Orthopedics
Specialist Care for Bone, Joint, and Muscle Health
- Overview and Definition
- Symptoms and Causes
- Diagnosis and Evaluation
- Treatment and Follow-up
- Prevention and Care
Orthopedics
Specialist Care for Bone, Joint, and Muscle Health
- Overview and Definition
- Symptoms and Causes
- Diagnosis and Evaluation
- Treatment and Follow-up
- Prevention and Care
Orthopedics focuses on the musculoskeletal system. Learn about the diagnosis, treatment, and rehabilitation of bone, joint, ligament, and muscle conditions.
Overview and definition
Orthopedics, formally known as Orthopaedic Surgery, is the branch of medicine dedicated to the diagnosis, treatment, rehabilitation, and prevention of injuries and diseases of the musculoskeletal system. This complex system provides form, stability, and movement to the human body. While many people associate orthopedics primarily with broken bones, the field is far more expansive, covering a vast network of tendons, ligaments, muscles, nerves, and joints. An orthopedic surgeon or orthopedist is a medical doctor with specialized training to manage these conditions through both surgical and non-surgical means.
The Anatomy of the Musculoskeletal System

To understand orthopedics, one must understand the intricate machinery of the body that allows for motion. The musculoskeletal system is an engineering marvel composed of several distinct tissue types that must function in harmony.
- Bones: The body’s rigid framework. The adult human skeleton consists of 206 bones that protect organs, produce blood cells, and store minerals. Bones are living tissues that constantly remodel themselves.
- Joints: The connection points between bones that facilitate movement. They range from hinge joints (such as the knee and elbow) to ball-and-socket joints (such as the hip and shoulder). The ends of bones in a joint are covered by cartilage, a smooth, rubbery substance that prevents friction.
- Muscles: Contractile tissues that pull on bones to create movement.
- Ligaments: Tough bands of fibrous connective tissue that connect bone to bone, providing stability to joints (e.g., the ACL in the knee).
- Tendons: Fibrous cords that attach muscle to bone (e.g., the Achilles tendon).
- Nerves: The “wiring” system that carries signals from the brain to the muscles to initiate movement and carries sensory information (pain, touch) back to the brain.
The Scope of Orthopedic Practice

Orthopedics is a broad field that addresses conditions present from birth (congenital), those caused by injury (traumatic), and those that develop over time due to aging or wear and tear (degenerative).
The field is often divided into specialized areas of focus, allowing physicians to develop high-level expertise in specific parts of the body or types of conditions:
- Joint Reconstruction and Arthroplasty: Focuses on replacing damaged joints, particularly the hip and knee, due to arthritis.
- Sports Medicine: Deals with injuries related to physical activity, such as ligament tears, meniscus injuries, and rotator cuff problems.
- Spine Surgery: Addresses conditions affecting the vertebral column, including herniated discs, spinal stenosis, and scoliosis.
- Hand and Upper Extremity: Focuses on the complex network of small bones, tendons, and nerves in the hand, wrist, and elbow (e.g., carpal tunnel syndrome).
- Foot and Ankle: Manages issues ranging from bunions and flat feet to complex fractures and Achilles tendonitis.
- Orthopedic Trauma: Specializes in the management of severe fractures and dislocations, often resulting from accidents.
- Pediatric Orthopedics: Dedicated to treating musculoskeletal issues in growing children, such as clubfoot, hip dysplasia, and growth plate fractures.
- Musculoskeletal Oncology: A specialized field treating benign and malignant tumors of the bone and soft tissue.
The Impact of Musculoskeletal Health
Mobility is central to quality of life. Orthopedic conditions are the leading cause of disability worldwide. They can range from acute, short-term injuries like a sprained ankle to chronic, progressive diseases like osteoarthritis. The goal of orthopedic care is not just to fix a broken part, but to restore function, alleviate pain, and help patients return to their daily activities, whether that involves high-performance sports or simply walking without pain.

