Cranial Nerve 3, also known as the oculomotor nerve, is key for most of our eye movements. It’s one of 12 pairs of cranial nerves that connect directly to the brain. This important nerve controls the ciliary muscles and pupil sphincter. It also manages four extraocular muscles and the levator palpebrae superioris muscle in the eyelid. The best guide to nerve eye movement. Learn how 3 critical nerves (CN III, IV, VI) control your eyes and what happens when they fail.
Palsy affecting Cranial Nerve 3 can cause serious symptoms like double vision and eyelid drooping. It’s vital to understand this nerve‘s role and how palsy impacts it. At Liv Hospital, we offer top-notch neuro-ophthalmologic care for those with Cranial Nerve 3 issues.
Key Takeaways
- Cranial Nerve 3 controls most eye movements and is key for good vision.
- Palsy affecting Cranial Nerve 3 can cause double vision and eyelid drooping.
- Early detection and treatment are vital for managing Cranial Nerve 3 palsy.
- Liv Hospital provides advanced neuro-ophthalmologic care for patients with Cranial Nerve 3 dysfunction.
- Understanding Cranial Nerve 3 and its functions is essential for diagnosing related disorders.
Understanding Cranial Nerve 3: The Oculomotor Nerve

It’s key to know about the oculomotor nerve, the third cranial nerve. This nerve is vital for eye health. It helps control eye movements and other functions.
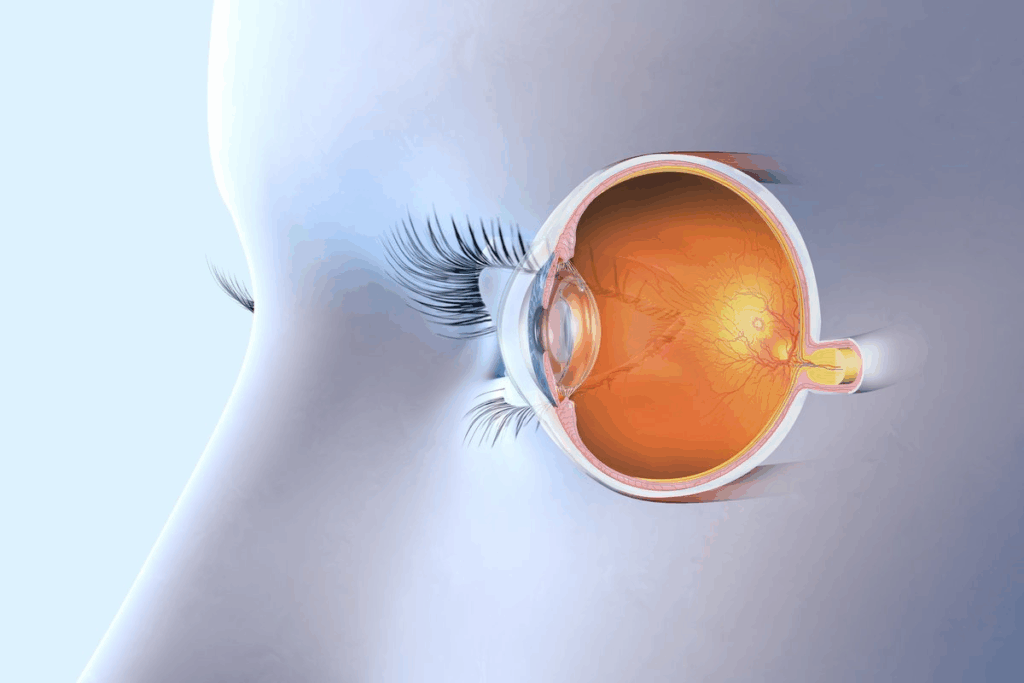
Definition and Anatomical Location
The oculomotor nerve, or cranial nerve 3, controls most eye movements. This includes rotating the eyeball and opening the eyelid. It starts in the midbrain and goes to the orbit through the superior orbital fissure.
This nerve has motor and parasympathetic fibers. The motor fibers work with four extraocular muscles. The parasympathetic fibers help the pupil and lens for clear vision.
The N N Nachachacotic Nn and Volpe NJ,eriatric Neuro-Ophthalmology
Details on “N N Nachachacotic Nn” are not clear. But, Volpe NJ’s work in geriatric neuro-ophthalmology is important. It shows how knowing about cranial nerves helps in treating eye problems, even in older adults.
