Stem Cell Therapy for Diabetes Success Rate: 7 Key Findings You Need to KnowDiabetic retinopathy is a big problem worldwide, affecting millions. It’s important to know its five stages, from mild to severe.moderate diabetic retinopathy
Diabetic retinopathy is a diabetes complication that harms the retina’s blood vessels. Knowing these stages helps catch it early and treat it to save vision.
We at our institution focus on top-notch care for diabetic eye disease. Our goal is to give our patients the best results.
Key Takeaways
- Diabetic retinopathy progresses through five distinct stages.
- Early detection is key to preventing vision loss.
- Understanding the stages is vital for timely medical action.
- Diabetic retinopathy is a major diabetes complication.
- Our institution is dedicated to providing world-class diabetic eye care.
Understanding Diabetic Retinopathy
It’s key for people with diabetes to know about diabetic retinopathy. This condition can cause serious vision loss if not treated. It affects the blood vessels in the retina, leading to vision problems.
What is Diabetic Retinopathy?
Diabetic retinopathy damages the blood vessels in the retina because of diabetes. This can cause vision problems and, in severe cases, blindness. The retina is vital for seeing, as it turns light into signals for the brain.
How Diabetes Affects the Retinal Blood Vessels
Diabetes makes the retinal blood vessels swell, leak, or close. This can cause new, fragile blood vessels to grow. The damage starts mildly and can get worse.
Global Prevalence and Statistics
About 22.3 percent of people worldwide have diabetic retinopathy. 6.2 percent of those with diabetes face vision-threatening cases. By 2030, 191 million people will have it.
| Year | Estimated Global Prevalence of Diabetic Retinopathy |
|---|---|
| Current | 22.3% |
| 2030 | 191 Million People |
U.S. Impact: 9.6 Million Affected Americans
In the U.S., 9.6 million people have diabetic retinopathy. It’s a top reason for vision loss in adults 25-74. Knowing the risks and taking steps to prevent it is important.
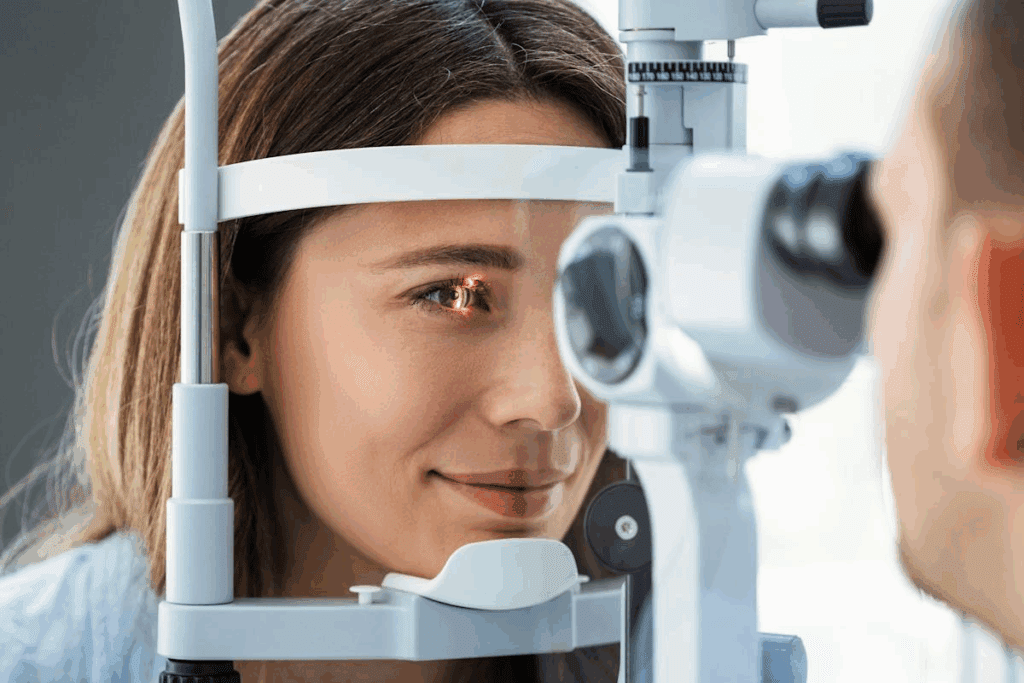
Early treatment and detection can greatly lower vision loss risks. Regular eye exams are vital for people with diabetes to check their retina’s health.