Symptoms and Causes
Musculoskeletal symptoms are among the most common reasons patients seek medical attention. Because the system involves so many moving parts, symptoms can present in various ways. Recognizing early warning signs is crucial for preventing minor issues from becoming chronic, debilitating conditions.
Recognizing Orthopedic Symptoms
Pain is the most universal symptom in orthopedics, but the nature of the pain and accompanying signs provide vital clues to the underlying problem.
- Pain Characteristics:
- Mechanical Pain: Pain that worsens with movement or specific activities and improves with rest. This is typical of osteoarthritis or tendonitis.
- Night Pain: Pain that disrupts sleep can be a sign of inflammatory conditions or, in rare cases, bone tumors.
- Radiating Pain: Pain that shoots from the spine down the arm or leg (sciatica) usually indicates nerve compression.
- Swelling and Inflammation: Visible puffiness, redness, or warmth around a joint suggests inflammation. This can result from acute injury (bleeding into the joint) or from chronic conditions such as arthritis or bursitis.
- Stiffness and Reduced Range of Motion: Difficulty moving a joint through its full extent. This is a hallmark of arthritis (often worse in the morning) or “frozen shoulder” (adhesive capsulitis).
- Instability or “Giving Way”: A sensation that a joint (often the knee or ankle) is buckling or cannot support weight. This strongly suggests ligament damage or laxity.
- Locking or Catching: A mechanical sensation where a joint feels like it gets stuck in one position. In the knee, this often indicates a meniscus tear or a loose fragment of bone/cartilage floating in the joint space.
- Deformity: Visible changes in the shape of a limb, such as the bowing of legs, the development of a bunion, or the unnatural angle of a limb following a fracture.
- Numbness and Tingling: Often described as “pins and needles,” these symptoms indicate nerve involvement, such as in carpal tunnel syndrome or spinal disc herniation.
- Muscle Weakness: An inability to generate normal force, which can result from muscle atrophy (wasting), tendon tears, or nerve damage.
30
Years of
Excellence
Trusted Worldwide
Book a Free Certified Online
Doctor Consultation
- Overview and Definition
- Symptoms and Causes
- Diagnosis and Evaluation
- Treatment and Follow-up
- Prevention and Care
Table of Contents
We're Here to Help.
Get in Touch.
Send us all your questions or requests, and our expert team will assist you.

Underlying Causes of Orthopedic Conditions
The causes of orthopedic disorders generally fall into three main categories: acute trauma, overuse/wear and tear, and systemic or congenital factors.
- Acute Trauma: Sudden injuries caused by external force.
- Degenerative Changes (Wear and Tear)
- Overuse and Repetitive Strain
- Congenital and Developmental Abnormalities
- Metabolic and Autoimmune Factors
Diagnosis and Staging
Accurate diagnosis in orthopedics relies on a combination of clinical skills and advanced technology. The goal is to not only identify what is wrong but also to quantify the severity, often referred to as grading or staging, to determine the most appropriate treatment pathway. At Liv Hospital, we utilize a comprehensive diagnostic approach to ensure no detail is overlooked.
The Clinical Evaluation: History and Physical Exam
The diagnostic process begins with a thorough consultation. The physician will take a detailed medical history, asking about the onset of pain, the mechanism of injury (how it happened), and what makes symptoms better or worse.
The Physical Examination is critical. The doctor will evaluate:
- Inspection: Looking for swelling, bruising, muscle wasting (atrophy), or deformity.
- Palpation: Feeling the area to pinpoint the exact location of tenderness.
- Range of Motion (ROM): Assessing how far a joint can move actively (by the patient) and passively (by the doctor).
- Stability Tests: Performing specific maneuvers to stress ligaments and check for laxity (e.g., the Lachman test for ACL tears).
- Neurological Assessment: Checking reflexes, sensation, and muscle strength to evaluate nerve function.
- Gait Analysis: Observing how a patient stands and walks to identify biomechanical issues.

Advanced Imaging Modalities
Imaging allows orthopedic specialists to “see” inside the body. Different technologies are used depending on the suspected tissue involved.
- X-Rays (Radiography): The gold standard for assessing bones. X-rays are excellent for diagnosing fractures and dislocations and for assessing the severity of arthritis (bone spurs, joint space narrowing). They are usually the first imaging test performed.
- Magnetic Resonance Imaging (MRI): This technology uses strong magnetic fields to create detailed images of soft tissues. It is the preferred method for diagnosing:
- Ligament and tendon tears (Rotator cuff, ACL).
- Meniscus injuries.
- Spinal disc herniations and spinal cord compression.
- Cartilage defects.
- Stress fractures that may not yet show up on X-rays.
- Computed Tomography (CT) Scans: CT scans provide cross-sectional X-ray images. They are crucial for assessing complex fractures (especially around joints like the pelvis or wrist) to plan surgery. They create 3D reconstructions of the bone.
- Bone Density Scan (DEXA): Specifically used to diagnose osteoporosis and assess fracture risk by measuring bone mineral density.
- Musculoskeletal Ultrasound: Used to visualize superficial tendons and muscles in real-time. It is also helpful for guiding injections.
Staging and Grading Musculoskeletal Conditions
In orthopedics, “staging” helps classify the severity of an injury or disease.
- Grading Sprains and Strains: Soft tissue injuries are typically graded on a scale of 1 to 3.
- Grade 1 (Mild): Microscopic tearing, minimal pain, no loss of stability.
- Grade 2 (Moderate): Partial tearing, moderate pain, swelling, and some loss of function/stability.
- Grade 3 (Severe): Complete rupture (tear) of the ligament or muscle, often requiring surgical repair and resulting in significant instability.
- Staging Osteoarthritis (Kellgren-Lawrence Scale): Doctors grade arthritis from Grade 0 (normal) to Grade 4 (severe).
- Grade 2: Mild osteophytes (bone spurs), possible narrowing of joint space.
- Grade 4: “Bone-on-bone” arthritis with large bone spurs and severe sclerosis (hardening) of bone ends. This stage usually necessitates joint replacement.
- Tumor Staging: For bone cancers, staging (Enneking system or TNM) involves determining the tumor type, its local extent, and whether it has spread (metastasized), which is vital for planning limb-salvage surgery.

