Last Updated on November 26, 2025 by Bilal Hasdemir

Ovarian cancer is a big health worry, mainly for women in certain age groups. The American Cancer Society says the risk goes up with age. Most cases happen in women over 60.
It’s interesting to know that ovarian cancer can hit at any age. But, the chance of getting it changes a lot with age. Knowing these risks helps find and stop it early.
Key Takeaways
- The risk of ovarian cancer increases with age.
- Most ovarian cancer cases are diagnosed in women over 60.
- Understanding age-related risks is key to early detection.
- Ovarian cancer can occur at any age, but is less common in younger women.
- Awareness of ovarian cancer risks can help in prevention.
Understanding Ovarian Cancer: A Brief Overview
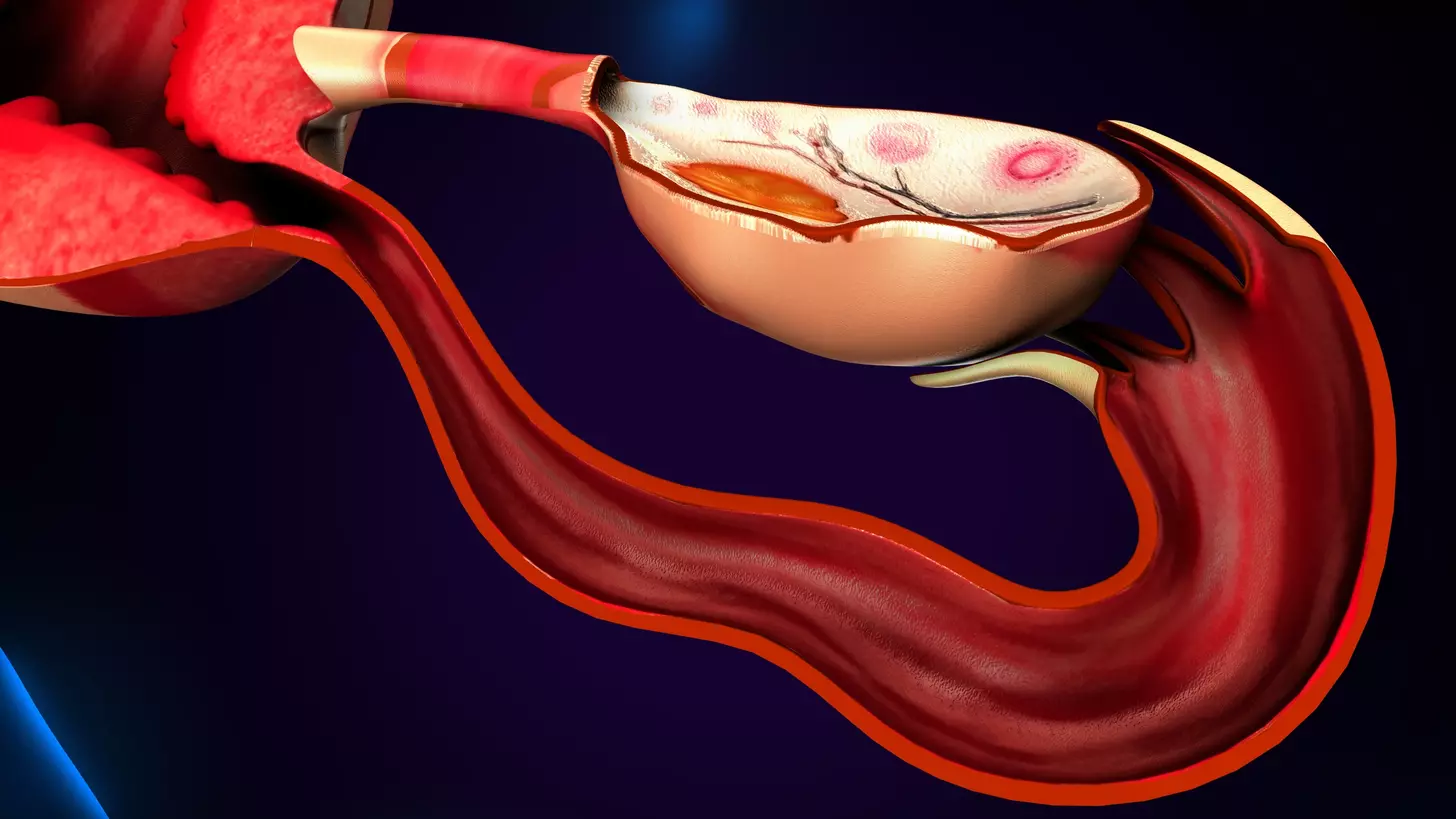
Ovarian cancer is a group of cancers that start in the ovaries. It has different types and risk factors. This disease is influenced by genetics, hormones, and the environment.