Risk Factors and Causes of Diabetic Retinopathy
Knowing the risk factors for diabetic retinopathy is key to preventing and managing it. This condition affects the blood vessels in the retina. It can lead to vision loss if not treated.
Duration of Diabetes
The longer you have diabetes, the higher your risk of diabetic retinopathy. The Wisconsin Epidemiologic Study of Diabetic Retinopathy (WESDR) found that after 20 years, almost all type 1 and 60% of type 2 diabetes patients have retinopathy. This shows why managing diabetes long-term is vital.
Blood Glucose Control
Keeping blood sugar levels in check is essential to prevent diabetic retinopathy. Hyperglycemia can harm the blood vessels in the retina. Studies have found that controlling blood sugar can lower the risk of retinopathy.
Hypertension and Cholesterol Levels
Hypertension and abnormal cholesterol levels also increase the risk of diabetic retinopathy. Managing these conditions through lifestyle changes and medication can help. Regular checks of blood pressure and cholesterol are important in diabetes care.
Genetic Factors
Genetics also play a part in diabetic retinopathy. Those with a family history of diabetes or retinopathy are at higher risk. Knowing your genetic risk can help in early detection and tailored management plans.
The main risk factors for diabetic retinopathy are:
- Duration of diabetes
- Poor blood glucose control
- Hypertension
- Abnormal cholesterol levels
- Genetic predisposition
By managing these risk factors, we can lower the risk and slow the progression of diabetic retinopathy. This helps protect the vision of people with diabetes.
Stage 1: No Apparent Diabetic Retinopathy
The first stage of diabetic retinopathy shows no signs of the disease. People with diabetes may not see any symptoms. It’s important to keep an eye on their health closely.
Baseline Eye Health in Diabetic Patients
It’s key to know a diabetic’s eye health from the start. This first check helps doctors see where the patient stands and spot risks early.
Diabetic patients should get regular eye exams. These can catch retinopathy early. They help doctors track the disease and plan the best treatment.
Early Detection Importance
Finding diabetic retinopathy early is vital to save vision. Even without symptoms, regular visits can spot changes in the retina.
Regular eye exams are essential. They can spot early signs like microaneurysms and hemorrhages. This is before symptoms show up.
Preventive Strategies at This Stage
Even at Stage 1, preventing diabetic retinopathy is important. Keeping blood sugar in check, managing blood pressure, and living a healthy lifestyle are key.
| Preventive Measure | Description | Benefit |
|---|---|---|
| Blood Sugar Control | Managing blood glucose levels through diet, exercise, and medication | Reduces risk of retinopathy progression |
| Blood Pressure Management | Controlling hypertension through lifestyle changes and medication | Slows down retinopathy progression |
| Healthy Lifestyle | Maintaining a balanced diet and regular physical activity | Improves overall health and reduces diabetes complications |
By following these steps, diabetics can lower their risk of retinopathy. They can also slow its progress if it starts.
Stage 2: Mild Nonproliferative Diabetic Retinopathy (NPDR)
Mild NPDR shows the first signs of diabetic retinopathy. It starts with microaneurysms, which are small spots on the retina. These signs are important for catching the disease early.
Defining Characteristics of Mild NPDR
The main sign of mild NPDR is microaneurysms. These are small bulges in the retinal capillaries. They are the first visible signs of diabetic retinopathy. Microaneurysms show the disease is getting worse and are found during eye exams.
Microaneurysms: The First Visible Signs
Microaneurysms look like tiny, round, red spots on the retina. They happen when the blood vessel walls weaken because of diabetes. Seeing microaneurysms means diabetic retinopathy is affecting the retina. Finding these changes early is key to acting fast.
Symptoms and Visual Impact
At this stage, people might not notice many symptoms. Their vision usually stays the same. But, some might see their vision get a bit blurry or notice floaters. It’s important to keep getting eye exams to watch for any changes.
Monitoring Requirements
People with mild NPDR need to see their eye doctor often. How often depends on their health and other factors. Usually, they should go back for exams every 6 to 12 months. Keeping blood sugar levels in check and managing blood pressure also helps slow down the disease.
As
“The key to managing diabetic retinopathy lies in early detection and consistent monitoring.”
, says regular eye care is very important for people with diabetes.
