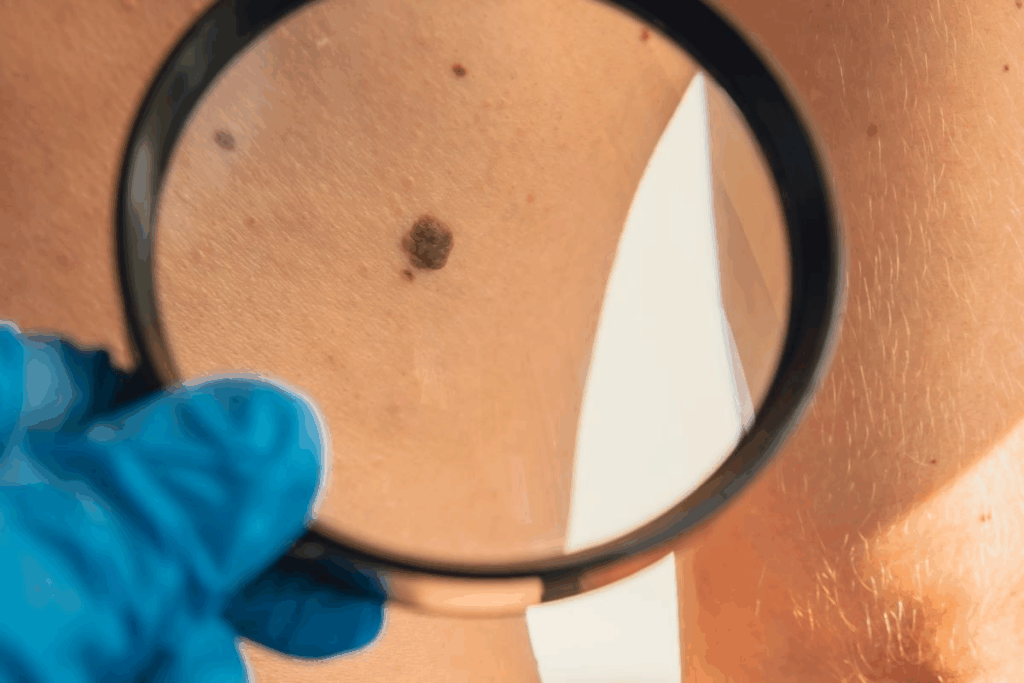
Professional Screening and Diagnosis
Early detection of oral melanoma is key. Accurate diagnosis is vital for effective treatment. We’ll guide you through the screening and diagnosis process.
What to Expect During a Professional Examination
Your healthcare provider will examine your mouth thoroughly. They’ll check your lips, tongue, gums, and more. They look for unusual pigmentation, ulcers, or other signs of melanoma mouth cancer.
They might use special tools and lighting to see better. They’ll also feel the area for swelling or tenderness. This can help spot malignant melanoma gums.
Biopsy Procedures
If they find something suspicious, a biopsy might be needed. A biopsy removes a small tissue sample for microscopic examination.
There are different biopsy types:
- Incisional biopsy: Takes a part of the lesion.
- Excisional biopsy: Removes the whole lesion.
Advanced Imaging Techniques
Advanced imaging can also help diagnose and stage oral melanoma. Techniques include:
- X-rays
- CT scans
- MRI scans
- PET scans
These tests check if the cancer has spread. This is important for treatment planning.
Staging of Oral Melanoma
After diagnosis, the cancer’s stage is determined. Staging looks at the tumor size, lymph node involvement, and distant spread.
Stage | Description |
I | The cancer is localized and relatively small. |
II | The cancer is larger or has spread to nearby tissues. |
III | The cancer has spread to nearby lymph nodes. |
IV | The cancer has metastasized to distant parts of the body. |
Knowing the stage is key for treatment planning and prognosis.
Differentiating Oral Cancer Melanoma from Benign Conditions
Oral melanoma can look like harmless pigmentation in the mouth. It’s important to know how to tell them apart. This is key for the right diagnosis and treatment.
Common Benign Oral Pigmentations
Many harmless pigments can show up in the mouth. These include:
- Oral melanotic macule: A benign pigmented lesion that can appear as a brown or black spot.
- Amalgam tattoo: A harmless pigmentation caused by the deposition of amalgam particles in the oral mucosa.
- Oral nevus: A benign growth that can be pigmented.
These conditions are usually not harmful but can look like melanoma. Knowing what they look like is important for making the right diagnosis.
Key Distinguishing Features
To tell oral melanoma from harmless conditions, look for certain signs. The main things to check are:
Characteristics | Benign Conditions | Oral Melanoma |
Color | Uniformly brown or black | Variable color, including shades of brown, black, and sometimes red or white |
Border | Well-defined borders | Irregular, notched, or scalloped borders |
Size | Typically small and stable | Can grow in size over time |
Surface | Usually smooth | May be ulcerated or have an irregular surface |
When to Be Concerned
If you see any changes in your mouth, get help right away. Look out for:
- A new or changing pigmented lesion in the oral cavity.
