Diabetic retinopathy is a serious problem linked to diabetes. It damages the blood vessels in the retina. This can lead to vision loss if not treated right away.mild diabetic retinopathyOPTHALMOLOGY
Diabetic retinopathy goes through different stages, from mild nonproliferative to severe proliferative. Knowing these stages helps patients and doctors take the right steps.
We will look at the five stages of this condition. We’ll see why catching it early and treating it right is key to saving your sight.
Key Takeaways
- Diabetic retinopathy is a complication of diabetes affecting the retina.
- It progresses through distinct stages, from mild to severe forms.
- Understanding these stages is key for timely actions.
- Early detection and proper treatment can stop vision loss.
- Knowing the stages helps both patients and doctors.
What Is Diabetic Retinopathy and Who Is at Risk

Diabetic retinopathy is a common eye problem linked to diabetes. It can seriously harm your vision if not treated. It happens when the blood vessels in the retina, the back of the eye, get damaged.
The Microvascular Damage Process
Diabetic retinopathy is caused by damage to the tiny blood vessels in the retina. High blood sugar levels can harm these vessels. This leads to microaneurysms, hemorrhages, and exudates.
This damage can make your vision worse. If it gets really bad, it can cause blindness.
The process involves several key steps:
- High blood sugar levels damage the small blood vessels in the retina.
- The damaged vessels leak fluid or blood, causing swelling and vision problems.
- In advanced stages, new, fragile blood vessels may form, leading to further complications.
Prevalence and Risk Factors
Anyone with diabetes can get diabetic retinopathy. The risk goes up if you have diabetes for a long time and don’t control your blood sugar well. Other things that increase your risk include high blood pressure, high cholesterol, pregnancy, and tobacco use.
Studies show that nonproliferative diabetic retinopathy is found in:
- 25% of patients five years after diabetes diagnosis
- 60% at 10 years
- 80% at 15 years
This shows why regular eye exams and good diabetes care are so important.
Knowing about these risks and how common diabetic retinopathy is can help catch it early. This can save your vision.
How Diabetes Affects Your Eye Health

It’s important to know how diabetes affects the eyes to manage diabetic retinopathy. Diabetes damages the tiny blood vessels that feed the retina, leading to vision issues. High blood sugar can make these vessels leak or block, harming the retina’s function.
Blood Vessel Damage Mechanisms
Diabetic retinopathy damages blood vessels in several ways. High blood sugar levels make blood vessels weak and leaky, causing hemorrhages. The body tries to fix these vessels but creates new, fragile ones that can bleed easily.
Inflammation and oxidative stress also play big roles in diabetic retinopathy. These factors harm the retina, leading to severe vision loss if not treated.
Timeline of Retinopathy Development
Diabetic retinopathy develops over time, with several stages. Knowing this timeline helps catch and treat it early.
The first stage, mild nonproliferative diabetic retinopathy, shows as microaneurysms in the retina. As it gets worse, the risk of losing vision grows.
Spotting diabetic retinopathy early can prevent serious vision loss. Regular eye exams are key for people with diabetes to keep an eye on their retina’s health.