Types of Ovarian Cancer
Ovarian cancer is not just one disease; it’s many. Each type has its own features. The main types are:
- Epithelial ovarian cancer, which starts in the outer layer of the ovary
- Germ cell tumors, which start in the egg-producing cells
- Sex cord-stromal tumors, which start in the tissue that holds the ovary together
General Risk Factors
Many things can raise your risk of getting ovarian cancer. These include:
| Risk Factor | Description |
| Family History | A history of ovarian or breast cancer in first-degree relatives |
| Genetic Mutations | Having BRCA1 and BRCA2 gene mutations |
| Age | Getting older, after 50 |
| Reproductive History | Never having been pregnant or having a first pregnancy at an older age |
These risk factors help find women who should get screened early and take preventive steps.
Ovarian Cancer Age Group Distribution
Ovarian cancer cases are spread out across different ages. This pattern is key to understanding the disease. It helps in assessing risks and setting up screening plans.
Global Age Distribution Patterns
Ovarian cancer rates change with age and location worldwide. Most cases are found in women over 50. This is based on global data.
A study showed the highest number of ovarian cancer cases is between 55 and 64. After 70, the rates drop sharply.
| Age Group | Global Incidence Rate |
| Under 40 | 2.5 per 100,000 |
| 40-49 | 15.6 per 100,000 |
| 50-59 | 30 per 100,000 |
| 60-69 | 40.2 per 100,000 |
| 70+ | 25.1 per 100,000 |
United States Age Statistics
In the US, ovarian cancer trends are similar to global ones, with some differences. Most cases are found in women aged 55 to 64, says the American Cancer Society.
In the US, ovarian cancer rates rise with age. There’s a big jump in rates between 60 and 69.
| Age Group | US Incidence Rate |
| Under 40 | 1.8 per 100,000 |
| 40-49 | 12.1 per 100,000 |
| 50-59 | 28.5 per 100,000 |
| 60-69 | 42.1 per 100,000 |
| 70+ | 30.5 per 100,000 |
The Median Age of Ovarian Cancer Diagnosis
Knowing the median age of ovarian cancer diagnosis is key for assessing risk and planning screenings. It shows when women are most likely to get this disease.
Understanding the 63-Year Median
The median age for ovarian cancer diagnosis is 63 years, recent data shows. This means half of women diagnosed are under 63, and the other half are older. This age is important for understanding who gets ovarian cancer.
Many things affect this median age, like the types of ovarian cancer and risk factors. These include genetic mutations or family history. Knowing these can help figure out your risk.
What This Means for Risk Assessment
The median age of 63 is important for assessing risk. Women near or over 63 should watch their risk factors closely. They should talk about screening with their doctors.
- Key Risk Factors: Family history, genetic mutations (e.g., BRCA1 and BRCA2), and personal history of other cancers.
- Screening Recommendations: Women with high-risk factors may need to start screening earlier or more frequently.
- Lifestyle Considerations: A healthy lifestyle, like a balanced diet and exercise, can lower cancer risk.
By knowing the median age of ovarian cancer diagnosis, women can better understand their risk. They can take steps for early detection and prevention.
Ovarian Cancer in Young Women
Ovarian cancer can happen at any age, and young women with certain genetic mutations are at higher risk. While most cases of ovarian cancer happen as women get older, young women can also be affected. This is often because of inherited factors.