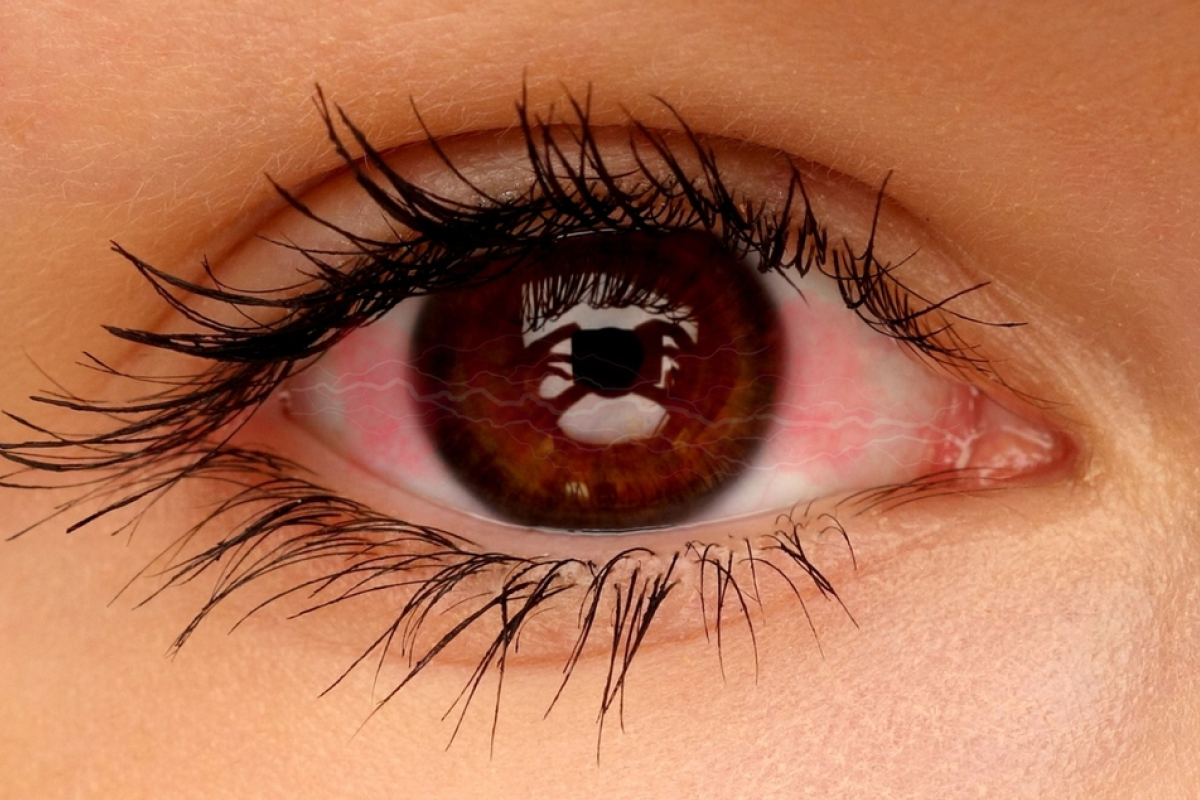
Stage 3: Moderate Diabetic Retinopathy – Critical Warning Signs
Stage 3 of diabetic retinopathy is a critical point. At this stage, the condition progresses, and significant changes occur in the retina. These changes can threaten vision.
Progression from Mild to Moderate NPDR
The transition from mild to moderate NPDR is marked by an increase in retinal hemorrhages and microaneurysms. We observe a more pronounced impact on the retinal blood vessels. This indicates a worsening of the condition.
This progression signifies that the disease is advancing. It requires closer monitoring.
Retinal Hemorrhages and Vascular Changes
Moderate NPDR is characterized by more extensive retinal hemorrhages and vascular changes. Retinal hemorrhages are a hallmark of this stage. They result from the weakening of retinal blood vessels.
These changes can lead to significant vision problems if not addressed promptly.
Moderate Nonproliferative Diabetic Retinopathy with Macular Edema
One of the complications of moderate NPDR is the development of macular edema. This is a condition where fluid accumulates in the macula. The macula is the part of the retina responsible for sharp, central vision.
This can lead to significant vision changes. These include blurred vision and decreased visual acuity.
