Optic disc edema is a serious eye problem. It happens when the nerve layer at the optic nerve head swells. This issue needs quick medical help because it can mean serious brain problems or losing your sight. What is optic disc oedema? This essential guide explains the 5 most dangerous causes, key signs, and when to seek urgent help.
Papilledema is a type of disc edema caused by high pressure in the brain. Knowing the signs of optic disc edema is key to getting the right treatment fast.
At Liv Hospital, we focus on our patients. We make sure you get the right diagnosis and support, no matter where you’re from.
Key Takeaways
- Optic disc edema is a serious neuro-ophthalmic condition requiring immediate attention.
- It is characterized by swelling of the nerve fiber layer at the optic nerve head.
- Papilledema is a specific type of disc edema caused by elevated intracranial pressure.
- Recognizing the signs of optic disc edema is critical for timely diagnosis and treatment.
- Liv Hospital offers detailed neuro-ophthalmologic care with a focus on the patient.
What Is Optic Disc Edema?

Optic disc edema is when the optic disc swells. This swelling can happen for many reasons, like high pressure inside the skull.
Definition and Critical Importance
Optic disc edema is when the optic disc, where the optic nerve fibers leave the eye, swells. It can be caused by idiopathic intracranial hypertension (IIH), which is now seen as the main cause, according to 2025 research.
This condition is very serious because it can mean there’s a bigger problem that could harm your vision or even your life. So, finding and treating it quickly is very important.
Nerve Fiber Layer Swelling at the Optic Nerve Head
The swelling of the nerve fibers at the optic nerve head is a key sign of optic disc edema. This happens when fluid builds up in the nerve fibers because they can’t move it properly.
This swelling can make the optic disc look different, like it’s blurred or raised. Knowing why this happens helps doctors diagnose and treat optic disc edema better.
Causes of Optic Disc Edema | Prevalence | Clinical Significance |
Idiopathic Intracranial Hypertension (IIH) | 53.7% | Primary cause, often associated with vision loss if not managed properly. |
Nonarteritic Anterior Ischemic Optic Neuropathy | 17.4% | Critical to differentiate from other causes to provide appropriate management. |
Non-IIH Papilledema | 10.9% | Requires thorough investigation to identify underlying causes. |
Anatomy and Physiology of the Optic Disc

To diagnose optic disc edema correctly, knowing the optic disc’s anatomy and functions is key. The optic disc is vital for our vision. It’s made of retinal ganglion cell axons and glial cells, covered by three meningeal layers.
Normal Optic Disc Appearance
The optic disc looks a certain way when it’s healthy. It’s a pinkish structure with a clear center. Its edges are sharp, and it looks the same in both eyes.
Vascular Supply and Drainage
The optic disc gets its blood from the posterior ciliary arteries and the central retinal artery. The veins drain through the central retinal vein. Knowing this is important because problems like optic disc hyperemia can mean something’s wrong.
Axonal Transport Mechanisms
Keeping the optic nerve healthy is all about axonal transport. This process moves important stuff to and from the retina. If it breaks down, you might see a swelling optic disc.
Aspect | Normal Characteristics | Clinical Significance |
Disc Margins | Sharp and well-defined | Blurred margins may indicate edema |
Color | Pinkish | Hyperemia or pallor can signify pathology |
Cup-to-Disc Ratio | Typically symmetric between eyes | Asymmetry can indicate glaucoma or other conditions |
Vascular Supply | Posterior ciliary arteries and central retinal artery | Understanding supply helps in diagnosing vascular-related conditions |
Recognizing Optic Disc Edema: Key Diagnostic Features
To spot optic disc edema, you need to know its main signs. This swelling of the optic disc shows clear signs that doctors look for to diagnose it correctly.
Blurred Optic Disc Margins
One key sign is when the optic disc margins get blurry. Normally, the optic disc has clear edges. But with edema, these edges get fuzzy because of swelling.
Disc Hyperemia and Hyperemic Appearance
Another important sign is disc hyperemia. This means the optic disc looks redder than usual. It happens because blood vessels at the optic nerve head get more blood, making it look flushed.
Venous Congestion and Dilation
Venous congestion and dilation are also signs. The veins look bigger and twisted. This shows there’s more pressure in the veins.
Peripapillary Hemorrhages
Peripapillary hemorrhages are bleeding around the optic disc. They happen when the disc swells a lot. These hemorrhages might mean there’s a serious problem.