Function | Muscle/Nerve Involved | Clinical Significance |
Eye Movement | Superior Rectus, Medial Rectus, Inferior Rectus, Inferior Oblique | Palsy can lead to diplopia and strabismus |
Pupillary Constriction | Parasympathetic fibers of CN III | Affects pupil size and reactivity |
Eyelid Elevation | Levator Palpebrae Superioris | Ptosis can occur with CN III palsy |
Anatomy and Structure of the Third Cranial Nerve
The third cranial nerve, or oculomotor nerve, is complex. It has both parasympathetic and somatic parts. This nerve is key for eye movements and functions.
Nerve Nuclei and Pathway Through the Brain
The oculomotor nerve starts from the oculomotor nucleus in the midbrain. This nucleus has several subnuclei. Each one controls a different extraocular muscle.
The nerve fibers leave the nucleus and go down through the midbrain. They pass near the cerebral peduncle and the red nucleus.
When it leaves the brainstem, it goes between two arteries. This is in the interpeduncular fossa. Then, it moves forward to the cavernous sinus, surrounded by other important structures.
Dual Components: Parasympathetic and Somatic Fibers
The oculomotor nerve has two types of fibers. Parasympathetic fibers control the pupillary light reflex and accommodation. They come from the Edinger-Westphal nucleus and go to the ciliary ganglion.
Somatic fibers, on the other hand, control four extraocular muscles. These muscles help with eye movements like adduction, elevation, depression, and rotation.
The oculomotor nerve’s complex structure is vital for eye control. It manages eye movements, pupil size, and lens focus. Knowing its anatomy helps in diagnosing and treating nerve disorders.
How Cranial Nerve 3 Controls Eye Movement
The oculomotor nerve, or Cranial Nerve 3, is key for eye movement. It connects to muscles that move and position the eyeball.
The Four Extraocular Muscles Under CN3 Control
Cranial Nerve 3 manages four of the six extraocular muscles. These muscles are vital for eye movement precision.
- The medial rectus muscle, which rotates the eye inward.
- The superior rectus muscle, responsible for elevating the eye.
- The inferior rectus muscle, which depresses the eye.
- The inferior oblique muscle, involved in rotating the eye upward and outward.
These muscles work together for smooth eye movement. They help us track objects and keep binocular vision.
Pupillary and Accommodation Functions
Cranial Nerve 3 also controls the iris sphincter muscle and ciliary muscles. It manages two important functions:
- Pupillary constriction: Adjusting pupil size with light changes.
- Accommodation: Focusing on near objects by lens shape change.
These functions are key for adjusting to light changes and near vision tasks, like reading.
Function | Muscle Involved | Role of Cranial Nerve 3 |
Eye Movement | Medial Rectus, Superior Rectus, Inferior Rectus, Inferior Oblique | Motor innervation for precise eye movement |
Pupillary Constriction | Iris Sphincter Muscle | Parasympathetic innervation for pupil size adjustment |
Accommodation | Ciliary Muscles | Parasympathetic innervation for lens shape adjustment |
Cranial Nerve 3 is essential for our visual interaction and interpretation. It controls eye movement, pupil size, and lens shape.
Oculomotor Nerve Palsy: Definition and Classification
To understand oculomotor nerve palsy, you need to know about the nerve’s structure and how it works. This condition, also called CN3 palsy, impacts the third cranial nerve. This nerve is key for eye movement.
Oculomotor nerve palsy can be split into different types. This split is based on how much of the nerve is affected and if the pupil is involved. Knowing this helps doctors figure out the cause and how to treat it.
Complete vs. Partial CN3 Palsy
Oculomotor nerve palsy can be either complete or partial. Complete CN3 palsy means the nerve is fully paralyzed. This limits eye movement a lot. On the other hand, partial CN3 palsy means some muscles are weak but not all. This might allow for some eye movement.
It’s important to tell the difference between complete and partial palsy. This helps doctors understand how damaged the nerve is. It also helps decide the best treatment.
Pupil-Involving vs. Pupil-Sparing Palsy
Oculomotor nerve palsy can also be classified by the pupil’s involvement. Pupil-involving palsy means the nerve’s fibers that control the pupil are affected. This causes the pupil to dilate. Pupil-sparing palsy means the fibers that control the pupil are not affected.
