We are on the brink of a big change with new cancer treatment. Many new discoveries are giving new hope to people all over the world. These breakthroughs in immunotherapy and targeted therapies are making a big difference in survival rates and how we care for patients.

These new treatments, like cellular immunotherapies, are not just adding more treatment options. They are also giving hope to millions of people. As we look into these new findings, we are here to help and support those fighting cancer.
Key Takeaways
- Immunotherapy is revolutionizing cancer care.
- Targeted therapies offer precise treatment options.
- Cellular immunotherapies are providing new hope for patients.
- Advancements in cancer therapy are improving survival rates.
- Patients worldwide are benefiting from these innovative treatments.
The Cancer Treatment Landscape in 2025
As we near 2025, the fight against cancer is changing fast. New research and tech are leading the way. The need for new treatments is urgent, with 316,950 new breast cancer cases and 42,680 deaths expected in the US.

Current Cancer Statistics and Projections
Cancer is a big challenge worldwide. In the US, the American Cancer Society predicts a lot of new cases and deaths in 2025. This shows how important it is to find new, effective treatments.
Knowing the current and future numbers is key for doctors, researchers, and patients. It helps plan and prepare for the future. Everyone is working hard to find a new cancer cure to help more people survive and live better.
The Paradigm Shift from Cytotoxic to Targeted Therapies
The way we treat cancer is changing. We’re moving from old, harsh treatments to new, targeted ones. These new treatments aim to hit cancer cells directly, with fewer side effects for healthy cells.
This change comes from a better understanding of cancer and new treatments. Cancer cure news often shares these breakthroughs, giving hope to those fighting cancer. By 2025, we’re looking forward to treatments that are more effective and less harsh, a big step in the fight against cancer.
The Rise of Immunotherapy in Oncology
Immunotherapy is a key player in the fight against cancer. It uses the body’s immune system to attack tumors. This method has changed cancer treatment, with 12 of the 28 FDA-approved drugs in 2025 being immunotherapies.
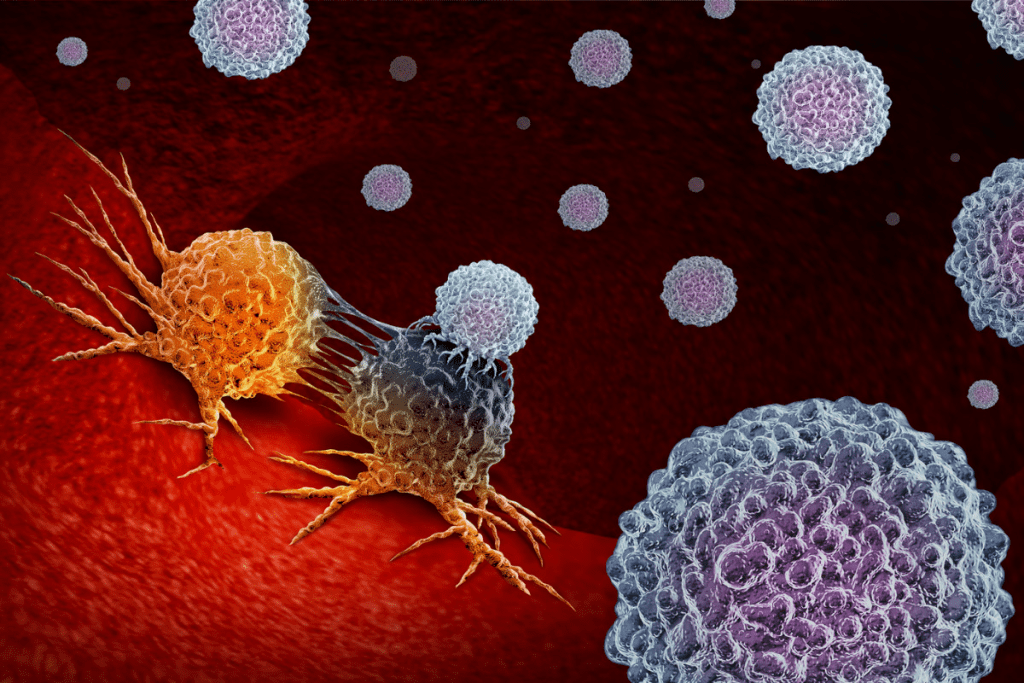
How Cancer Evades the Immune System
Cancer cells find ways to avoid the immune system. They use checkpoints and mechanisms to suppress the immune response. It’s important to understand these tactics to create effective treatments.