Incidence Rates Under Age 40
Ovarian cancer is rare in women under 40, but it does happen. Studies show that genetic mutations like BRCA1 and BRCA2 play a big role. These mutations can greatly increase the risk of ovarian cancer at a younger age.
Unique Challenges for Young Patients
Young women with ovarian cancer face special challenges. They often worry about their family planning and fertility. Being diagnosed can be very hard, as these women are often at a young age with young families or plans for future pregnancies.
Fertility Considerations
Preserving fertility is very important for young women with ovarian cancer. The treatment they choose can affect their ability to have children in the future. Options like fertility-sparing surgery might be considered for early-stage cancers. This could help women keep their fertility.
It’s key for young women to understand their genetic risk, like BRCA mutations. Genetic testing can give them important information about their risk. This can help them make decisions about preventive measures, like prophylactic oophorectomy after they’ve had children.
Ovarian Cancer in Your 20s and 30s

It’s important to know about ovarian cancer in younger women. This knowledge helps with early detection and treatment. Even though the risk is lower for women under 40, it’s key to be aware of the possibility of ovarian cancer at a young age.
Early-Onset Cases: How Common?
Ovarian cancer in women under 40 is called early-onset. The American Cancer Society says about 10% of ovarian cancer cases happen in women under 45. A small part of these cases are in women under 30.
Statistics on Early-Onset Ovarian Cancer:
| Age Group | Percentage of Ovarian Cancer Cases |
| Under 20 | <1% |
| 20-29 | 2-3% |
| 30-39 | 8-10% |
Symptoms That Younger Women Should Watch For
Symptoms of ovarian cancer can be hard to spot and might seem like other health issues. Younger women should keep an eye out for symptoms like:
- Pelvic or abdominal pain
- Bloating or swelling in the abdomen
- Difficulty eating or feeling full quickly
- Urinary urgency or frequency
Genetic Testing Recommendations
Women with a family history of ovarian or breast cancer might need genetic testing. Finding mutations in the BRCA1 and BRCA2 genes can raise the risk of ovarian cancer a lot.
Guidelines for Genetic Testing:
- Women with a known BRCA1 or BRCA2 mutation should talk to their doctor about screening.
- Those with a strong family history of ovarian or breast cancer should think about genetic counseling.
Ovarian Cancer Risk in Your 40s
Ovarian cancer risk in women in their 40s is influenced by various pre-menopausal factors. During this decade, women may experience significant hormonal changes. These changes can impact their risk profile. Understanding these factors is key for early detection and prevention.
Pre-Menopausal Risk Factors
Pre-menopausal women, in their 40s, should know about several risk factors. These include family history, genetic mutations like BRCA1 and BRCA2, and previous reproductive health issues. Women with a history of endometriosis or PCOS may also face higher risks.
Genetic testing is advised for women with a family history of ovarian or breast cancer. It helps assess risk and guide preventive steps.
Screening Recommendations
There’s no universal screening test for ovarian cancer. But, women in their 40s with risk factors should talk to their doctor about screening. The CA-125 blood test and transvaginal ultrasound might be used for screening.
It’s vital for women to know the pros and cons of these tests. Early detection is key to better survival rates. Following screening guidelines is essential.
Warning Signs Specific to This Age Group
Women in their 40s should watch for symptoms that could point to ovarian cancer. These include persistent bloating, abdominal pain, and difficulty eating. Also, look out for urinary urgency.
Being aware of these signs and talking to a healthcare provider can lead to early diagnosis. Remember, ovarian cancer symptoms can be subtle. So, staying vigilant is important.
Ovarian Cancer After Menopause
Ovarian cancer risk doesn’t go away after menopause. It’s a time when awareness is key. Women need to know about the changes and how they might affect ovarian cancer risk.
Hormonal Changes and Cancer Risk
Menopause brings big hormonal changes, like a drop in estrogen. Studies show these changes can impact ovarian cancer risk. The drop in estrogen might affect how some ovarian cancer cells grow, but scientists are studying this more.
Hormone replacement therapy (HRT) is often used to ease menopause symptoms. But its effect on ovarian cancer risk is complex. It’s something to think about carefully.
