Last Updated on December 2, 2025 by Bilal Hasdemir

In 2020, nearly 252,000 bariatric surgeries were done in the U.S. This shows how popular weight-loss surgeries have become. Bariatric surgery changes the digestive system to help with weight loss Organs Involved in Bariatric Surgery.
Many wonder: what organ is taken out? The answer depends on the bariatric surgery type. For example, a gastric sleeve removes a big part of the stomach.
The changes from bariatric surgery can greatly affect weight loss. It’s important to know the details of each surgery for those thinking about it.
Key Takeaways
- Bariatric surgery includes many procedures, like gastric sleeve.
- The gastric sleeve removes a big part of the stomach.
- Each bariatric surgery changes the digestive system differently.
- Knowing the details of each surgery is key for those considering it.
- Bariatric surgery is a big step in losing weight.
Understanding Bariatric Surgery: A Complete Overview
Learning about bariatric surgery is key for those thinking about weight loss surgery. It involves various surgical methods to help people lose a lot of weight and improve their health.
The Purpose of Weight Loss Surgery
The main aim of bariatric surgery is to help people lose weight when other ways have not worked. This is for those with a BMI of 40 or more, or a BMI of 35 with health problems linked to obesity.
By changing the digestive system, surgery limits how much food you can eat or absorb. This leads to weight loss. It can also help with conditions like type 2 diabetes and high blood pressure.
Common Misconceptions About Organ Removal
Many think bariatric surgery means removing organs. But, while some surgeries do remove or reroute parts of the digestive system, the main goal is not organ removal. It’s to change how the digestive system works.
Surgical Technique | Organ Involved | Modification Made |
Gastric Sleeve | Stomach | Partial removal of the stomach |
Gastric Bypass | Stomach and Intestine | Rerouting of the digestive tract |
Adjustable Gastric Band | Stomach | Placement of a band around the upper stomach |
It’s important to know that different surgical techniques exist, each with its own benefits and risks. Talking to a healthcare expert is vital to find the best surgery for your health needs.
Organs Involved in Bariatric Surgery
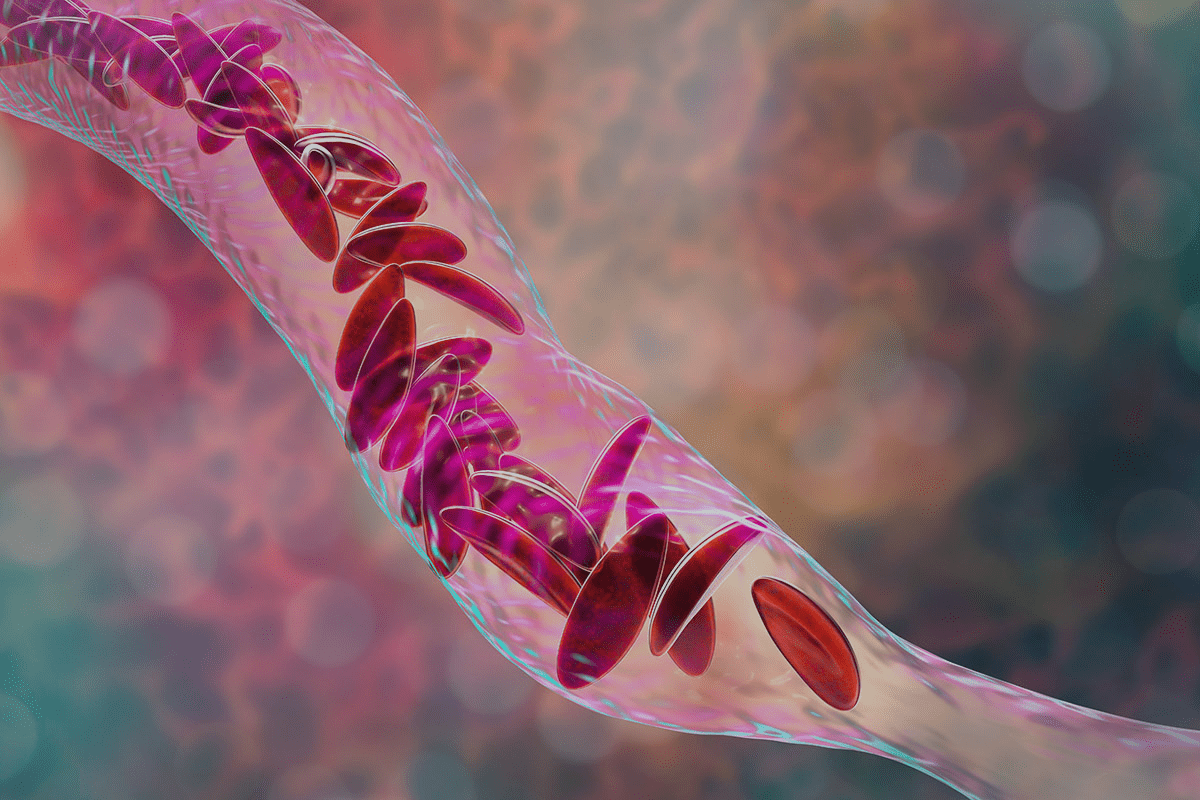
It’s important to know which organs are involved in bariatric surgery. This surgery changes the shape of key digestive organs to help with weight loss.