Vision Changes at This Stage
At Stage 3, patients may start to notice more pronounced vision changes. These include fluctuations in vision and difficulty with reading or other daily activities.
If left untreated, the risk of vision loss increases. Timely intervention is critical.
We emphasize the importance of regular eye exams and monitoring. By controlling blood sugar levels and addressing retinal changes promptly, we can mitigate the risk of further vision deterioration.
Stage 4: Severe Nonproliferative Diabetic Retinopathy
Severe NPDR is a critical stage in diabetic retinopathy. It shows severe retinal changes that can cause significant vision loss. It’s important to address it quickly.
Identifying Severe NPDR Using the “4-2-1 Rule”
The “4-2-1 rule” helps diagnose Severe NPDR. It looks for:
- Diffuse retinal hemorrhages in all four quadrants
- Venous beading in at least two quadrants
- Intraretinal microvascular anomalies in at least one quadrant
This rule helps doctors understand the severity and plan the best treatment.
Retinal Ischemia and Its Consequences
Severe NPDR leads to retinal ischemia. This is when the retina doesn’t get enough blood. It can cause:
- Reduced vision
- Increased risk of neovascularization
- Potential for further complications such as vitreous hemorrhage
Retinal ischemia is a key factor in diabetic retinopathy’s progression.
Vision Threats and Quality of Life Impact
At Severe NPDR, vision threats are high. These include:
| Vision Threat | Description | Impact on Quality of Life |
|---|---|---|
| Vision Loss | Gradual or sudden loss of vision due to retinal damage | Significant impact on daily activities and independence |
| Blurred Vision | Distorted vision due to macular edema or retinal ischemia | Affects reading, driving, and other daily tasks |
Treatment Urgency at This Stage
Timely and effective treatment is key at this stage. Options include:
- Laser photocoagulation to reduce edema and prevent further vision loss
- Anti-VEGF injections to reduce neovascularization and edema
- Vitrectomy in advanced cases to remove blood or scar tissue
Quick action can greatly improve outcomes and save vision.
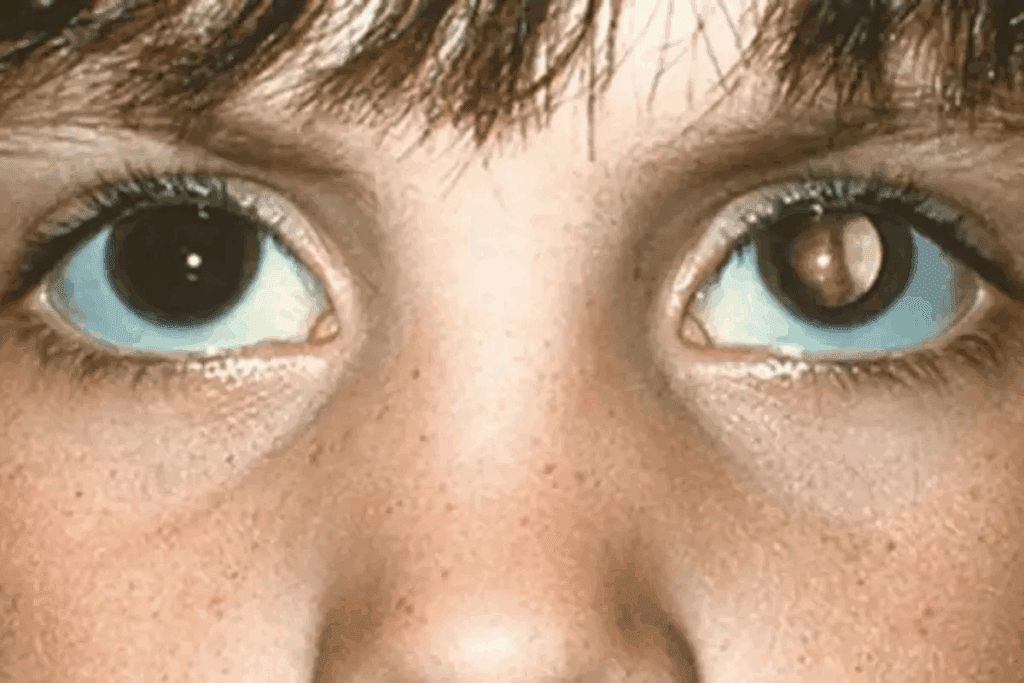
Stage 5: Proliferative Diabetic Retinopathy (PDR)
Diabetic retinopathy gets worse and reaches its fifth stage. The retina starts making new blood vessels. This can cause serious problems.