Post-Menopausal Warning Signs
Knowing the signs of ovarian cancer after menopause is key for early detection. Common symptoms include:
- Pelvic or abdominal pain
- Bloating or swelling in the abdomen
- Difficulty eating or feeling full quickly
- Urinary urgency or frequency
Women should watch for these symptoms and see a doctor if they don’t go away. Catching it early can make a big difference in treatment.
Hormone Replacement Therapy Considerations
The link between HRT and ovarian cancer risk is being studied. Some research says HRT might slightly raise the risk, mainly with long-term use. Women should talk to their doctor about their risk and the pros and cons of HRT.
By understanding hormonal changes, knowing warning signs, and thinking about HRT, women can manage their ovarian cancer risk after menopause better.
Ovarian Cancer in Women Over 50
Ovarian cancer risk goes up for women over 50. It’s important to know why. As women get older, their bodies change in ways that can raise their cancer risk. Knowing these changes and risks helps with early detection and treatment.
Why Risk Increases After 50
The risk of ovarian cancer goes up after 50 because of hormones, genes, and the environment. Hormonal changes during menopause are a big factor. Also, genetic mutations build up over time.
Detection Challenges in Older Women
Finding ovarian cancer in older women is hard because early symptoms are not clear. Symptoms like bloating, pain, and trouble eating are often thought of as other things. This can lead to a late diagnosis.
Comorbidity Factors
Women with ovarian cancer over 50 often have other health issues. Heart disease, diabetes, and high blood pressure make treatment harder. They need a full care plan.
Peak Age Range for Ovarian Cancer Diagnosis
Ovarian cancer often strikes between 55 and 64 years old. This age group is key because of many changes and risks. These changes and risks grow stronger with age.
Understanding the 55-64 Age Spike
Women aged 55-64 face a higher risk of ovarian cancer. Hormonal, genetic, and environmental factors play a role. By this age, many women have gone through menopause. Genetic risks also become clearer.
A study in the Journal of Clinical Oncology found a big jump in ovarian cancer rates after 50. The highest rates are between 55 and 64 years old.
“The age-specific incidence rates of ovarian cancer show a steep increase starting at around age 50, with the highest rates observed in women aged 55-64,” the study notes.
Risk Factors Specific to This Age Range
Women in their 50s and early 60s face certain risks. These include:
- Family history of ovarian or breast cancer
- Genetic mutations such as BRCA1 and BRCA2
- History of endometriosis
- Obesity and lack of physical activity
Knowing these risks helps with early detection and prevention.
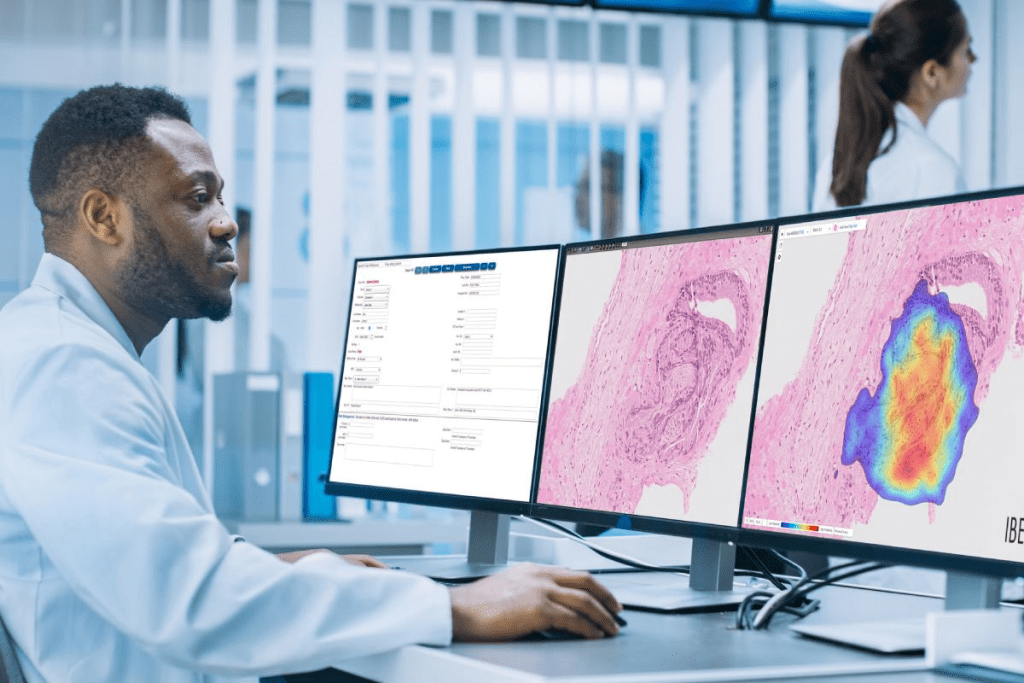
Latest Research on Peak Incidence
Recent studies have looked into ovarian cancer in older women. They found that cancers in this age group have specific genetic mutations. These could be targets for new treatments.