Papilledema often shows up on both sides but can look different. Sometimes, it only shows up on one side. Seeing these signs means you should look into why the optic disc is swollen.
Diagnostic Feature | Description | Clinical Significance |
Blurred Optic Disc Margins | Obscuring of the normal optic disc borders | Indicates swelling of the nerve fiber layer |
Disc Hyperemia | Increased redness of the optic disc | Suggests congestion of blood vessels |
Venous Congestion and Dilation | Engorgement and tortuosity of veins | Indicates increased venous pressure |
Peripapillary Hemorrhages | Bleeding around the optic disc | May indicate severe underlying condition |
Clinical Presentation and Patient Symptoms
Patients with optic disc edema may show different symptoms. These can range from visual problems to headaches. It’s important for doctors to know about these symptoms.
Visual Disturbances
Visual problems are common in optic disc edema. These include:
- Blurred vision
- Transient visual obscurations
- Visual field defects
Patients might see things blur or dim for a short time. This can happen when they change their position. It’s key to catch these signs early to avoid lasting eye damage.
Headaches and Associated Neurological Symptoms
Headaches are a big issue for those with optic disc edema. They often get worse in the morning or when lying down. Other symptoms can be:
- Pulsatile tinnitus
- Nausea and vomiting
- Diplopia (double vision)
These symptoms can mean there’s too much pressure inside the skull. This needs quick checking.
Asymptomatic Presentations
Some people with optic disc edema don’t show any symptoms at first. They might only find out through an eye check-up. Regular eye exams are key to spotting changes and managing the condition.
Knowing about the different symptoms of optic disc edema helps doctors make better diagnoses. They can then create the right treatment plans.
Primary Causes of Optic Disc Edema
Optic disc edema has many causes, but Idiopathic Intracranial Hypertension is the main one in most cases. Knowing the main causes helps doctors diagnose and treat it better.
Idiopathic Intracranial Hypertension (53.7% of Cases)
Idiopathic Intracranial Hypertension (IIH) is the top reason for optic disc edema, making up about 53.7% of cases. It’s when the pressure inside the skull goes up without a clear reason. People with IIH often have headaches and vision problems.
IIH mostly affects women who are of childbearing age and are overweight. If not treated, it can cause serious vision loss. It’s important to catch and treat it early to avoid lasting vision damage.
Demographic Characteristics | Clinical Implications |
Women of childbearing age | Higher risk of IIH |
Obesity | Increased intracranial pressure |
Headaches and visual disturbances | Common presenting symptoms |
Nonarteritic Anterior Ischemic Optic Neuropathy (17.4% of Cases)
Nonarteritic Anterior Ischemic Optic Neuropathy (NAION) is another big reason for optic disc edema, making up about 17.4% of cases. NAION usually happens in older people. It’s linked to high blood pressure, diabetes, and high cholesterol.
NAION happens when the optic nerve head doesn’t get enough blood, causing sudden vision loss. It’s key to manage risk factors quickly to stop vision from getting worse.
Non-IIH Papilledema (10.9% of Cases)
Non-IIH papilledema makes up about 10.9% of optic disc edema cases. This includes swelling of the optic disc due to other reasons like tumors or blood clots in the brain.
Finding out the real cause is important for the right treatment. A detailed check-up is needed to find the cause and plan the treatment.
By knowing the main causes of optic disc edema, like IIH, NAION, and non-IIH papilledema, we can better help patients. This leads to better health outcomes.
Secondary Causes of Optic Disc Edema
Many secondary factors can cause optic disc edema. It’s important to understand these causes to treat the condition properly. A detailed diagnosis is key.
Intracranial Masses and Space-Occupying Lesions
Intracranial masses and lesions can raise intracranial pressure. This leads to edema of the optic disc. These masses, like tumors or abscesses, take up space in the skull. They can block or compress the cerebrospinal fluid (CSF) pathways.
Cerebral Venous Thrombosis
Cerebral venous thrombosis (CVT) is another major cause of optic disc edema. CVT forms blood clots in the cerebral venous sinuses. This can increase intracranial pressure by blocking CSF absorption. Symptoms include headaches, seizures, and vision problems.
Inflammatory and Infectious Processes
Inflammatory and infectious diseases can also cause optic disc margin blurring and edema. Meningitis, encephalitis, and neurosarcoidosis are examples. These conditions can lead to inflammation affecting the optic nerve. It’s important to treat the underlying cause.