Primary Digestive Organs Affected
The stomach and intestines are mainly affected by bariatric surgery. The stomach is often made smaller to limit how much food you can eat. In surgeries like gastric sleeve, a big part of the stomach is removed, leaving a narrow stomach.
In gastric bypass surgery, a small pouch is made at the stomach’s top. It’s then connected directly to the small intestine.
The intestines, mainly the small intestine, are key in bariatric surgery. This is true for surgeries like gastric bypass and biliopancreatic diversion. These surgeries change the small intestine’s path, affecting how nutrients are absorbed.
Organs That Remain Untouched
While the stomach and intestines are changed, the liver and gallbladder are usually not. But, they can be affected indirectly. For example, changes in bile flow and digestive enzymes can impact the gallbladder.
Even if some organs aren’t directly changed, the impact on the digestive system is big. It’s key for patients to understand these changes to take care of their health after surgery.
Gastric Sleeve Surgery: Partial Stomach Reduction
Gastric sleeve surgery makes the stomach very narrow. This helps patients lose a lot of weight. The surgery removes a big part of the stomach, leaving a thin tube-like stomach.
The Procedure Explained
The surgery is done through small cuts in the belly. A big part of the stomach is taken out. This makes the stomach very small, so you feel full quickly.
The whole surgery takes about 60 to 90 minutes. Most people go home the same day or after a short stay in the hospital.
How Much of the Stomach Is Removed
About 75% to 80% of the stomach is removed. This can change based on the patient and the surgeon. The stomach left is like a banana or a narrow tube.
Aspect | Details |
Portion of Stomach Removed | 75% to 80% |
Remaining Stomach Size | About the size of a banana |
Surgery Duration | 60 to 90 minutes |
Long-term Anatomical Changes
The stomach sleeve can stretch a bit over time. But it stays much smaller than before. This long-term change helps keep weight off by limiting how much you can eat. It also changes hunger hormones, helping with weight control.
Patients must stick to a strict diet after surgery. They also need to go to follow-up appointments. This helps track progress and solve any problems.
Gastric Bypass: Creating a Stomach Pouch
The Roux-en-Y gastric bypass is a complex surgery. It makes a small stomach pouch and changes the intestines to help with weight loss.
Roux-en-Y Technique Explained
The Roux-en-Y gastric bypass makes a small pouch from the stomach. It connects this pouch to the small intestine. This method was first described by French surgeon César Roux.
Key Steps in Roux-en-Y Gastric Bypass:
- Creation of a small stomach pouch
- Division of the small intestine
- Attachment of the intestinal limbs to the stomach pouch
Stomach and Intestinal Modifications
Gastric bypass surgery changes the stomach and intestines a lot. The stomach is made smaller, which limits how much food you can eat. The intestines are also changed, affecting how nutrients are absorbed.
Modification | Description | Effect |
Stomach Pouch Creation | Reducing the stomach to a small pouch | Reduces food intake capacity |
Intestinal Rerouting | Connecting the stomach pouch directly to the small intestine | Alters nutrient absorption pathway |
Digestive Pathway Changes
The gastric bypass changes how food is digested and nutrients are absorbed. This can lead to a lot of weight loss and better health for people with obesity.
“Gastric bypass surgery has been shown to be an effective treatment for obesity, leading to substantial weight loss and improvement in comorbidities.” –
American Society for Metabolic and Bariatric Surgery
Understanding the changes made in gastric bypass surgery helps patients see its benefits and risks.