Treatment Details

Orthopedic treatment has evolved significantly. The modern philosophy emphasizes the idea that “motion is life.” Treatment plans are designed to restore mobility as safely and quickly as possible. At Liv Hospital, we follow a ladder of care, typically starting with conservative (non-surgical) measures and reserving surgery for cases where conservative therapy fails or the injury is severe.
Non-Surgical (Conservative) Management
The majority of orthopedic conditions can be treated effectively without surgery.
- Immobilization: Casts, splints, braces, or slings are used to hold a bone or joint in place to allow it to heal properly (e.g., for fractures or severe sprains).
- Medication Management: Use of NSAIDs (non-steroidal anti-inflammatory drugs) to reduce pain and swelling. In some cases, muscle relaxants or neuropathic pain medications are prescribed.
- Physical Therapy and Rehabilitation: This is perhaps the most critical aspect of non-surgical care. Specific exercises strengthen the muscles around a joint, improve flexibility, and correct biomechanical faults to relieve pain and prevent recurrence.
- Injection Therapies (Orthobiologics):
- Corticosteroids: Potent anti-inflammatory injections delivered directly into a joint or around a tendon to reduce acute pain and swelling.
- Viscosupplementation (Hyaluronic Acid): Injections of a gel-like substance into the knee to lubricate the joint and cushion it, providing relief for mild to moderate arthritis.
- Platelet-Rich Plasma (PRP): A regenerative therapy where the patient’s own blood is spun down to concentrate platelets, which are then injected into the injured tissue to stimulate healing.
Surgical Interventions
When surgery is necessary, the goal is to be as minimally invasive as possible to speed up recovery.
- Arthroscopy (Keyhole Surgery): This minimally invasive technique is used to diagnose and treat joint problems. A camera (arthroscope) is inserted through a tiny incision.
- Fracture Fixation: For broken bones that cannot heal in a cast, surgery is needed to stabilize them.
- Osteotomy: Cutting and reshaping a bone to shift weight away from a damaged part of a joint, often done in younger patients with arthritis to delay the need for joint replacement.
- Spinal Surgery: Procedures include discectomy, laminectomy, and spinal fusion.
Joint Replacement Surgery (Arthroplasty)
For end-stage arthritis where the joint cartilage is completely worn away, joint replacement is the gold standard treatment.
- Total Hip Replacement (THR): Replacing the ball and socket of the hip joint with metal, ceramic, and specialized plastic components.
- Total Knee Replacement (TKR): Resurfacing the ends of the femur and tibia.
- Shoulder and Ankle Replacement: Similar procedures adapted for the specific biomechanics of these joints.
- Revision Surgery: Replacing an old artificial joint that has worn out or loosened over time.
The Medical Center