Medication-Induced Optic Disc Edema
Some medications can lead to optic disc hyperemia and edema. Antibiotics, corticosteroids, and other drugs can change the optic disc’s appearance. It’s critical for doctors to recognize these causes. This helps in managing the condition by adjusting or stopping the medication.
It’s essential for healthcare providers to understand the secondary causes of optic disc edema. A thorough evaluation, including imaging and clinical assessment, is needed. This helps identify the cause and develop an effective treatment plan.
Diagnostic Approaches and Imaging Techniques
Diagnosing optic disc edema needs a mix of old and new methods. We’ll look at the tools and techniques used to spot and treat this condition.
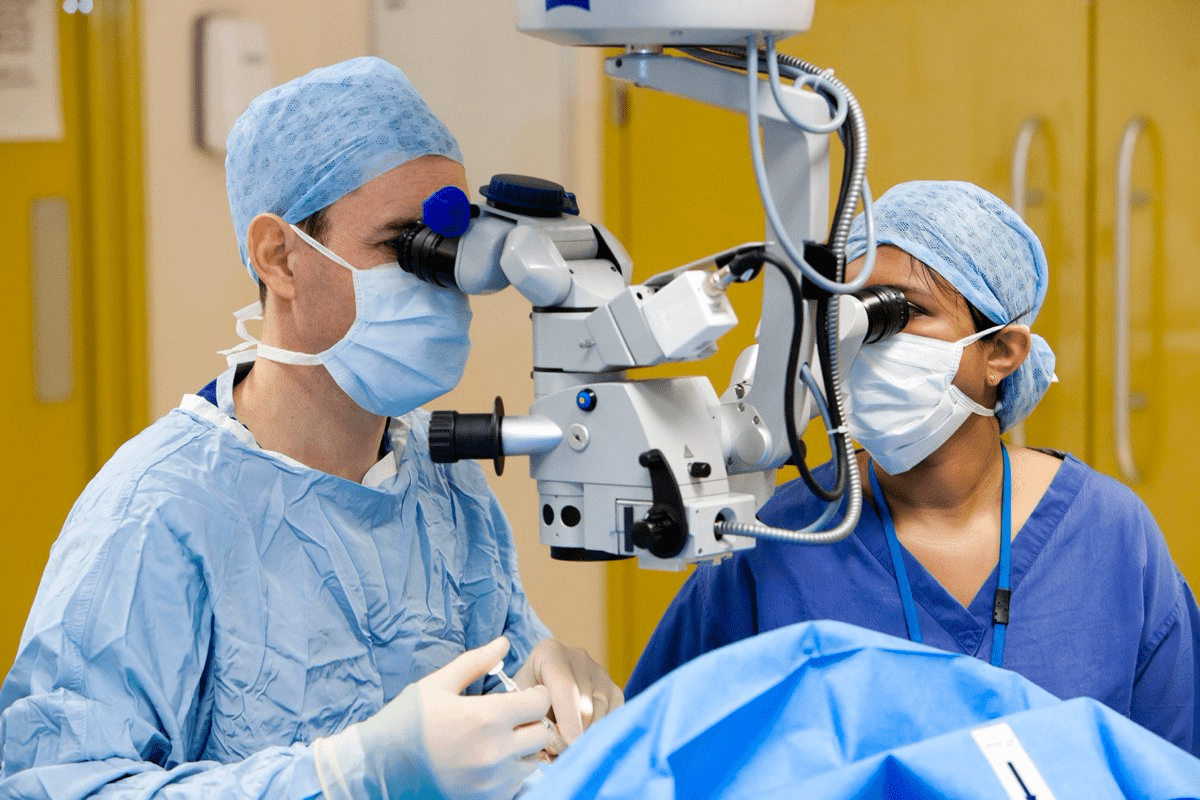
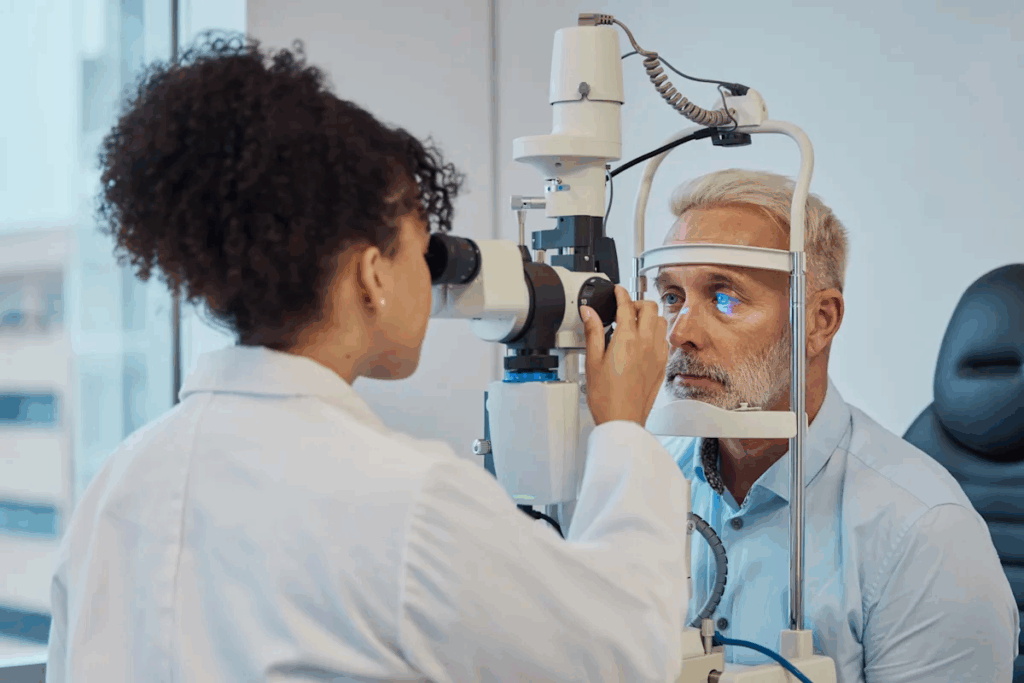
Ophthalmoscopic Examination
The first step in diagnosing optic disc edema is an ophthalmoscopic exam. This method lets doctors see the optic disc and retina. They look for signs like blurry edges, redness, and vein swelling.
Direct ophthalmoscopy gives a close-up view. Indirect ophthalmoscopy shows more, helping find other eye problems.
Optical Coherence Tomography (OCT)
Optical Coherence Tomography (OCT) has changed how we diagnose optic disc edema. It takes detailed pictures of the optic disc and retina. This helps measure swelling and spot small changes.
We use OCT to check the thickness of the nerve layer and watch the optic disc. This is key for managing optic disc edema.
Neuroimaging Considerations
Neuroimaging is important for diagnosing optic disc edema, mainly when there’s a brain issue. Magnetic Resonance Imaging (MRI) and Computed Tomography (CT) scans check the brain and eyes. We suggest these scans when the cause is unclear or if there are brain symptoms.
Lumbar Puncture and CSF Analysis