Biliopancreatic Diversion: Intestinal Rerouting
This surgery changes how the body absorbs nutrients by rerouting the intestines. This helps in losing weight.
The Surgical Approach
The surgery has two parts: sleeve gastrectomy and intestinal rerouting. First, a big part of the stomach is removed, leaving a narrow tube.
Then, the small intestine is split and rearranged. This makes it harder for the body to absorb calories and nutrients.
Impact on Digestive Organs
This surgery changes the digestive system a lot. The smaller stomach means less food can be eaten. The intestines process food differently too.
This change affects how bile and digestive enzymes work in the body.
Nutritional Absorption Changes
The main goal is to reduce how much the body absorbs. This is done by shortening the intestine’s length for absorption.
Nutritional Aspect | Pre-Surgery | Post-Surgery |
Caloric Absorption | Normal absorption | Reduced absorption |
Nutrient Uptake | Optimal nutrient uptake | Altered nutrient uptake |
Vitamin and Mineral Absorption | Normal absorption | May require supplementation |
People who have this surgery need to watch for nutritional deficiencies. They should talk to their doctor about diet and supplements.
Adjustable Gastric Band: Non-Removal Approach
The adjustable gastric band is a popular choice. It’s reversible and less invasive than other surgeries.
How the Band Works
A silicone band is placed around the upper stomach. This creates a small pouch to limit food intake. The band is connected to a port under the skin for adjustments.
Key benefits include its reversibility and adjustable tightness. This offers a tailored approach to weight loss.
Stomach Function With a Band
The stomach’s upper pouch is restricted after the band is placed. This limits food intake. Yet, the stomach digests food normally.
The band reduces hunger and increases fullness. This helps with weight loss.
Reversibility Factors
The adjustable gastric band is reversible. It can be adjusted or removed if needed. This makes it less permanent than other surgeries.
Procedure | Reversibility | Adjustment Capability |
Adjustable Gastric Band | Yes | Yes |
Gastric Sleeve | No | No |
Gastric Bypass | In some cases | No |
The table shows the adjustable gastric band’s unique benefits. It’s reversible and adjustable, making it a good choice for bariatric surgery.
“The adjustable gastric band represents a significant advancement in bariatric surgery, providing a reversible and adjustable solution for weight loss.”
A Bariatric Surgeon
The Stomach’s Role Before and After Surgery
It’s important to know how the stomach works before and after bariatric surgery. The stomach is key in our digestive system. It stores and breaks down food. After surgery, the stomach changes, affecting digestion and health.
Normal Stomach Function
The stomach is vital in our digestive system. It stores food, mixes it with digestive enzymes and acids, and slowly releases it into the small intestine. The stomach’s walls churn food, and its lining protects it from acidic juices.
“The stomach is a complex organ with multiple functions, including mechanical and chemical digestion, and its role is significantly altered after bariatric surgery.”
Adapted Function Post-Surgery
After bariatric surgery, the stomach changes. For example, in gastric sleeve surgery, a lot of the stomach is removed. This makes the stomach smaller, leading to less food intake.
In gastric bypass surgery, a small pouch is made at the stomach’s top. It’s then connected directly to the small intestine. This bypasses a big part of the stomach and upper small intestine.
- The stomach’s size is reduced, leading to less food capacity.
- The anatomy of the stomach is altered, changing how food is processed.
- The connection between the stomach and the small intestine is modified, affecting nutrient absorption.
Long-term Adaptations
Over time, the body gets used to the changes from bariatric surgery. The stomach and digestive system adjust. Patients often see changes in eating habits and digestion.
Long-term, the body might adjust how it absorbs nutrients. This can include changes in gut hormones that affect hunger and fullness.
Adaptation | Description | Impact |
Reduced Stomach Size | Less food capacity | Earlier satiety, reduced food intake |
Altered Gut Hormones | Changes in hunger and satiety signals | Reduced hunger, improved weight loss |
Changes in Nutrient Absorption | Modified digestive pathway | Potential for nutritional deficiencies if not properly managed |
In conclusion, understanding the stomach’s role before and after bariatric surgery is key. It helps patients make informed decisions about weight loss. Knowing the changes in the stomach and digestive system after surgery helps patients prepare for the lifestyle changes they’ll need to make.