Whether the pupil is involved or spared is very important. It helps doctors guess what might be causing the palsy. Pupil-involving palsy might suggest a problem like an aneurysm. Pupil-sparing palsy is more likely to be caused by something like diabetes.
Classification | Characteristics | Common Causes |
Complete CN3 Palsy | Total paralysis of oculomotor nerve-innervated muscles | Aneurysm, trauma |
Partial CN3 Palsy | Varying degrees of muscle weakness | Ischemia, partial nerve damage |
Pupil-Involving Palsy | Pupillary dilation due to parasympathetic fiber involvement | Compressive lesions (aneurysm, tumor) |
Pupil-Sparing Palsy | Pupil not affected; parasympathetic fibers spared | Ischemic causes (diabetes, hypertension) |
Recognizing Symptoms of Cranial Nerve 3 Damage
It’s important to know the signs of cranial nerve 3 damage to get the right treatment. The third cranial nerve, or oculomotor nerve, helps control eye movements and functions. Damage to this nerve can cause several symptoms that can be very hard to deal with.
Ptosis: The Drooping Eyelid
One common sign is ptosis, or a drooping eyelid. This happens because the oculomotor nerve controls the muscle that lifts the eyelid. If this muscle weakens, the eyelid may drop, making it hard to see.
Diplopia and Visual Disturbances
Diplopia, or seeing double, is another symptom. It occurs when the nerve damage affects the eye muscles. This misalignment can cause double vision, making everyday tasks difficult.
The “Down and Out” Eye Position
A sign of oculomotor nerve palsy is the “down and out” eye position. This happens because other nerves control the eye muscles differently. The eye looks down and outward, which is a clear sign of the problem.
Pupillary Abnormalities
Pupillary abnormalities are also a key indicator. The oculomotor nerve helps control how the pupils react. Damage can cause a pupil to dilate, which is a serious sign and might mean there’s a blockage, like an aneurysm.
Symptom | Description | Cause |
Ptosis | Drooping eyelid | Weakness of levator palpebrae superioris muscle |
Diplopia | Double vision | Misalignment of the eyes due to extraocular muscle dysfunction |
“Down and Out” Eye Position | Eye deviated downward and outward | Unopposed action of muscles controlled by trochlear and abducens nerves |
Pupillary Abnormalities | Dilated pupil | Damage to parasympathetic fibers controlling pupillary constriction |
Common Causes of Oculomotor Nerve Damage
The oculomotor nerve can be damaged by several common causes. Knowing these causes helps in diagnosing and treating oculomotor nerve palsy.
Vascular Disorders: Diabetes and Aneurysms
Vascular disorders are a big reason for oculomotor nerve damage. Diabetes can damage nerves due to high blood sugar, known as diabetic neuropathy. Diabetes is a leading cause of oculomotor nerve palsy in adults. Aneurysms, or abnormal blood vessel bulges, can also press on the nerve, causing palsy. “The presence of an aneurysm is a medical emergency requiring immediate attention,” say doctors.
Traumatic Brain Injuries
Traumatic brain injuries (TBI) are another common cause. The oculomotor nerve can get hurt directly or indirectly from trauma. For example, a severe head injury can stretch or compress the nerve, causing palsy. The severity of the palsy depends on the injury’s extent.
Tumors and Compression Syndromes
Tumors, both benign and malignant, can press on the oculomotor nerve, causing damage. Tumors in the brain or nearby can put pressure on the nerve, affecting its function. Compression syndromes, where the nerve is squeezed between structures, can also cause oculomotor nerve palsy.
Inflammatory and Infectious Etiologies
Inflammatory and infectious conditions can also damage the oculomotor nerve. Infections like meningitis or conditions like multiple sclerosis can inflame the nerve, leading to palsy. Knowing the cause is key for the right treatment.
In conclusion, oculomotor nerve damage can come from vascular disorders, traumatic brain injuries, tumors, and inflammatory or infectious conditions. Finding the exact cause is vital for effective management and treatment.
Diagnostic Approach to Cranial Nerve 3 Palsy
When diagnosing cranial nerve 3 palsy, doctors use many tools. They look at clinical exams, neuro-ophthalmologic tests, and neuroimaging. This helps find the cause.
Clinical Examination and Neuro-ophthalmologic Tests
A detailed clinical exam is key to diagnosing cranial nerve 3 palsy. Doctors check eye movements, pupillary reactions, and eyelid position. Neuro-ophthalmologic tests also help understand the oculomotor nerve’s function and the palsy’s extent.