“The immune system can spot and destroy cancer cells,” “But tumors find ways to hide. Immunotherapy tries to stop these tricks.”
Principles of Immunotherapy Approaches
Immunotherapy boosts the body’s defenses against cancer. It can activate immune cells or use checkpoint inhibitors to enhance the immune response.
- Checkpoint inhibitors: Drugs that block proteins like PD-1 and CTLA-4, which normally dampen the immune response.
- Cancer vaccines: Therapies that stimulate the immune system to recognize and attack cancer cells.
- Adoptive T-cell therapy: A treatment where T cells are engineered to target specific cancer cells.
Reduced Toxicity Compared to Traditional Chemotherapy
Immunotherapy has a big advantage over traditional chemotherapy. It targets cancer cells more precisely, reducing harm to healthy tissues.
Immunotherapy is a major step forward in cancer treatment. It brings new hope for patients and doctors. As research grows, we’ll see more ways to use the immune system against cancer.
FDA’s Oncology Drug Revolution: 12 of 28 Approvals
The FDA is changing cancer treatment, with 12 out of 28 approvals being immunotherapies. The U.S. Food and Drug Administration has been approving new cancer treatments. A big part of these are immunotherapies, bringing new hope to patients everywhere.
Breakdown of Recent Immunotherapy Approvals
The FDA has approved many treatments for different cancers. Immunotherapies like pembrolizumab and nivolumab have been approved for various uses. This shows how the immune system can fight cancer.
We’re seeing more targeted therapies, too. Antibody-drug conjugates (ADCs) and CAR T-cell therapies are also getting approved. This variety is key to better patient care.
Regulatory Fast-Tracking for Promising Treatments
The FDA has fast-track programs for new treatments. The Breakthrough Therapy Designation is one such program. It helps bring innovative cancer treatments to market quickly.
- Fast Track designation
- Breakthrough Therapy designation
- Accelerated Approval
- Priority Review
These programs cut down the time for new cancer drugs to reach patients. They do this without sacrificing safety or effectiveness.
Real-World Effectiveness of Newly Approved Drugs
Clinical trials are important, but real-world evidence matters too. Studies show many new immunotherapies work well in more patients.
We’re watching how these treatments work over time. We also support research on their effectiveness in real-world use.
Antibody-Drug Conjugates: Smart Bombs Against Cancer
Cancer treatment is getting smarter, thanks to antibody-drug conjugates. These advanced treatments use antibodies to find cancer cells and then deliver drugs to kill them. This method is both precise and powerful.
The Three-Part Structure of ADCs
Antibody-drug conjugates (ADCs) are made of three parts: an antibody, a drug, and a linker. The antibody finds cancer cells. The drug kills them, but only after it gets inside the cell. This way, healthy cells are not harmed.
The three-part structure of ADCs is a big step forward. It means fewer side effects for patients. The antibody finds cancer cells, and the drug kills them once inside.
Current FDA-Approved ADCs and Their Targets
Many ADCs have been approved by the FDA to fight different cancers. For example, Trastuzumab deruxtecan is for HER2-positive breast cancer. Brentuximab vedotin is for certain types of lymphoma.
- Trastuzumab deruxtecan: Targets HER2-positive breast cancer.
- Brentuximab vedotin: Approved for relapsed or refractory Hodgkin lymphoma and systemic anaplastic large cell lymphoma.
- Inotuzumab ozogamicin: Used for relapsed or refractory B-cell precursor acute lymphoblastic leukemia.
Patient Selection Criteria for Optimal Response
Choosing the right patients is key for ADCs to work best. Biomarkers help find who will benefit most. For example, HER2 is important for some ADCs.
- Biomarker testing to identify target antigens.