- A lesion that is growing in size or changing in color.
- A lesion with irregular borders or an irregular surface.
Early detection is key for good treatment. If you’re unsure about any mouth pigmentation, see a doctor for a check-up.
Treatment Options for Early-Stage Oral Melanoma
Managing early-stage oral melanoma involves a mix of treatments. We’ll look at treatment options like surgery, radiation, and immunotherapy.
Surgical Interventions
Surgery is key for early-stage oral melanoma. The goal is to remove the tumor and some healthy tissue around it. This helps reduce the chance of the cancer coming back.
The surgery needed depends on the melanoma’s size and where it is. For example, melanoma tongue cancer treatment might include removing part of the tongue. This ensures the cancer is fully removed.
Radiation Therapy Approaches
Radiation therapy is also important for treating oral melanoma. It’s used when the cancer is in a sensitive area or when surgery margins are close. We use advanced techniques to target the tumor well, protecting nearby tissues.
External beam radiation therapy and brachytherapy are used based on the tumor’s details and location.
Immunotherapy Options
Immunotherapy is a new hope for treating malignant melanoma, including oral melanoma. It boosts the body’s immune system to fight cancer cells better. Checkpoint inhibitors are a type of immunotherapy drug that has shown great promise in treating advanced melanoma.
Treatment Selection Factors
Choosing the right treatment for oral cancer melanoma treatment involves several factors. These include the cancer’s stage, the patient’s health, and the tumor’s characteristics. We use these to create a treatment plan that fits each patient.
Treatment Modality | Indications | Benefits |
Surgery | Early-stage melanoma, localized tumors | Potential for cure, removal of tumor |
Radiation Therapy | Tumors in sensitive areas, close surgical margins | Precise targeting, minimal damage to surrounding tissues |
Immunotherapy | Advanced melanoma, recurrent disease | Enhanced immune response, targeted therapy |
Knowing the different treatment options helps patients with early-stage oral melanoma make informed choices. We’re dedicated to supporting patients through every step of their treatment.
Advanced Treatment Strategies
When oral melanoma gets worse, we need new ways to treat it. This section will look at how we tackle advanced oral melanoma. We’ll cover combination therapies, clinical trials, and palliative care.
Combination Therapies
For advanced oral melanoma, combining treatments is a promising approach. We mix treatments like surgery, radiation, and immunotherapy. This way, we can attack the cancer more effectively.
Benefits of Combination Therapies:
- Enhanced tumor control
- Improved survival rates
- Reduced risk of recurrence
We’ll dive into the details of these therapies. We’ll see how they’re customized for each patient.
Clinical Trials and Emerging Treatments
Clinical trials are key in finding new treatments for oral melanoma. They test new therapies that might not be available yet. This gives patients access to the latest treatments.
Trial Type | Description | Potential Benefits |
Immunotherapy Trials | Investigating new immunotherapies to boost the body’s immune response against cancer cells | Improved response rates, enhanced survival |
Targeted Therapy Trials | Examining targeted therapies that focus on specific genetic mutations in cancer cells | More precise treatment, reduced side effects |
Palliative Care Considerations
Palliative care is vital for advanced oral melanoma. It focuses on easing symptoms, pain, and stress of the disease.
Palliative care teams work closely with patients and their families. They address unique needs to improve quality of life.
Multidisciplinary Treatment Teams
Advanced oral melanoma treatment benefits from a team effort. Specialists like oncologists, surgeons, and radiologists work together. They also include palliative care professionals.
We create a treatment plan that fits each patient’s needs and situation.
Post-Treatment Care and Follow-Up
After treatment for oral melanoma, it’s important to watch for signs of the disease coming back. It’s also key to manage any side effects. A follow-up plan helps keep an eye on your health and catch any problems early.
Monitoring for Recurrence
Seeing your healthcare provider regularly is vital. They will check the treated area for any signs of cancer coming back. This may include exams, tests, and biopsies if needed.
- Schedule regular follow-ups as recommended by your healthcare team.
- Be aware of the signs of recurrence, such as new pigmentation or ulcers.
- Report any changes or concerns to your healthcare provider promptly.
Managing Side Effects
Handling side effects well is important for a better life after treatment. This can include managing pain, getting the right nutrition, and doing rehabilitation.
Common side effects that may need to be managed include:
- Dry mouth (xerostomia)
- Difficulty swallowing (dysphagia)
- Changes in taste or sensation
- Fatigue
Long-term Surveillance Protocols
Keeping an eye on your health long-term is key. This means regular check-ups with your healthcare team, even after five years.
“Long-term follow-up is critical for those treated for oral melanoma. It helps catch any return of the disease early and manage late effects.” — Expert in Oral Oncology
Nutritional and Oral Care Considerations
Good oral hygiene and a balanced diet are important after treatment. Your healthcare team can guide you on how to take care of your mouth and eat well despite any challenges.