Impact on the Digestive System Beyond the Stomach
Bariatric surgery changes more than just the stomach. It affects other important parts of the digestive system too. The small intestine, bile flow, digestive enzymes, and gallbladder all see big changes.
Effects on the Small Intestine
The small intestine is key for absorbing nutrients. Bariatric surgery can change how it works. For example, gastric bypass surgery reroutes food through the small intestine, bypassing parts of the stomach and duodenum.
This can alter nutrient absorption. It might lead to vitamin and mineral deficiencies. It can also change the gut’s microbiome.
Rerouting the small intestine can lead to:
- Altered nutrient absorption patterns
- Potential deficiencies in essential vitamins and minerals
- Changes in the gut microbiome due to the altered anatomy
Changes in Bile and Digestive Enzymes Flow
Bariatric surgery can also change how bile and digestive enzymes work. Bile helps digest fats and is stored in the gallbladder. Some surgeries can mess with bile release, affecting fat digestion.
A study in a Journal found changes in the gut’s anatomy can affect digestive enzymes and bile. This can impact nutrient absorption and digestive health.
“The rearrangement of the gastrointestinal tract during bariatric surgery can have profound effects on the digestive process, including changes in bile and enzyme secretion.”
The Role of the Gallbladder After Surgery
The gallbladder’s role can change after bariatric surgery. Even if it’s not removed, its function can be affected. Rapid weight loss after surgery can increase gallstone risk.
Patients should talk to their doctors about gallbladder risks. They might need to take ursodeoxycholic acid (UDCA) to prevent gallstones during weight loss.
Metabolic Changes Following Bariatric Procedures
Bariatric surgery does more than just help you lose weight. It changes your body in many ways.
Hormonal Impacts
Bariatric surgery changes your hormones a lot. It affects hunger and fullness signals. This helps patients eat better.
Changes in Hunger and Satiety
After surgery, you might feel full faster and less hungry. Hormones and surgery changes cause this. For example, a smaller stomach means you can’t eat as much.
Metabolic Benefits Beyond Weight Loss
Bariatric surgery also improves your metabolism. It makes your body better at handling sugar, reduces inflammation, and improves fats. This lowers the risk of diabetes and heart disease.
The changes after bariatric surgery are complex. Knowing about them helps doctors and patients better.
Nutritional Considerations After Organ Modification
Nutritional planning is key after bariatric surgery. The surgery changes how the body absorbs nutrients. This makes it important to plan your diet carefully after surgery.
Essential Nutrient Absorption
After bariatric surgery, the body may not absorb nutrients as well. The surgery can make it harder for the body to take in proteins, vitamins, and minerals.
Nutrients of particular concern include:
- Protein: important for muscle and overall health
- Vitamin B12: needed for nerves and red blood cells
- Iron: prevents anemia
- Calcium: keeps bones healthy
- Vitamin D: good for bones and immune system
Vitamin and Mineral Supplementation
To avoid nutritional deficiencies, taking supplements is often recommended. The kind and amount of supplements needed vary based on the surgery and individual needs.
Common supplements recommended include:
- Multivitamins: for a wide range of vitamins and minerals
- Calcium citrate: for bone health
- Vitamin B12 injections or oral supplements: to prevent deficiency
- Iron supplements: to prevent anemia
Preventing Nutritional Deficiencies
Preventing nutritional deficiencies requires a detailed plan. This includes dietary changes, supplements, and regular health check-ups. Patients should eat a diet full of nutrients and watch for signs of deficiency.
Key strategies for preventing deficiencies include:
- Eating a balanced diet full of essential nutrients
- Following the recommended supplement plan
- Having regular health check-ups to monitor nutrition
Patient Education and Surgical Consultation
Patient education is key in bariatric surgery. It helps people make smart choices about their health. Knowing what to expect can lead to better results.
Understanding Surgical Options
Bariatric surgery offers many options, each with its own benefits and risks. It’s important to know about gastric sleeve, gastric bypass, and adjustable gastric banding. This knowledge helps choose the right surgery for you.
Choosing a surgery depends on your health, BMI, and past surgeries. Talking to a bariatric surgeon is the first step to find the best option for you.
Questions to Ask Your Surgeon About Organ Modifications
When you meet with your surgeon, ask important questions. You might want to know:
- What changes will be made to my stomach or intestines?