- Assessment of previous treatments and their outcomes.
- Evaluation of the patient’s overall health and cancer stage.
By picking patients carefully, doctors can make ADCs more effective. This leads to better results and fewer side effects.
Immune Checkpoint Inhibitors: Removing the Brakes
Checkpoint inhibitors have changed cancer treatment by boosting the immune system. They offer new hope to patients and doctors. This has opened up new ways to fight cancer.
PD-1/PD-L1 and CTLA-4 Pathways
These inhibitors target cancer’s tricks to hide from the immune system. The PD-1/PD-L1 pathway lets cancer cells hide by binding to T-cells. CTLA-4 also plays a big role in controlling T-cells.
By blocking these pathways, the immune system can better find and fight cancer cells.
Pembrolizumab’s 34% Reduction in Head and Neck Cancer Recurrence
Pembrolizumab has shown great results in treating head and neck cancers. It has cut down recurrence by 34% in some patients. This shows how powerful immune checkpoint inhibitors can be.
This success in head and neck cancer shows its wide impact. As research grows, we’ll see these therapies used in more cancers.
Expanding Applications Beyond Common Cancers
Immune checkpoint inhibitors are not just for common cancers like melanoma and lung cancer. They’re being tested in rarer and harder-to-treat cancers. This shows their wide range of uses.
As we learn more about these treatments, we’ll see even more progress in cancer care. Their ability to help many cancers is huge. Ongoing research is key to unlocking this.
CAR T-Cell Therapy: Living Drugs
CAR T-cell therapy is a new way to fight cancer. It uses the body’s immune system to attack cancer cells. First, T-cells are taken from the patient. Then, they are changed to find and kill cancer cells. After that, they are put back into the body.
Engineering Process for CAR T-Cells
Making CAR T-cells is a detailed process. T-cells are first taken from the blood. They are then changed in a lab to recognize cancer cells. These cells are then grown and ready to be given back to the patient.
Key aspects of the engineering process include:
- Choosing the right target for cancer cells
- Creating the CAR construct
- Changing T-cells with the CAR gene
- Growing CAR T-cells to the right number
Current Approved Blood Cancer Applications
CAR T-cell therapy is helping with some blood cancers. It’s approved for certain types of lymphoma, leukemia, and multiple myeloma. This gives patients new hope when other treatments fail.
It works well because it targets cancer cells without harming healthy ones.
Challenges in Solid Tumor Treatment
But CAR T-cell therapy is harder to use on solid tumors. Solid tumors can make CAR T-cells less effective. Researchers are looking at new ways to help, like combining treatments.
Managing Cytokine Release Syndrome
One big side effect is cytokine release syndrome (CRS). It’s a serious condition caused by the immune cells’ reaction. Doctors watch patients closely and use medicines like tocilizumab to help.
It’s important to manage CRS to keep CAR T-cell therapy safe.
New Cancer Treatment Breakthroughs in Clinical Trials
The fight against cancer is getting a boost from new treatments in clinical trials. These innovative therapies are showing great promise. They are changing the way we treat cancer.
The INTERLACE Trial’s 40% Mortality Reduction in Cervical Cancer
The INTERLACE trial is a big win, showing a 40% drop in cervical cancer deaths. It tested a new mix of treatments for advanced cervical cancer. This breakthrough could lead to better care for patients.
The trial found that this new treatment not only saved lives but was also safe at Memorial Sloan Kettering Cancer Center. “The INTERLACE trial shows the power of teamwork in finding new treatments.”
Novel Combination Approaches
New ways of treating cancer involve mixing different treatments. This includes combining immunotherapy and targeted therapy. These mixes aim to beat the challenges of single treatments.
- Combining immunotherapies with other treatments to enhance efficacy
- Targeting multiple pathways simultaneously to reduce resistance
- Exploring new sequences of treatment to optimize patient outcomes
By trying these new mixes, we’re learning how to use them in real-world treatment.
Biomarker Discovery for Treatment Selection
Biomarkers are key in choosing the right treatment. They help doctors pick the best therapy for each patient. This makes cancer care more precise and effective.