- Avoiding irritants such as spicy or acidic foods.
- Ensuring adequate hydration.
- Consuming a balanced diet rich in fruits, vegetables, and proteins.
By following these tips, you can improve your life and lower the risk of problems after treatment for gum melanoma or oral melanoma.
Prognosis and Survival Rates
Oral melanoma is a rare but aggressive cancer. Its prognosis is greatly improved by early detection. The 5-year survival rate for oral malignant melanoma is about 15-40%. Knowing what affects prognosis and survival is key for patients and doctors.
Factors Affecting Prognosis
Several factors greatly influence oral melanoma prognosis. These include the cancer’s stage, tumor thickness, and if it has spread. Early diagnosis leads to a better prognosis than later stages.
- Stage at Diagnosis: Early detection means better survival chances.
- Tumor Thickness: Thicker tumors have a worse prognosis.
- Metastasis: If the cancer has spread, the prognosis is much worse.
Comparison with Cutaneous Melanoma
Oral melanoma has a different prognosis than cutaneous melanoma. Cutaneous melanoma, caught early, has a higher survival rate. This is because cutaneous melanoma is easier to spot on the skin.
Impact of Early Detection on Survival
Early detection of oral melanoma is vital for better survival chances. Early-stage diagnosis means more effective treatments and higher survival rates. Regular self-exams and dental check-ups are essential to catch any unusual changes.
The 5-year survival rate varies with the cancer’s stage. Localized oral melanoma has a better survival rate than cancer that has spread.
Quality of Life Considerations
Prognosis isn’t just about survival; it’s also about quality of life. Oral melanoma patients face challenges like eating, speaking, and swallowing difficulties. Managing these symptoms is key to a good quality of life.
We help patients create a care plan that treats the cancer and improves daily life. This plan addresses both treatment and symptom management.
Conclusion
Early detection and treatment are key to beating oral melanoma, a rare but aggressive cancer. We’ve covered the main points about oral melanoma, like how common it is, its risk factors, early signs, and treatment choices.
Being aware and catching it early is vital in fighting oral melanoma. Knowing where oral cancer often starts and the risk factors helps people watch their mouth health. Regular self-checks and doctor visits are important to spot oral melanoma early.
Diagnosing and treating oral melanoma needs a team effort. This includes surgery, radiation, and immunotherapy. We’ve highlighted the importance of quick action and proper care to boost survival chances and quality of life for mouth cancer patients.
We urge everyone to stay alert about their mouth health and get help if they see anything odd. With the right steps, we can all help improve outcomes for those with oral melanoma.
FAQ
What is oral melanoma, and how common is it?
Oral melanoma is a rare and aggressive cancer in the mouth. It makes up less than 1% of all melanomas in the U.S. and Europe.
What are the common sites where oral melanoma occurs?
The hard palate is most often affected. Other areas like the buccal gingiva and tongue are also common.
What are the risk factors for developing oral melanoma?
Risk factors include age over 40, being male, genetic predispositions, and environmental influences. Pre-existing oral conditions also play a role.
What are the early warning signs of oral melanoma?
Look out for unusual pigmentation, pain, bleeding, swelling, or ulceration. Also, watch for changes in sensation or function.
How can I perform an oral self-examination to detect oral melanoma early?
Check your mouth step by step for unusual changes. If you find anything suspicious, get professional help right away.
What can I expect during a professional screening and diagnosis for oral melanoma?
A healthcare professional will look for signs of oral melanoma. They might do a biopsy to confirm. Advanced imaging can help stage the cancer.
How is oral melanoma differentiated from benign oral conditions?
Look for unusual pigmentation changes or irregular borders. These are key signs that can help tell it apart from benign conditions.
What are the treatment options for early-stage oral melanoma?
Early-stage oral melanoma can be treated with surgery, radiation, or immunotherapy. The choice depends on several factors.
What are the advanced treatment strategies for oral melanoma?
Advanced treatments include combination therapies and clinical trials. Palliative care is also important to manage symptoms and improve quality of life.
Why is post-treatment care and follow-up important for oral melanoma?
Post-treatment care and follow-up are key. They help monitor for recurrence, manage side effects, and ensure long-term surveillance.
What is the prognosis and survival rate for oral melanoma?
The prognosis and survival rate vary based on several factors. Early detection significantly improves survival chances.
How does oral malignant melanoma differ from cutaneous melanoma?
Oral malignant melanoma is more aggressive and has a poorer prognosis than cutaneous melanoma. It affects different areas and has different demographics.
What is the role of palliative care in managing oral melanoma?
Palliative care is vital for managing symptoms and improving quality of life. It’s essential for patients with advanced oral melanoma.
Can melanoma occur on the gums?
Yes, melanoma can occur on the gums. It’s important to know the signs and symptoms to detect it early.
What is the impact of early detection on the survival rate of oral melanoma?
Early detection greatly improves survival rates for oral melanoma. Regular self-examinations and professional screenings are key.