In some cases, a lumbar puncture and CSF analysis are needed. They help find conditions like idiopathic intracranial hypertension, a common cause. The CSF test measures pressure and checks for infection or inflammation.
We do lumbar punctures safely and accurately. This helps us diagnose and treat optic disc edema properly.
By using these methods together, we can accurately diagnose and manage optic disc edema. This helps address the root cause and prevent future problems.
Differential Diagnosis: Conditions That Mimic Optic Disc Edema
Diagnosing optic disc edema correctly means knowing the difference from other similar-looking conditions. Several conditions can look like optic disc edema. This makes it important to diagnose them correctly for the right treatment.
Pseudopapilledema
Pseudopapilledema looks like optic disc swelling but isn’t really swollen. It can happen due to birth defects or optic disc drusen. Unlike true optic disc edema, it doesn’t usually affect vision much.
Optic Nerve Drusen
Optic nerve drusen are hard deposits in the optic nerve head. They make the optic disc look swollen, like optic disc edema. These drusen often make the optic disc look bumpy and may change the retina nearby.
Myelinated Nerve Fibers
Myelinated nerve fibers can make the optic disc look swollen. This is because of the myelin sheaths in front of the lamina cribrosa. It’s usually harmless and can be told apart from true optic disc edema by its unique edge appearance.
Small Crowded Discs
Small crowded discs can look like optic disc edema because they appear elevated. They often have a small optic cup and can be normal. OCT can help tell them apart from true edema.
In summary, telling optic disc edema apart from look-alike conditions needs a thorough eye exam. This includes talking to the patient, checking their vision, and using OCT. Knowing these differences is key for the right diagnosis and treatment.