Important parts of the clinical exam are:
- Evaluating eye movements and alignment
- Checking pupillary size and reactivity
- Looking at eyelid position and function
Advanced Neuroimaging: MRI, CT, and Angiography
Neuroimaging is vital in finding the cause of cranial nerve 3 palsy. MRI, CT, and angiography help see the oculomotor nerve and nearby structures. They spot compressive lesions, vascular issues, or other problems.
Neuroimaging Technique | Primary Use in Diagnosing CN3 Palsy | Key Benefits |
MRI | Detailed view of the oculomotor nerve and soft tissues | High sensitivity for soft tissue issues |
CT | Quick look at acute trauma or hemorrhage | Quick and widely available |
Angiography | Looks at vascular structures and aneurysms | Crucial for vascular causes of CN3 palsy |
Differential Diagnosis: Distinguishing from Other Ocular Conditions
Differential diagnosis is key in managing cranial nerve 3 palsy. Many ocular conditions can look similar. Doctors must tell CN3 palsy apart from other causes of diplopia, ptosis, or pupillary issues. This includes myasthenia gravis, thyroid eye disease, or other cranial neuropathies.
Important factors in differential diagnosis are:
- Pupillary involvement: Presence or absence of pupillary dilation
- Pattern of eye movement limitation
- Presence of other neurological symptoms
By combining clinical findings with advanced diagnostic tools, doctors can accurately diagnose cranial nerve 3 palsy. They can then find the cause and guide treatment.
Treatment Strategies for Oculomotor Nerve Palsy
Treating oculomotor nerve palsy involves several steps. It depends on the cause and how severe it is. A good plan might include medicine, non-surgical methods, and surgery.
Medical Management of Underlying Causes
Managing the cause of oculomotor nerve palsy is key. If diabetes or high blood pressure is the cause, controlling these is vital. For aneurysms, quick surgery or endovascular treatment is needed.
Medicines can also help. For example, pain relief is important. Doctors might prescribe painkillers to help with discomfort.
Non-surgical Interventions: Patching, Prisms, and Botulinum Toxin
Non-surgical methods can help a lot. Patching the good eye can stop double vision. Prisms in glasses can also help. Botulinum toxin injections can relax muscles and align the eyes.
These methods are great in the early stages. They help manage symptoms while waiting for recovery.
Intervention | Purpose | Benefits |
Patching | Eliminate diplopia | Immediate relief from double vision |
Prisms | Redirect light to reduce double vision | Can be adjusted or changed as needed |
Botulinum Toxin | Temporarily paralyze overactive muscles | Can help realign the eyes |
Surgical Options for Persistent Palsy
If oculomotor nerve palsy doesn’t get better, surgery might be needed. Surgery can fix eye alignment or ptosis (drooping eyelid).
Deciding on surgery depends on several things. These include how bad the symptoms are, how they affect daily life, and if there’s a chance for improvement.
Recovery and Prognosis Factors
Recovering from oculomotor nerve palsy is complex. It depends on many things. The speed and extent of recovery differ for everyone. This is based on the cause, how severe it is, and any other health issues.
Predictors of Favorable Outcomes
Some things can help a patient recover better from oculomotor nerve palsy. These include:
- Cause of the palsy: Palsy from diabetes or high blood pressure usually has a better chance of recovery. This is different from palsy caused by injury or tumors.
- Age of the patient: Younger people tend to recover faster.
- Severity of the initial damage: Those with partial palsy often do better than those with complete palsy.
- Presence of other medical conditions: Patients with fewer health problems usually have better outcomes.
Knowing these factors helps doctors give better advice and treatment plans to each patient.
Typical Recovery Timeline and Expectations
The time it takes to recover from oculomotor nerve palsy varies a lot. Generally, patients can expect the following:
Timeframe | Expected Recovery |
0-3 months | Initial improvement in symptoms, mostly in partial palsy cases. |
3-6 months | More improvement, with some patients seeing big changes. |
6-12 months | More recovery, but slower. Some might fully recover. |
It’s key for patients to have realistic hopes and work closely with their doctors. This helps track progress and adjust treatment plans as needed.
We stress the need for a full care plan. It should cover both physical and emotional recovery from oculomotor nerve palsy. Understanding what affects recovery and having realistic hopes helps patients deal with this tough condition better.