When facing musculoskeletal issues, the choice of a medical center determines not just the success of a surgery but the quality of the entire recovery journey. Liv Hospital stands as a leader in orthopedic excellence, combining the precision of robotic technology with the artistry of experienced surgical teams. We offer a holistic environment where surgeons, physiotherapists, and pain specialists work together to help you get back to the life you love.
Why Choose Liv Hospital for Orthopedic Care?
Our Orthopedics and Traumatology department is designed to handle the full spectrum of musculoskeletal health, from high-performance sports injuries to complex degenerative diseases.
- Sub-Specialized Expertise: We do not believe in a “one size fits all” approach. Our department is divided into specialized units: Spine, Hand, Foot & Ankle, Arthroplasty, and Sports Medicine. This means if you have a knee problem, you are treated by a surgeon who dedicates their career specifically to the knee.
- Robotic-Assisted Surgery: Liv Hospital is at the forefront of robotic-assisted joint replacement. We use advanced robotic-arm-assisted systems (such as MAKO or similar technologies) for total knee and hip replacements.
- Precision: The robot assists the surgeon in preparing the bone with sub-millimeter accuracy.
- Personalization: The implant positioning is tailored to each patient’s unique anatomy using 3D CT scans.
- Preservation: Greater protection of surrounding soft tissues, leading to less pain and faster recovery.
Comprehensive Sports Medicine and Rehabilitation
We understand that surgery is only half the battle. Our approach integrates rehabilitation into the treatment plan from day one.
- Integrated Physical Therapy: Our surgeons work directly with our physiotherapy team to design custom rehab protocols. This seamless communication prevents care gaps and ensures safe progression.
- Return-to-Sport Protocols: For athletes, we offer specialized testing and training to ensure they are physically ready to return to competition, reducing the risk of re-injury.
- Multidisciplinary Spine Center: Our spine unit brings together neurosurgeons, orthopedic spine surgeons, and physical medicine specialists to offer a complete range of options, emphasizing non-surgical management whenever possible.
Patient-Centric Surgical Journey
At Liv Hospital, we prioritize the patient experience.
- Rapid Recovery Protocols: We utilize modern anesthesia techniques and minimally invasive approaches to mobilize patients as soon as possible after surgery, often on the same day. This reduces complications like blood clots and accelerates healing.
- Global Standards: Our facility adheres to international safety and hygiene standards, minimizing infection risks and ensuring the highest-quality implant materials are used.
Whether you are an elite athlete dealing with a ligament tear or a senior seeking relief from arthritis pain, Liv Hospital provides the expertise, technology, and compassionate care required to restore your movement and your freedom.
- Overview and Definition
- Symptoms and Causes
- Diagnosis and Evaluation
- Treatment and Follow-up
- Prevention and Care
Book a Free Certified Online
Doctor Consultation

FREQUENTLY ASKED QUESTIONS
I am item content. Click edit button to change this text. Lorem ipsum dolor sit amet, consectetur adipiscing elit. Ut elit tellus, luctus nec ullamcorper mattis, pulvinar dapibus leo.
I am item content. Click edit button to change this text. Lorem ipsum dolor sit amet, consectetur adipiscing elit. Ut elit tellus, luctus nec ullamcorper mattis, pulvinar dapibus leo.
I am item content. Click edit button to change this text. Lorem ipsum dolor sit amet, consectetur adipiscing elit. Ut elit tellus, luctus nec ullamcorper mattis, pulvinar dapibus leo.
I am item content. Click edit button to change this text. Lorem ipsum dolor sit amet, consectetur adipiscing elit. Ut elit tellus, luctus nec ullamcorper mattis, pulvinar dapibus leo.
I am item content. Click edit button to change this text. Lorem ipsum dolor sit amet, consectetur adipiscing elit. Ut elit tellus, luctus nec ullamcorper mattis, pulvinar dapibus leo.

RELATED VIDEOS
Understanding Your Cancer Diagnosis: A Beginner's Guide
This video breaks down the basics of a cancer diagnosis, explaining common terms, what to expect, and questions to ask your doctor. A gentle introduction for newly diagnosed patients.
Navigating Treatment Side Effects: Tips for Comfort
Learn practical strategies and expert advice on managing common side effects like fatigue, nausea, and pain during cancer treatment. Find ways to improve your daily comfort and well-being.
Life Beyond Cancer: Thriving in Survivorship
Explore the journey of cancer survivorship, focusing on emotional recovery, long-term health, and embracing a fulfilling life after treatment. Hear inspiring stories and expert insights.
Blog
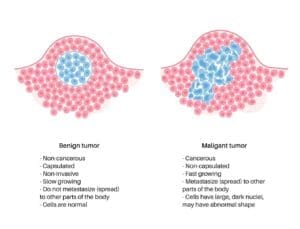
What Is the Difference Between Malignant and Benign Tumors?
Last Updated on November 14, 2025 by Ugurkan Demir At Liv Hospital, we know that getting a tumor diagnosis can be scary. But, not all

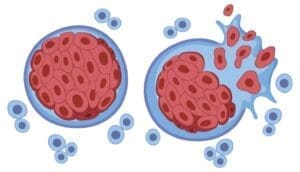
What Does a Cancer Tumor Look Like? Visual Differences Between Cancer Cells and Normal Cells Under a Microscope
Last Updated on November 14, 2025 by Ugurkan Demir Knowing how cancer cells look under a microscope is key for accurate diagnosis and treatment. At
Can a Benign Tumor Become Malignant? Understanding When Tumors Turn Cancerous
Last Updated on November 14, 2025 by Ugurkan Demir At Liv Hospital, we know that the thought of having a tumor can be scary. Not