Clinical Management and Urgency Assessment
Managing optic disc edema well means acting fast to avoid permanent vision loss. We need to know the cause, watch for urgent signs, and keep an eye on how it changes. This helps prevent serious problems.
Red Flags Requiring Immediate Intervention
Some signs of swollen optic disc need quick action. Look out for severe vision problems, sudden blindness, and signs of high pressure inside the skull. It’s important to see a specialist right away to avoid lasting damage.
“The presence of severe headache, nausea, and vomiting in conjunction with optic disc edema may indicate raised intracranial pressure, necessitating urgent evaluation and management.”
Referral Guidelines
Seeing an eye doctor or neurologist is a good idea if you have optic disc swelling. How fast you need to see them depends on how bad the symptoms are. A full eye check and scans are usually needed to find out why it’s happening.
Clinical Feature | Urgency Level | Recommended Action |
Severe Visual Loss | High | Immediate Referral |
Mild Visual Disturbances | Moderate | Urgent Referral within 1-2 weeks |
Asymptomatic | Low | Routine Referral within 4-6 weeks |
Monitoring Progression and Resolution
Keeping an eye on things is key to see if treatment is working. Optical Coherence Tomography (OCT) is a great tool. It lets us check the thickness of the nerve layer in the retina.
Preventing Vision Loss and Neurological Complications
Treatment aims to fix the cause of high pressure. For some, losing weight and certain medicines might help. Quick and right treatment can really lower the chance of lasting vision loss and brain problems.
- Identify and manage underlying causes
- Monitor for signs of increased intracranial pressure
- Implement appropriate therapeutic measures
- Regular follow-up to assess treatment response
By being thorough and proactive in managing optic disc edema, we can make sure patients do better and avoid long-term vision problems.
Conclusion
Optic disc edema is a serious issue that needs quick action to avoid vision loss and brain problems. We talked about how important it is to know about the optic disc’s structure and function. We also discussed how to spot the signs and find the main reasons for this condition.
Papilledema, a type of disc edema, is a big worry. It’s often linked to a condition called idiopathic intracranial hypertension and other serious issues. It’s key to catch it early with eye exams, Optical Coherence Tomography (OCT), and brain scans.
Healthcare providers must know the warning signs that mean a patient needs help right away. By understanding the causes, how to diagnose, and how to treat optic disc edema, we can help patients better. This helps prevent lasting damage to their vision and brain.
Handling disc oedema well means watching how it changes and fixing the root problems. We need to stay careful in checking and treating optic disc edema. This way, we can give our patients the best care possible.
FAQ
What is optic disc edema?
Optic disc edema is when the optic disc swells. This is the spot on the retina where optic nerve fibers leave the eye. It can happen due to high pressure inside the skull, inflammation, or lack of blood flow.
What are the symptoms of optic disc edema?
Symptoms include blurry vision, double vision, or losing side vision. Some people might also get headaches or other brain-related symptoms. But, some might not notice anything wrong.
What causes optic disc edema?
It can be caused by many things. This includes high pressure in the brain, inflammation, or not enough blood flow. It can also be caused by tumors, blood clots, infections, or some medicines.
How is optic disc edema diagnosed?
Doctors use eye exams, like ophthalmoscopy and OCT, to check for it. They might also do MRI or CT scans. Sometimes, they’ll take a sample of spinal fluid for more information.
What is the difference between optic disc edema and papilledema?
Papilledema is swelling of the optic disc due to high brain pressure. Optic disc edema can be caused by many things, not just brain pressure.
Can optic disc edema be treated?
Treatment depends on the cause. It might involve lowering brain pressure or managing symptoms. Quick action is key to avoid losing vision or facing brain problems.
What is the significance of hyperemic optic disc in optic disc edema?
A hyperemic optic disc means there’s more blood flow and congestion. It’s a sign of optic disc edema. It can show there’s inflammation or high brain pressure.
How does optic disc edema affect vision?
It can cause blurry vision, double vision, or losing side vision. If not treated, it can lead to permanent vision loss.
Can optic disc edema be asymptomatic?
Yes, some people might not notice any symptoms. Regular eye checks are important to catch it early.
What are the red flags for immediate intervention in optic disc edema?
Look out for severe vision loss, quick symptom worsening, and signs of high brain pressure. These include headaches, nausea, and vomiting. Quick medical help is needed in these cases.
References
National Center for Biotechnology Information. Evidence-Based Medical Guidance. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10332214/