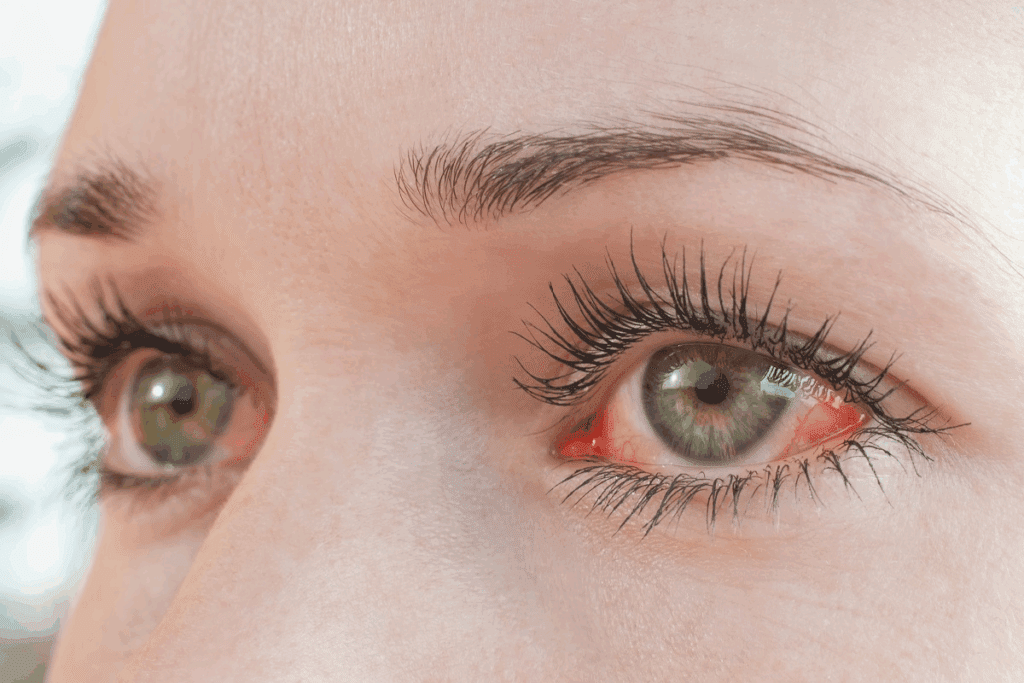
Mild Diabetic Retinopathy: The First Warning Signs
Diabetic retinopathy’s first stage, mild NPDR, is marked by the formation of microaneurysms in the retina. At this early stage, the disease begins to manifest through subtle changes in the blood vessels of the retina.
Microaneurysm Formation
In the early stages of diabetic retinopathy, the walls of the blood vessels in the retina weaken. This causes tiny bulges called microaneurysms. These microaneurysms can leak fluid and blood into the retina, setting the stage for further complications. The formation of microaneurysms is a critical indicator of mild NPDR, as it signifies the initial damage to the retinal vasculature.
Symptoms and Detection Challenges
Mild NPDR often presents with minimal or no symptoms, making it challenging to detect without a thorough eye examination. Patients may not experience significant vision problems initially, but regular monitoring is essential to prevent progression. We recommend that individuals with diabetes undergo regular eye exams to catch the disease early.
Progression Statistics
While mild NPDR is the earliest stage, there is a risk of progression. Studies have shown that about 16% of cases progress to proliferative diabetic retinopathy within four years if left unchecked. Early detection and management are key to preventing severe complications. By controlling blood sugar levels and undergoing regular eye exams, patients can significantly reduce the risk of progression.
Moderate Nonproliferative Diabetic Retinopathy
Moderate NPDR is a serious step in diabetic retinopathy. It shows more damage to the blood vessels in the retina. This stage is marked by several clear signs.
Increased Microaneurysms and Dot-and-Blot Hemorrhages
In moderate NPDR, you’ll see more microaneurysms and dot-and-blot hemorrhages. Microaneurysms are small bulges in the blood vessels. Dot-and-blot hemorrhages are tiny blood spots in the retina. These signs show the damage diabetes does to the blood vessels.
- Microaneurysms are a key sign of diabetic retinopathy, showing weak blood vessel walls.
- Dot-and-blot hemorrhages happen when these weak vessels burst, causing the retina to not get enough blood.
Cotton-Wool Spots and Hard Exudates
Moderate NPDR also brings cotton-wool spots and hard exudates. Cotton-wool spots are white, fluffy spots on the retina from lack of blood flow. Hard exudates are lipid deposits from leaking blood vessels.
Cotton-wool spots mean the retina’s nerve layer isn’t getting enough blood. Hard exudates show long-term damage from leaking blood vessels. Both are important signs of diabetic retinopathy getting worse.
Vision Changes at This Stage
At this stage, vision changes may start, but they’re often small. The damage to blood vessels can cause:
- Fluctuations in vision
- Mild blurring of vision
- Difficulty with color perception
People with diabetes should get their eyes checked often. This helps catch these vision changes early and stop them from getting worse.
Severe Nonproliferative Diabetic Retinopathy
Severe nonproliferative diabetic retinopathy (NPDR) is a serious stage of diabetic retinopathy. At this level, the retina has suffered a lot of damage from diabetes. The risk of more serious problems also goes up a lot.
The “4-2-1 Rule” for Diagnosis
The “4-2-1 rule” helps doctors diagnose severe NPDR. It looks for specific signs in the retina: 4 quadrants of hemorrhages and microaneurysms, 2 quadrants of venous beading, or 1 quadrant of intraretinal microvascular abnormalities (IRMA). If these signs are found, it means the patient has severe NPDR. This rule is key for doctors to know how serious the disease is.