- How will these changes affect my digestive process?
- Are there any possible complications or risks with the procedure?
- How might the surgery affect my nutrition?
These questions help you understand the surgery and its effects on your health.
Setting Realistic Expectations
It’s important to have realistic goals after surgery. Remember, weight loss surgery is a tool for long-term weight control, not a quick fix.
Pre-Surgery Expectations | Post-Surgery Reality |
Significant weight loss | Gradual weight loss over time |
Improved overall health | Potential improvements in comorbidities |
Reduced hunger and increased satiety | Changes in hunger and fullness hormones |
Understanding the surgery and its effects helps set realistic goals. This can lead to a more successful outcome.
Support Systems and Resources for Bariatric Patients
A strong support system is key for bariatric patients. They face big challenges with weight loss and lifestyle changes. This support comes from doctors, support groups, and community resources.
Medical Follow-up Requirements
After surgery, patients need regular medical check-ups. These visits help track their health and fix any problems. Medical follow-up is key to avoiding long-term health issues.
How often patients see their doctors varies. It depends on the surgery type and their health. Usually, they visit every few weeks or months to check on their progress.
Support Groups and Community Resources
Support groups are very important for bariatric patients. They share experiences, get emotional support, and learn from others. Being part of a support group boosts mental and emotional health.
There are also online forums and local groups for support. They offer tips on healthy living, diet, and coping. Patients can find these resources through hospitals, doctors, or online.
Navigating Life After Anatomical Changes
Life after bariatric surgery brings big changes. Patients must adjust to new eating habits and nutrition. These changes affect how they relate to food and their lifestyle.
Patients face challenges like nutritional deficiencies and changes in hunger. Education and support help overcome these challenges. Doctors and support groups provide guidance and resources.
Understanding the value of support systems and using available resources helps bariatric patients. They can smoothly transition to their new lifestyle and keep their weight loss.
Conclusion: Making Informed Decisions About Bariatric Surgery
Patients thinking about bariatric surgery need to do their homework. They should talk to doctors and learn about the different surgeries. This includes gastric sleeve, gastric bypass, and adjustable gastric band.
Looking into how well these surgeries work and what others say can help a lot. It gives a clear picture of what to expect. This way, people can make choices that are right for them.
Understanding bariatric surgery fully is key. It means knowing the good and bad sides. By doing research and talking to doctors, patients can make smart choices. This helps them get the best results from their surgery.
FAQ
What is bariatric surgery and how does it affect the digestive system?
Bariatric surgery is a way to lose weight by changing the digestive system. It can involve different surgeries, but most change the stomach or intestines. This limits how much food you can eat or absorb.
Which organs are typically removed or modified during bariatric surgery?
The main organ changed is the stomach. The surgery type decides how much of it is changed. Sometimes, the intestines are also altered or moved.
How much of the stomach is removed during gastric sleeve surgery?
In gastric sleeve surgery, a big part of the stomach is taken out. This leaves a narrow stomach. About 75-80% of the stomach is removed.
What are the long-term anatomical changes after gastric sleeve surgery?
After gastric sleeve surgery, the stomach is much smaller. The remaining stomach tissue adjusts. This leads to a smaller stomach, changes in digestive enzymes, and hormone levels.
How does gastric bypass surgery affect the digestive pathway?
Gastric bypass surgery, like the Roux-en-Y, makes a small stomach pouch. It also changes the intestines’ path. This reduces nutrient and calorie absorption.
What are the nutritional considerations after bariatric surgery?
After surgery, it’s important to watch what you eat to avoid deficiencies. Taking vitamins and minerals is key to staying healthy.
How does bariatric surgery impact metabolism and hunger hormones?
Bariatric surgery can change how you feel hungry or full. These changes help with weight loss and better health.
What support systems are available to bariatric patients after surgery?
Bariatric patients have many support options. These include medical care, support groups, and community help. They ensure a smooth recovery and good health.
What are the possible complications of bariatric surgery?
Bariatric surgery can have risks like infections, bleeding, and nutrient deficiencies. It’s important to know these risks and talk to your surgeon.
How can patients make informed decisions about bariatric surgery?
To make a good choice, understand your options, ask questions, and set realistic goals. Learning about outcomes and talking to others can also help.
References
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://pubmed.ncbi.nlm.nih.gov/32196159/