Prevention and Management for At-Risk Individuals
We can lower the risk of oculomotor nerve palsy by using good prevention methods. This means tackling different risk factors and starting early interventions.
Risk Reduction Strategies for Vascular Causes
Vascular causes are a big risk for oculomotor nerve palsy. To lower this risk, we suggest these steps:
- Managing Hypertension: Keeping blood pressure in check through lifestyle changes and meds can cut down vascular-related oculomotor nerve palsy risk.
- Diabetes Management: Keeping diabetes under control, by keeping blood sugar levels in range, is key to avoiding vascular problems.
- Lifestyle Modifications: Living a healthy life, with a balanced diet, regular exercise, and no smoking, can lessen vascular risks.
Monitoring and Early Intervention Approaches
Spotting and acting early is key to managing oculomotor nerve palsy well. We advise:
- Regular Eye Examinations: People at risk should get regular eye checks to catch oculomotor nerve palsy signs early.
- Neurological Monitoring: Watching for neurological symptoms and reporting any changes quickly helps in early action.
- Timely Medical Intervention: Getting medical help and treatment fast when symptoms show up can greatly improve results.
By following these steps, we can better handle oculomotor nerve palsy and lessen its effects on those at risk.
Conclusion
We’ve looked into cranial nerve 3, also known as the oculomotor nerve, and its key role in eye movement. Oculomotor nerve palsy can really affect someone’s life, leading to symptoms like ptosis, diplopia, and vision problems.
Diagnosing oculomotor nerve palsy involves a detailed check-up and advanced scans. Knowing the causes, like blood vessel issues, head injuries, and tumors, is key to managing it well.
Treatment options include managing the cause, using non-surgical methods like patching and prisms, and sometimes surgery. The outcome depends on the cause and how much nerve damage there is.
In short, cranial nerve 3 is essential for eye movement, and oculomotor nerve palsy needs quick diagnosis and treatment to avoid vision issues. Healthcare teams can provide the best care by understanding symptoms, causes, and treatments.
FAQ
What is cranial nerve 3, and what is its role in controlling eye movements?
Cranial nerve 3, also known as the oculomotor nerve, controls eye movements. It helps rotate the eyeball, constrict the pupil, and keeps the eyelid open. It affects four extraocular muscles and is key for pupillary and accommodation functions.
What is oculomotor nerve palsy, and how is it classified?
Oculomotor nerve palsy is damage to the third cranial nerve. It leads to problems with eye movements and other symptoms. It’s classified into complete and partial palsy, and whether it affects the pupil.
What are the common symptoms of cranial nerve 3 damage?
Symptoms include a drooping eyelid, double vision, and an “out and down” eye position. A dilated pupil is also a sign.
What are the common causes of oculomotor nerve damage?
Causes include vascular disorders like diabetes and aneurysms. Traumatic brain injuries, tumors, and infections also cause damage.
How is cranial nerve 3 palsy diagnosed?
Diagnosis involves a detailed clinical exam and neuro-ophthalmologic tests. Advanced imaging like MRI and CT scans help find the cause and extent of damage.
What are the treatment strategies for oculomotor nerve palsy?
Treatment includes managing the cause and non-surgical methods like patching and prisms. Surgery may be needed for persistent cases.
What factors influence recovery and prognosis in oculomotor nerve palsy?
Recovery depends on the cause, extent of damage, and timely treatment. Early intervention and effective management are key for a good outcome.
Can oculomotor nerve palsy be prevented?
Some cases can’t be prevented, but risk factors can be managed. This includes controlling vascular risk factors and avoiding head trauma.
What is the typical recovery timeline for oculomotor nerve palsy?
Recovery time varies based on the cause and damage. It can take months, and in some cases, recovery may not be complete.
What is the significance of cranial nerve 3 in overall eye health?
Cranial nerve 3 is vital for eye movements, pupillary functions, and eyelid opening. It’s essential for eye health and function.
What is the difference between pupil-involving and pupil-sparing oculomotor nerve palsy?
Pupil-involving palsy affects the pupil, while pupil-sparing palsy does not. Pupil-involving palsy often indicates a more serious cause.
How does cranial nerve 3 damage affect daily life?
Damage can cause eye movement problems, double vision, and other visual issues. These can make daily tasks difficult and affect independence.
References
National Center for Biotechnology Information. Evidence-Based Medical Guidance. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK541034/