“The use of biomarkers in treatment is changing cancer care. It’s making treatments more tailored and effective.”
As research keeps moving forward, we’ll see more progress in biomarkers and cancer treatment.
Personalized Cancer Vaccines: Tailored Immunity
Personalized cancer vaccines are changing how we fight cancer. They help the immune system find and fight cancer cells. This makes treatments more effective and targeted.
mRNA Platform Technology
mRNA platform technology is key in making these vaccines. It uses messenger RNA to tell cells to make proteins found on cancer cells. This starts an immune response.
This tech is flexible, allowing vaccines to be quickly made for each patient.
The process includes:
- Identifying tumor-specific antigens
- Designing and manufacturing mRNA that encodes these antigens
- Delivering the mRNA to the patient’s cells
- Stimulating an immune response against the cancer cells
Neoantigens and Tumor-Specific Targeting
Neoantigens are proteins on cancer cells but not normal cells. They are perfect targets for these vaccines. This means the vaccines can attack cancer cells without harming healthy cells.
This focus on neoantigens is a big step forward. It leads to a more precise and effective fight against cancer. Studies show these vaccines can shrink tumors and improve patient outcomes.
Current Clinical Trial Results
Clinical trials show personalized cancer vaccines are promising. They’ve worked well in treating melanoma, lung cancer, and more.
Recent trials have found:
- Improved overall survival rates
- Enhanced immune response against cancer cells
- Reduced tumor size in some patients
Manufacturing Challenges and Solutions
But making these vaccines is hard. Each one is made for a specific patient’s cancer. This requires quick and complex processes.
To solve these problems, new solutions are being developed. These include:
- Automated manufacturing systems
- Advanced mRNA synthesis techniques
- Streamlined quality control processes
These advancements are key to making these vaccines more available and effective for patients everywhere.
Treatment Delivery Innovations: 7-Minute Injections
New ways to give treatments faster and better are changing how we fight cancer. These new methods are key to making care better for patients.
Subcutaneous vs. Intravenous Administration
Now, we’re moving from old ways like IVs to subcutaneous injections. This means putting medicine under the skin, not in the veins. It’s faster and getting more popular.
7-minute injections are a big deal for cancer patients. They make getting medicine quicker, so patients spend less time in treatment.
Patient Quality of Life Improvements
These new ways help patients live better lives. They spend less time in treatment, which means more time for everything else. Plus, subcutaneous injections might be less scary than IVs.
Patients feel many things when they’re getting treatment. Quick treatments make their experience better. One patient said, “Getting my treatment in just a few minutes lets me get back to my routine faster.”
Healthcare System Efficiency Benefits
These new methods also help healthcare systems. They make treatment smoother, which can save money and make care better.
Using subcutaneous injections, like 7-minute shots, makes healthcare more sustainable. This is key as more people need cancer treatment.
In short, new ways to give treatments are changing cancer care. They make life better for patients and help healthcare systems work better. These changes are important for the future of cancer treatment.
Access and Cost Considerations for New Therapies
Exploring new cancer treatments brings up big challenges. The high cost and complex healthcare systems worldwide block many patients’ access. It’s vital to tackle these issues.
“The cost of cancer care is becoming unsustainable,” notes a recent report by a leading healthcare research organization.
“New therapies, while life-saving, are pushing the boundaries of what healthcare systems can afford.”
Insurance Coverage Challenges
Insurance coverage is a big hurdle for new cancer therapies. Insurance providers often can’t keep up with new treatments. This leads to delays or denials of coverage. We face several challenges:
- Lack of clear guidelines for new therapies
- Variability in coverage policies across different providers
- High out-of-pocket costs for patients, even with insurance
Patient assistance programs help patients with financial barriers. These programs, often from pharmaceutical companies, can greatly reduce costs.
Patient Assistance Programs
Patient assistance programs offer different kinds of support. They include:
- Financial assistance for copays and deductibles
- Free or discounted medication for eligible patients
- Resources for navigating insurance complexities
For example, a major pharmaceutical company now offers free medication to uninsured patients. They are undergoing treatment with their new cancer therapy.