Vascular Abnormalities and Ischemia
Severe NPDR shows a lot of problems with blood vessels in the retina. There are many hemorrhages, microaneurysms, and venous beading. These issues cause the retina to not get enough blood, leading to ischemia.
Ischemia makes diabetic retinopathy worse, creating a cycle of damage. IRMA, or shunt systems, try to solve this problem but often fail to fix the retina’s function.
Risk of Progression to Proliferative Stage
Severe NPDR is at high risk of turning into proliferative diabetic retinopathy (PDR). PDR means new, weak blood vessels grow in the retina. This can cause serious vision loss if not treated. The chance of moving to PDR is why it’s so important to watch and treat patients closely.
Regular eye checks and sticking to treatment plans are key. They help stop diabetic retinopathy from getting worse. This way, we can keep vision safe for people with diabetes.
Proliferative Diabetic Retinopathy (PDR)
Proliferative diabetic retinopathy is the most severe stage of diabetic retinopathy. It happens when new, fragile blood vessels grow in the retina. This is a serious problem that can cause vision loss if not treated.
Neovascularization Process
In PDR, the retina tries to get more oxygen by growing new blood vessels. This is called neovascularization. These new vessels are weak and can leak or bleed easily.
These vessels can form on the retina or in the vitreous gel. This shows the retina is not getting enough oxygen. This is because of the damaged blood vessels from diabetic retinopathy.
Vitreous Hemorrhage Complications
Vitreous hemorrhage is a serious problem in PDR. It happens when the new blood vessels bleed into the vitreous gel. This can cause sudden vision loss because the blood blocks light from reaching the retina.
Vitreous hemorrhage can be mild or severe. Sometimes, it clears up on its own. But in severe cases, surgery may be needed to fix vision.
Retinal Detachment Risks
Another big risk with PDR is retinal detachment. The new blood vessels can cause scar tissue. This can pull the retina away from the underlying tissue, leading to detachment.
Retinal detachment is a medical emergency. It needs quick attention to avoid permanent vision loss. Symptoms include sudden flashes of light, floaters, and a shadow or curtain over the vision.
Diabetic Macular Edema: The Fifth Stage
Diabetic macular edema is a serious part of diabetic retinopathy. It happens when fluid builds up in the macula because of leaky blood vessels. This swelling can make vision blurry.
How DME Affects Central Vision
DME mainly messes with central vision. It does this by building up fluid in the macula. The macula is key for clear, central vision. This buildup can cause distorted vision.
This can make it hard to do things that need sharp vision, like reading or driving. How much vision is affected can vary. Some people might only notice small changes, while others could see a big difference.
Occurrence Across Different Retinopathy Stages
DME can happen at any stage of diabetic retinopathy. It can show up even when the retinopathy is mild. This makes it important to keep an eye on it closely.
- DME can be present even in the early stages of diabetic retinopathy.
- The risk of DME increases with the duration of diabetes and the severity of retinopathy.
- Effective management of diabetes is critical in preventing DME.
Vision Impact and Symptoms
The symptoms of DME include blurred vision, double vision, and vision that changes a lot. Sometimes, people don’t notice these symptoms until the problem gets worse.
Getting regular eye exams is key to catching DME early. Early treatment can really help. Options like anti-VEGF injections and laser therapy can help reduce fluid and improve vision.
Diagnosis and Screening Recommendations
Diabetic retinopathy diagnosis uses clinical exams and advanced imaging. Regular eye exams are key for early detection and management.
Components of a Comprehensive Eye Examination
A thorough eye exam for diabetic retinopathy includes a detailed medical history and visual acuity tests. A dilated fundus examination is essential. It lets doctors see the retina for signs of diabetic retinopathy.
The exam might also include fundus photography. This helps track the disease’s progress and treatment success.
Advanced Imaging Techniques
Advanced imaging is critical for diagnosing and managing diabetic retinopathy. Optical Coherence Tomography (OCT) checks retinal thickness and spots diabetic macular edema. OCT angiography shows the retinal vasculature, helping spot non-perfusion and neovascularization.
Recommended Screening Schedules by Risk Level
People with diabetes should get regular eye exams based on their risk level. Those with mild diabetic retinopathy need annual checks. Those with moderate to severe diabetic retinopathy should see doctors every 6-12 months.
Screening schedules can change based on other risk factors like poor glycemic control, hypertension, and hyperlipidemia. Pregnant women with diabetes might need more frequent eye exams due to faster disease progression.
Treatment Options for Each Stage
Managing diabetic retinopathy needs a mix of treatments based on the disease’s stage and severity. We’ll look at different strategies, from controlling blood sugar to surgery.
Blood Sugar Control as Foundation
Keeping blood sugar levels in check is key to managing diabetic retinopathy. This basic step helps stop the disease from getting worse. Studies have shown that controlling blood sugar well can lower the risk of diabetic retinopathy.
- Regular monitoring of blood glucose levels
- Adherence to medication regimens
- Lifestyle modifications including diet and exercise
Laser Treatments and Anti-VEGF Therapy
For more serious cases, laser treatments and anti-VEGF therapy are vital. Laser photocoagulation helps by reducing swelling and stopping vision loss. Anti-VEGF injections cut down on blood vessel leakage and growth.
- Laser photocoagulation for non-proliferative diabetic retinopathy
- Anti-VEGF injections for diabetic macular edema
- Combination therapy for better results
Surgical Interventions for Advanced Cases
For severe cases, like proliferative diabetic retinopathy or serious diabetic macular edema, surgery might be needed. Surgical options include removing blood or scar tissue from the eye with a vitrectomy.
- Vitrectomy for vitreous hemorrhage or retinal detachment
- Scleral buckling for retinal detachment repair
Knowing the treatment options for each stage of diabetic retinopathy helps patients and doctors create a good plan.
Conclusion: Preventing Progression Through Early Detection
Early detection and timely treatment are key to stopping vision loss from diabetic retinopathy. Regular eye exams and good diabetes care are vital. They help prevent this condition from getting worse.
Diabetic retinopathy goes through stages, from mild to severe. Knowing these stages helps in managing the condition well. By keeping blood sugar in check and getting regular eye exams, people with diabetes can lower their risk of losing vision.
Preventing and catching diabetic retinopathy early are essential. We suggest that people with diabetes stick to screening schedules. They should also work closely with their healthcare team to manage their diabetes well.
FAQ
What is diabetic retinopathy?
Diabetic retinopathy is a problem that happens to people with diabetes. It affects the blood vessels in the retina. If not treated, it can cause vision loss.
What are the stages of diabetic retinopathy?
Diabetic retinopathy has several stages. These include mild nonproliferative diabetic retinopathy (NPDR), moderate NPDR, severe NPDR, and proliferative diabetic retinopathy (PDR). Diabetic macular edema can happen at any stage.
What is mild nonproliferative diabetic retinopathy?
Mild NPDR is the first stage of diabetic retinopathy. It’s when small blood vessels in the retina start to swell. It’s hard to notice and often has no symptoms.
How does diabetes affect eye health?
Diabetes can harm the blood vessels in the retina. This is because high blood sugar levels damage these tiny vessels over time. This leads to diabetic retinopathy.
What is diabetic macular edema?
Diabetic macular edema is when fluid builds up in the macula. The macula is key for clear vision. This can cause blurry vision and even vision loss.
How is diabetic retinopathy diagnosed?
Doctors use eye exams to find diabetic retinopathy. They check vision, dilate the eyes, and use tools like optical coherence tomography (OCT).
What are the treatment options for diabetic retinopathy?
Treatments include managing blood sugar, laser therapy, and anti-VEGF therapy. Surgery might be needed for more serious cases.
Can diabetic retinopathy be prevented?
You can’t stop diabetic retinopathy from happening. But, you can slow it down. This is by keeping blood sugar in check, getting regular eye exams, and treating problems early.
What is the “4-2-1 rule” in diabetic retinopathy?
The “4-2-1 rule” is a way to spot severe NPDR. It means looking for specific signs in the retina that show a high risk of getting worse.
What is proliferative diabetic retinopathy?
Proliferative diabetic retinopathy is the most serious stage. It’s when new, weak blood vessels grow in the retina. This can cause bleeding and detachment.
How often should individuals with diabetes have their eyes screened?
People with diabetes should get their eyes checked every year. They might need more frequent exams if their doctor says so.
References
National Center for Biotechnology Information. Evidence-Based Medical Guidance. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3091231/



