Neovascularization Process
The retina makes new blood vessels because it needs oxygen. But these new vessels are weak and can leak. This leads to more issues.
New vessels can grow in different parts of the eye. This can cause blood to leak into the vitreous gel. It can also make the retina detach from its base.
Major Complications of PDR
The main problems with PDR come from the new blood vessels. These include:
- Vitreous hemorrhage: Bleeding into the vitreous gel can cause sudden vision loss.
- Tractional retinal detachment: The formation of fibrous tissue along with new blood vessels can cause the retina to detach.
- Neovascular glaucoma: New vessels can grow on the iris and block the drainage of fluid, leading to increased intraocular pressure.
These issues can really hurt a person’s quality of life. It shows how important it is to manage PDR well.
Vision Loss Risk and Management
Not treating PDR can lead to a big risk of losing vision. But, with the right treatment, this risk can go down. Treatments include laser photocoagulation and anti-VEGF injections.
People with PDR should stay close to their doctors. They need to watch the disease and change treatments if needed. Regular eye checks are key to catching problems early and stopping vision loss.
Diabetic Macular Edema: A Vision-Threatening Complication
Diabetic macular edema is a serious problem that can cause vision loss if not treated. It happens when fluid builds up in the macula, the part of the retina that helps us see clearly. This swelling can harm our vision.
Understanding Macular Edema in Diabetic Retinopathy
Macular edema is when fluid and proteins build up in the macula. In diabetic retinopathy, this fluid leaks into the macula because of a damaged blood-retinal barrier. This can cause blurry vision, blind spots, and even vision loss.
The cause of diabetic macular edema is complex. It involves inflammation, oxidative stress, and factors like VEGF.
Diagnosis and Classification
To diagnose diabetic macular edema, doctors do a thorough eye exam. They use optical coherence tomography (OCT) to check the retina’s thickness. Fundus fluorescein angiography (FFA) helps spot leaks and ischemia.
Doctors classify diabetic macular edema based on its severity and if it affects the center of the macula. This helps decide the best treatment and predict how well the patient will see.
| Classification | Description | Treatment Approach |
|---|---|---|
| Mild DME | Some retinal thickening or hard exudates | Observation, control of systemic factors |
| Moderate DME | Retinal thickening or hard exudates in the posterior pole | Laser photocoagulation, anti-VEGF therapy |
| Severe DME | Retinal thickening or hard exudates involving the center of the macula | Anti-VEGF injections, vitreoretinal surgery |
Treatment Approaches for Diabetic Macular Edema
Treatment for diabetic macular edema has changed a lot. Anti-VEGF injections are now a key part of treatment. Other options include laser photocoagulation, corticosteroids, and surgery for severe cases.
Anti-VEGF Therapy: This treatment involves injections that block VEGF. It helps reduce swelling and improve vision.
Laser Photocoagulation: Laser treatment can help by closing leaking blood vessels and reducing ischemia.
Visual Prognosis
The outlook for vision in diabetic macular edema depends on how severe it is and how well it responds to treatment. Catching it early and treating it right is key to keeping your vision.
Thanks to new treatments, many people can see better and live better lives. But, it’s important to keep watching and treating it to stop it from coming back.
Comprehensive Management Across All Stages
Managing diabetic retinopathy well means controlling blood sugar and using the right treatments. It’s a complex condition needing a detailed management plan.
Blood Sugar and Blood Pressure Control
Keeping blood sugar and blood pressure in check is key. Tight glycemic control helps prevent or slow diabetic retinopathy. We suggest regular blood glucose checks and keeping levels in target range.
Also, managing blood pressure is important. Hypertension can make diabetic retinopathy worse, so it’s essential to control it.
| Parameter | Target Value | Benefit |
|---|---|---|
| Blood Glucose (Fasting) | 70-130 mg/dL | Reduces risk of Medical Expert |
| Blood Pressure | <140/90 mmHg | Slows Medical Expert |
Laser Photocoagulation Therapy
Laser photocoagulation is a common treatment for diabetic retinopathy. It uses laser burns to reduce swelling and prevent vision loss. This is often used in more advanced stages.