Global Disparities in Treatment Access
New cancer therapies are not available equally worldwide. Global disparities in healthcare infrastructure, insurance systems, and economic conditions cause unequal access. This is a big issue.
To fix these disparities, we need many solutions. These include:
- Improving healthcare infrastructure in underserved regions
- Developing more equitable pricing strategies for new therapies
- Enhancing international collaboration in cancer research and treatment
By tackling these challenges, we can ensure more equal access to life-saving cancer therapies. This is for patients all over the world.
The Future of Cancer Care: Beyond 2025
Looking ahead to 2025 and beyond, cancer care will see big changes. New technologies will make treatments better and life easier for patients.
Emerging Technologies on the Horizon
New tech like artificial intelligence (AI) will change cancer care. AI can make treatment plans more personal and help doctors find cancer sooner.
Liquid biopsies are another big step. They let doctors check for cancer without surgery. This could change how we find and track cancer.
Artificial Intelligence in Treatment Selection
AI is helping doctors make better choices. It looks at lots of data to find patterns. This helps doctors pick the best treatments for each patient.
Using AI for treatment plans could lead to better results. It ensures treatments match each patient’s cancer perfectly.
Liquid Biopsies and Early Detection
Liquid biopsies are a big leap in finding and tracking cancer. They check for cancer DNA in the blood. This lets doctors find cancer early and see how treatments are working.
This tech could lead to better care. It means doctors can act sooner, and treatments can be more effective.
The future of cancer care looks bright with these new tools. By using the latest tech, we can make care better and life easier for cancer patients.
Conclusion: Transforming Cancer from Fatal to Chronic Disease
We are seeing a big change in how we treat cancer. New treatments are coming out, changing the way we fight cancer. These new ways are giving patients hope and better lives.
The American Association for Cancer Research’s Cancer Progress Report shows us the big steps forward in cancer treatment. New medicines and tools are helping us fight cancer better. This is moving us towards a future where cancer is managed like a chronic disease.
By supporting and advancing cancer research, we can make a difference. We can see more stories of people beating cancer. The work being done now is just the start of something big, promising better lives for all.
FAQ
What is the latest breakthrough in cancer treatment?
Cancer treatment is getting better fast. We now have immunotherapies, targeted therapies, and new ways to deliver treatments. These include antibody-drug conjugates and CAR T-cell therapy.
How does immunotherapy work in cancer treatment?
Immunotherapy uses your body’s immune system to fight cancer. It removes the brakes on your immune system. This lets it find and attack cancer cells better.
What are antibody-drug conjugates (ADCs) and how do they work?
ADCs are special cancer treatments. They use antibodies to find cancer cells and then deliver chemotherapy. This targets cancer cells while protecting healthy ones.
What is CAR T-cell therapy, and how is it used in cancer treatment?
CAR T-cell therapy makes your T-cells attack cancer. It’s a new way to treat some blood cancers and might work for others, too.
Are there any new cancer drugs or treatments available?
Yes, many new cancer drugs and treatments are being developed. These include immunotherapies, targeted therapies, and combinations. They offer hope to patients all over the world.
How do I access new and innovative cancer treatments?
Getting new cancer treatments can be hard. It’s because of insurance and unequal access worldwide. But, patient assistance programs and clinical trials can help.
What is the role of artificial intelligence in cancer treatment?
Artificial intelligence is becoming important in cancer treatment. It helps choose treatments, diagnose, and improve patient outcomes. It does this by analyzing data and finding patterns.
Can cancer be cured with the latest treatments?
Cancer is a complex disease, but new treatments are promising. They could make cancer more manageable and improve outcomes.
What are the benefits of subcutaneous administration of cancer treatments?
Subcutaneous treatments, like quick injections, can make life better for patients. They reduce treatment time and might lessen side effects. This also makes healthcare more efficient.
How do personalized cancer vaccines work?
Personalized cancer vaccines use mRNA and neoantigens. They create a unique immunity against tumors. This is a new and promising area in cancer treatment.
References
- Schubert, M. L., & Baroudjian, B. A. (2025). Personalized cancer vaccines:








