Last Updated on November 14, 2025 by mcelik
Did you know over 10 million Americans have a condition that weakens their bones? This makes them more likely to break bones. This condition is called osteoporosis. It happens when bones lose mineral density and mass.
Knowing what causes this condition is key to stopping it. Low bone density, often from a calcium deficiency, is a big risk. As we get older, our bones naturally lose density. But some things can make this happen faster.
Key Takeaways
- Osteoporosis primary cause is a silent disease that can lead to fractures.
- Low bone density is a significant risk factor for osteoporosis.
- Calcium deficiency can contribute to the development of osteoporosis.
- Understanding the main cause of osteoporosis is critical for prevention and treatment.
- A healthy lifestyle can help prevent osteoporosis.
Understanding Osteoporosis: A Silent Bone Disease
Osteoporosis is a “silent disease” that causes bones to break without pain. It makes bones weak and more likely to fracture. Knowing what osteoporosis is, how common it is, and how to keep bones strong is key.
Definition and Prevalence in the United States
Osteoporosis is a condition where bones lose density and strength, raising the risk of fractures. In the U.S., it’s a big problem, hitting older adults hard. It’s most common in non-Hispanic white women and Asian women, but it can affect anyone.
Understanding osteoporosis is vital, as millions in the U.S. are affected. The numbers are expected to grow as more people get older.
How Healthy Bones Maintain Strength
Healthy bones are always being rebuilt through bone resorption and formation. Bone health relies on a balance between these two. If bone resorption outpaces formation, bones can weaken and lead to osteoporosis.
Keeping bones strong involves good nutrition, hormonal balance, and exercise. For example, not enough vitamin D can hurt bone health by making it hard for the body to absorb calcium.
| Factor | Impact on Bone Health |
| Calcium Intake | Essential for bone density |
| Vitamin D Levels | Critical for calcium absorption |
| Hormonal Balance | Influences bone remodeling |
| Physical Activity | Stimulates bone strength |
By learning about osteoporosis and how to keep bones healthy, we can prevent fractures and maintain strong bones.
The Osteoporosis Primary Cause: Imbalance in Bone Remodeling
Osteoporosis mainly comes from an imbalance in bone remodeling. This imbalance happens when bone resorption goes up and bone formation goes down. Bone remodeling is key for keeping bones healthy. Any problem here can lead to osteoporosis.
Bone remodeling has two main parts: bone formation and bone resorption. Bone formation makes new bone tissue. Bone resorption breaks down old bone tissue. In healthy people, these two are balanced, keeping bone density steady.
Bone Formation vs. Bone Resorption Increase
In osteoporosis, the balance shifts, causing more bone resorption and less bone formation. This leads to bone loss and a higher risk of fractures. Aging plays a big role in this imbalance, as bone resorption goes up and bone formation slows down with age.
The table below shows the difference in bone formation and resorption between healthy people and those with osteoporosis:
| Process | Healthy Individuals | Individuals with Osteoporosis |
| Bone Formation | Balanced with bone resorption | Decreased |
| Bone Resorption | Balanced with bone formation | Increased |
When the Balance Tips Toward Bone Loss
When bone resorption outpaces bone formation, bone loss happens. This leads to lower bone density and a higher risk of fractures. Many factors can cause this imbalance, like aging, hormonal changes, and lifestyle choices. As we age, the risk of bone loss grows, making it key to watch bone health and take steps to prevent it.
“Osteoporosis is a major public health problem, affecting millions of people worldwide. Understanding the causes and risk factors of osteoporosis is critical for prevention and treatment.”
In summary, osteoporosis is mainly caused by an imbalance in bone remodeling. This imbalance is marked by more bone resorption and less bone formation. Knowing about this process and its factors can help prevent and treat osteoporosis.
Hormonal Factors Leading to Osteoporosis
Osteoporosis is linked to hormonal changes, like the drop in important hormones for bones. These imbalances can lower bone density, raising the risk of osteoporosis.
Estrogen Loss During Menopause
Menopause brings a big hormonal shift, with estrogen levels falling a lot. Estrogen helps keep bones strong by helping them grow and preventing them from breaking down. Without enough estrogen, bones start to lose density, making osteoporosis more likely. “Estrogen deficiency is a major risk factor for osteoporosis in postmenopausal women,” showing why it’s important to watch and possibly treat this change.
Testosterone Deficiency in Men
Testosterone is key for bone health in men. Low testosterone is linked to weaker bones and a higher chance of fractures. It can happen as men age or due to health issues, leading to osteoporosis.
Thyroid Hormone Imbalance Effects
Thyroid hormones are also vital for bones. Too much or too little thyroid hormone can harm bone density. This imbalance can cause bones to break down faster, increasing the risk of osteoporosis. “Thyroid hormone imbalance can have a profound impact on bone health, necessitating careful management.”
In summary, hormonal changes play a big role in osteoporosis risk. It’s key to understand and manage these hormonal effects to keep bones healthy and prevent osteoporosis.
Nutritional Deficiencies and Bone Health

Osteoporosis is a silent bone disease often linked to diet. It’s mainly caused by a lack of calcium and vitamin D. Without these nutrients, the risk of osteoporosis goes up.
Calcium Deficiency: The Foundation of Bone Health
Calcium is key for strong bones. Not getting enough can lead to osteoporosis. The body might take calcium from bones, making them weak. So, getting enough calcium is very important.
Recommended Daily Calcium Intake:
| Age Group | Recommended Daily Calcium Intake |
| 19-50 years | 1,000 mg |
| 51+ years | 1,200 mg |
Vitamin D Deficiency and Poor Calcium Absorption
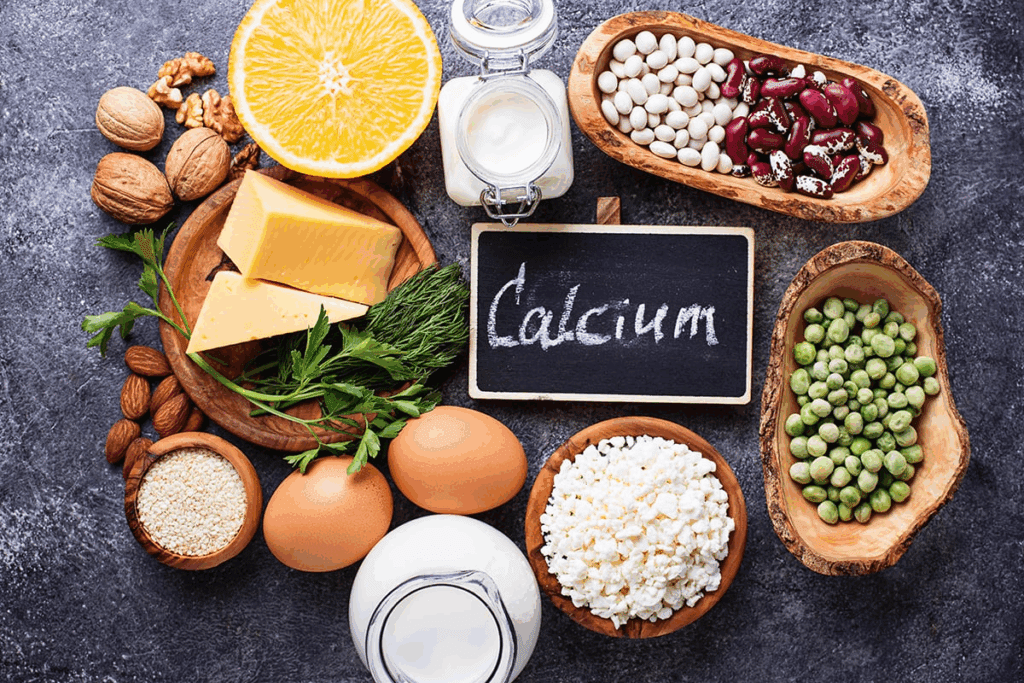
Vitamin D helps the body absorb calcium. Without enough vitamin D, the body can’t absorb calcium well. This can harm bone health and increase the risk of osteoporosis.
“Vitamin D is essential for the absorption of calcium in the gut, and its deficiency can lead to secondary hyperparathyroidism, which in turn can cause bone loss.” –
Endocrinologist
To keep bones strong, it’s important to eat enough calcium and vitamin D. Sometimes, supplements are needed to meet these needs.
Age-Related Changes in Bone Structure
As we get older, our bones naturally weaken. This happens because of changes in our bones as we age. These changes affect how strong our bones are.
Aging Bone Weakness: Natural Progression
Aging bone weakness is something everyone faces. It happens because the balance between making and breaking down bones changes. This balance shifts as we age, leading to weaker bones.
Key factors contributing to aging bone weakness include:
- Reduced osteoblast activity: Osteoblasts are cells that build bone. As we age, they work less, causing bones to form less.
- Increased osteoclast activity: Osteoclasts are cells that break down bone. With age, they work more, causing bones to lose mass.
- Hormonal changes: Hormones like estrogen and testosterone decline with age. This affects bone health.
Changes in Cellular Activity with Age
As we age, how our bones work changes a lot. The bone remodeling process, which involves osteoblasts and osteoclasts, gets less efficient. This imbalance can lead to bones losing more than they gain.
The impact of these changes can be seen in several areas:
- Bone density reduction: The imbalance in bone remodeling results in a net loss of bone density.
- Increased risk of osteoporosis: As bone density decreases, the risk of developing osteoporosis increases.
- Higher fracture risk: Weakened bones are more susceptible to fractures, which can significantly impact quality of life.
Understanding these age-related changes in bone structure is key. It helps us find ways to keep our bones healthy as we age.
Genetic Predisposition to Osteoporosis
It’s key to know about genetic risks for osteoporosis to help those at higher risk. Osteoporosis is shaped by genes, environment, and lifestyle.
Having family members with osteoporosis raises your risk. Studies link genes to bone density and fracture risk.
Family History Osteoporosis: Understanding Your Risk
A family history of osteoporosis is a big risk factor. If your parents or grandparents had it, you’re more likely to too. Genes affect bone health and loss rate.
Key genetic factors include genes for bone metabolism, like vitamin D and calcium.
Genetic Osteoporosis Risk Factors
Many genetic factors increase osteoporosis risk. These include:
- Genes that control bone metabolism
- Hormone levels, like estrogen and testosterone, important for bones
- Genetic effects on bone structure and density
Genetic risk is big, but not the only one. Lifestyle, diet, and health conditions also matter.
Knowing your genetic risk helps. Eat well, exercise, and avoid smoking and too much alcohol to lower your risk.
Lifestyle Factors Contributing to Low Bone Density
Many lifestyle choices affect bone density and health. Making smart choices can lower the risk of osteoporosis and fractures.
Sedentary Lifestyle Risk and Lack of Weight-Bearing Exercise
A sedentary lifestyle increases the risk of low bone density. Activities like walking, running, and dancing are key for strong bones. Weight-bearing exercise boosts bone growth and density, cutting down osteoporosis risk. People with desk jobs or who sit a lot should move more.
Small changes, like taking stairs or walking during breaks, help a lot. Adding resistance training to your routine also strengthens bones and muscles.
Smoking Bone Loss Connection
Smoking harms bone health. It cuts down blood flow and hinders calcium absorption, vital for strong bones. Smokers face a higher risk of osteoporosis and fractures.
Tobacco smoke also messes with hormone production needed for bone health. Quitting smoking is key to keeping bones strong and healthy.
Alcohol Bone Weakening Effects
Drinking too much alcohol raises osteoporosis risk. Alcohol disrupts calcium balance and bone formation, making bones weaker. For women, up to one drink a day is okay, and for men, up to two.
Drinking less can lessen alcohol’s negative impact on bones. Eating a diet full of calcium and vitamin D also supports bone health.
Medications and Medical Conditions Affecting Bone Health
Medications and health conditions can greatly affect bone health. Some drugs, used for a long time, can lower bone density. This makes osteoporosis more likely.
Chronic Steroid Use and Bone Deterioration
Chronic steroid use, like glucocorticoids, harms bones. Long-term steroid use can slow bone formation and speed up bone breakdown. This results in less bone density.
Glucocorticoid-induced osteoporosis is a common problem for those on long-term steroids. The risk is highest in the first few months. But, there are ways to prevent it.
Other Medications That Affect Bone Density
Other drugs can also affect bones. These include some anticonvulsants, aromatase inhibitors for breast cancer, and certain antidepressants.
| Medication Type | Effect on Bone Density |
| Anticonvulsants | May decrease bone density |
| Aromatase Inhibitors | Can lead to bone loss |
| Certain Antidepressants | Associated with increased risk of osteoporosis |
People on these medications should talk to their doctor about bone health. Regular checks and preventive steps can help protect bones.
Knowing how medications affect bones is key to keeping bones strong. By understanding risks and taking action, people can lower their chance of osteoporosis.
Diagnosing Low Bone Density and Osteoporosis
Bone density testing is key to spotting those at risk of osteoporosis. This test checks the minerals in your bones. It helps see how healthy your bones are. Knowing this is vital for treating and preventing bone breaks.
Bone Density Testing: When and Why
Bone density testing, or DXA, finds osteoporosis and fracture risks. It looks at bone mineral density in places like the hip and spine. It’s for women over 65 and men over 70, or those with fracture history or risk factors.
Why is bone density testing important? It shows how strong your bones are and spots problems early. This means you can get help before things get worse, lowering fracture risks.
Understanding Your T-Score Results
Your bone density test gives a T-score. It compares your bone density to a healthy young adult of the same sex. A T-score of -1 or above is normal. Scores between -1 and -2.5 mean low bone mass (osteopenia). A score of -2.5 or lower is osteoporosis.
| T-Score Range | Diagnosis |
| -1 or above | Normal |
| Between -1 and -2.5 | Osteopenia (Low Bone Mass) |
| -2.5 or lower | Osteoporosis |
Knowing your T-score is key to taking care of your bones. Doctors use it to suggest lifestyle changes, supplements, or meds to boost bone density and lower fracture risk.
Prevention Strategies for Maintaining Bone Health
Keeping bones strong needs a mix of good food and regular exercise. These are key to avoiding osteoporosis. A healthy lifestyle with the right diet and activity can lower bone disorder risks.
Nutritional Approaches to Prevent Bone Deficiency
Eating a diet full of calcium and vitamin D is key for strong bones. Calcium is vital for bones, and vitamin D helps absorb calcium. Dairy, leafy greens, and fortified foods are good sources of calcium. Vitamin D comes from sunlight, fatty fish, and supplements.
Other nutrients like magnesium and potassium also help bones. Eating fruits, vegetables, and whole grains gives you these important nutrients.
Exercise Recommendations for Bone Strengthening
Exercise is essential for keeping bones dense and preventing osteoporosis. Walking, running, and dancing are great for bones because they stimulate growth. Using weights or resistance bands can also boost bone health by building muscle.
Adding exercises that improve balance and flexibility, like tai chi or yoga, is important. These help prevent falls and fractures. A balanced routine with weight-bearing, resistance, and balance exercises keeps bones strong and prevents osteoporosis.
Combining good nutrition with exercise can greatly lower the risk of osteoporosis. This way, people can keep their bones strong for life.
Treatment Options for Established Osteoporosis
Osteoporosis treatment includes various therapies and lifestyle changes. These help manage the condition well.
When osteoporosis is found, doctors suggest a mix of medicines and lifestyle changes. These aim to slow bone loss and lower fracture risk.
Medication Therapies for Bone Preservation
Medicine is key in treating osteoporosis. It aims to keep bone density high and prevent fractures.
- Bisphosphonates: These are top choices for osteoporosis treatment. They slow bone loss and lower fracture risk.
- Denosumab: Given by injection, it targets a protein that breaks down bones.
- Teriparatide: This boosts bone formation, helping those at high fracture risk.
| Medication | Administration | Primary Effect |
| Bisphosphonates | Oral or IV | Reduces bone resorption |
| Denosumab | Injection | Decreases bone breakdown |
| Teriparatide | Injection | Stimulates bone formation |
Lifestyle Modifications for Those with Diagnosis
Along with medicine, lifestyle changes are vital for osteoporosis management.
Dietary Changes: It’s important to get enough calcium and vitamin D. Include dairy, leafy greens, and fortified cereals in your diet.
Exercise: Doing weight-bearing and resistance exercises strengthens bones. Walking, jogging, and weight training are good choices.
Combining medicines with lifestyle changes helps manage osteoporosis. It also lowers the risk of complications.
Long Term Osteoporosis: Complications and Management
Osteoporosis can lead to more fractures and complications over time. It’s important to manage it well to avoid fractures and keep a good quality of life.
Fracture Risk and Prevention
Fractures are a big worry with long-term osteoporosis. Preventing fractures is key in managing osteoporosis. This can be done through lifestyle changes, better nutrition, and medicine.
People with osteoporosis should make their homes safer to avoid falls. This means removing tripping hazards and improving the lighting. Also, exercises that boost balance and strength can help prevent falls.
Living Well with Osteoporosis
Managing osteoporosis involves diet, exercise, and sometimes medicine. A balanced diet with lots of calcium and vitamin D is vital for bone health.
Doing weight-bearing and resistance exercises regularly can strengthen bones and lower fracture risk. It’s also key for those with osteoporosis to stay updated on their condition and work with their healthcare team.
- Maintain a balanced diet rich in calcium and vitamin D.
- Engage in regular weight-bearing and resistance exercises.
- Stay informed about osteoporosis management.
- Work closely with your healthcare provider.
Conclusion: Taking Control of Your Bone Health
Understanding osteoporosis is key to strong bones and fewer fractures. Knowing what causes bone loss helps people protect their bones.
Preventing osteoporosis needs good nutrition, exercise, and lifestyle changes. Eating enough calcium and vitamin D, doing weight-bearing exercises, and quitting smoking are important. These steps help keep bones strong.
Protecting your bones is a long-term job, but it’s worth it. Making smart choices and living healthy can lower your risk of osteoporosis. This leads to a better, more active life.
FAQ
What is osteoporosis and how does it affect the body?
Osteoporosis is a condition where bones lose density and strength. This makes bones more likely to break. It’s often called a “silent disease” because you might not feel any symptoms until a bone breaks.
What are the main causes of osteoporosis?
The main cause is when bone loss happens faster than bone growth. Hormonal changes, not getting enough nutrients, and lifestyle choices also play a part.
How does estrogen loss during menopause affect bone health?
Estrogen helps keep bones strong. When estrogen levels drop during menopause, bones start to break down more. This can lead to osteoporosis.
What is the role of calcium and vitamin D in maintaining bone health?
Calcium is key for strong bones. Vitamin D helps the body use calcium. Not having enough of either can harm bones.
How does a sedentary lifestyle contribute to osteoporosis?
Not moving enough can weaken bones. This is because bones need exercise to stay strong.
Can certain medications affect bone health?
Yes, some medicines, like steroids, can harm bones. This can lead to osteoporosis.
How is osteoporosis diagnosed?
Doctors use bone density tests to find osteoporosis. These tests check the bones in the hip, spine, or other areas.
What are the treatment options for established osteoporosis?
Treatments include medicines, making lifestyle changes, and eating right. These help manage the condition and stop bones from getting weaker.
How can osteoporosis be prevented?
To prevent osteoporosis, eat foods rich in calcium and vitamin D. Exercise regularly. Avoid things that harm bones.
What are the long-term complications of osteoporosis?
If not treated, osteoporosis can cause more fractures. This can really hurt your quality of life and independence.
Can genetic factors contribute to osteoporosis?
Yes, having a family history of osteoporosis raises your risk. It’s something to talk to your doctor about.
How does thyroid hormone imbalance affect bone health?
Thyroid hormones help control bone health. An imbalance can lead to osteoporosis.
What is the impact of smoking on bone health?
Smoking damages bones and increases fracture risk. It’s a big risk factor for osteoporosis.
How does excessive alcohol consumption affect bone density?
Drinking too much alcohol weakens bones. It raises the risk of osteoporosis
References
- Bae, S. (2023). Position Statement: Exercise Guidelines for Osteoporosis. International Journal of Environmental Research and Public Health.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10345999/