There are different laser therapies, like focal/grid laser for diabetic macular edema and pan-retinal photocoagulation (PRP) for proliferative diabetic retinopathy. The right therapy depends on the disease’s specifics.
Anti-VEGF Injections
Anti-vascular endothelial growth factor (anti-VEGF) injections are key for diabetic macular edema and proliferative diabetic retinopathy. They reduce swelling, improve vision, and lower the risk of vision loss.
Common anti-VEGF agents include ranibizumab, bevacizumab, and aflibercept. The injection frequency varies based on patient response and drug type.
Vitrectomy and Advanced Surgical Options
In severe cases, surgery like vitrectomy may be needed. It removes the vitreous gel to repair retinal detachments, remove blood, or relieve traction on the retina.
Modern surgical techniques have improved vitrectomy outcomes. Surgery is usually considered when other treatments fail or are not suitable.
We stress that a good diabetic retinopathy management plan combines these strategies. It’s tailored to each patient’s needs and disease stage.
Conclusion: Living with Diabetic Retinopathy
Living with diabetic retinopathy means you need to keep managing it to avoid losing your vision. We talked about the different levels of diabetic retinopathy and why managing it well is key.
Managing diabetic retinopathy means getting regular eye checks, keeping your blood sugar and blood pressure in check. You also need to follow your treatment plan. This might include laser therapy, injections, or surgery.
Knowing what causes diabetic retinopathy helps you take steps to manage it. Treatment should fit your needs, and ongoing care is vital. This helps prevent vision loss and keeps your quality of life good.
We stress the need for teamwork between healthcare providers and those with diabetic retinopathy. This teamwork is essential for the best management and treatment results.
FAQ
What are the stages of diabetic retinopathy?
Diabetic retinopathy has five stages. These include no apparent diabetic retinopathy, mild nonproliferative diabetic retinopathy (NPDR), moderate NPDR, severe NPDR, and proliferative diabetic retinopathy (PDR).
What is mild nonproliferative diabetic retinopathy?
Mild NPDR is the first stage of diabetic retinopathy. It shows up as microaneurysms. These are small swellings in the retinal blood vessels.
How does diabetic retinopathy affect vision?
Diabetic retinopathy can damage the retina’s blood vessels. This leads to leakage, bleeding, or the growth of new, fragile vessels. These can cause scarring and retinal detachment, leading to vision loss.
What is diabetic macular edema?
Diabetic macular edema is a complication of diabetic retinopathy. Fluid builds up in the macula. This part of the retina is key for sharp, central vision. It causes vision distortion and loss.
How is diabetic retinopathy diagnosed?
Diabetic retinopathy is diagnosed with a thorough eye exam. This includes visual acuity testing and a dilated eye exam. Retinal imaging and optical coherence tomography (OCT) are also used. They check retinal thickness and detect fluid accumulation.
What are the risk factors for developing diabetic retinopathy?
Risk factors include how long you’ve had diabetes, poor blood glucose control, and high blood pressure. High cholesterol levels and genetic predisposition also play a role.
Can diabetic retinopathy be prevented?
While you can’t prevent diabetic retinopathy completely, early detection and management can help. Regular eye exams, controlling blood sugar and blood pressure, and timely treatment can reduce vision loss risk.
What are the treatment options for diabetic retinopathy?
Treatments include laser photocoagulation therapy and anti-vascular endothelial growth factor (anti-VEGF) injections. Vitrectomy and advanced surgical options are also available. The choice depends on the stage and severity of the condition.
How does blood sugar control impact diabetic retinopathy?
Good blood sugar control is key in preventing diabetic retinopathy. High blood glucose levels damage the retinal blood vessels over time.
What is proliferative diabetic retinopathy?
Proliferative diabetic retinopathy is the most advanced stage. It’s marked by the growth of new, fragile blood vessels. If untreated, it can lead to severe vision loss.
What is the “4-2-1 rule” in diabetic retinopathy?
The “4-2-1 rule” is a guideline for identifying severe NPDR. It looks for specific retinal changes that signal a high risk of progressing to proliferative diabetic retinopathy.
How often should individuals with diabetes have their eyes examined?
People with diabetes should get a thorough eye exam at least once a year. They may need more frequent exams based on their diabetic retinopathy severity.
References
National Center for Biotechnology Information. Evidence-Based Medical Guidance. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4239702/