| Age Group | Incidence Rate | Common Risk Factors |
| 55-59 | Higher incidence | Genetic mutations, family history |
| 60-64 | Peak incidence | Obesity, endometriosis, hormonal changes |
These findings are vital for creating age-specific screening and treatment plans.
Ovarian Cancer in Elderly Women
As more people live longer, ovarian cancer in older women is a big worry. Ovarian cancer hits women of all ages hard, but it’s more common in the elderly.
Incidence in Women Over 70
The risk of ovarian cancer goes up with age. Women over 70 are hit the hardest. Most ovarian cancer cases are found in women who have gone through menopause, with many being over 70.
Key statistics on ovarian cancer incidence in elderly women include:
- Increased risk with advancing age
- Higher incidence rates in post-menopausal women
- Majority of diagnoses occurring in women over 70
Treatment Considerations for Elderly Patients
When treating ovarian cancer in older women, doctors must think about many things. This includes the patient’s health, other health issues, and how treatment will affect their life. Personalized treatment plans are key to meet the needs of older patients.
Treatment might include surgery, chemotherapy, or both. It’s tailored to each patient’s situation and what they want.
Quality of Life Concerns
Keeping quality of life in mind is vital when treating ovarian cancer in older women. This means managing symptoms, reducing side effects, and giving supportive care. This helps ensure the best results.
Quality of life considerations include:
- Symptom management
- Minimizing treatment side effects
- Supportive care
Genetic Factors and Age of Onset
Genetic factors are key in when ovarian cancer starts. Some genetic mutations raise the risk of ovarian cancer, often at a younger age.
The link between genetics and ovarian cancer is complex. It involves many genes and pathways. Knowing these genetic details helps in assessing risk and making screening and prevention plans.
BRCA Mutations and Early-Onset Ovarian Cancer
BRCA1 and BRCA2 mutations are big risk factors for ovarian cancer. Women with these mutations face a higher risk of ovarian cancer, often at a younger age. Studies show BRCA mutation carriers are more likely to get ovarian cancer before 50.
“Women with BRCA1 mutations have a 39-46% lifetime risk of developing ovarian cancer, while those with BRCA2 mutations have a 10-27% risk.”
Lynch Syndrome and Age-Related Risk
Lynch syndrome, or hereditary nonpolyposis colorectal cancer (HNPCC), also raises ovarian cancer risk. Women with Lynch syndrome face a higher risk of ovarian cancer, often at a younger age than those without it.
| Genetic Syndrome | Lifetime Risk of Ovarian Cancer | Typical Age of Onset |
| BRCA1 Mutation | 39-46% | 40-50 |
| BRCA2 Mutation | 10-27% | 45-55 |
| Lynch Syndrome | 8-14% | 40-50 |
Other Genetic Risk Factors Across Age Groups
While BRCA mutations and Lynch syndrome are major risks, other genetic mutations also play a role. For example, mutations in DNA repair genes can increase ovarian cancer risk.
Genetic testing is key in finding high-risk individuals. Women with a family history of ovarian or breast cancer should think about genetic counseling and testing.
Age-Related Survival Rates
It’s key to know how age affects survival rates for ovarian cancer. Age plays a big role in how well a patient does and how treatment works.
How Age Affects Prognosis
Age changes how well a patient with ovarian cancer does. Younger patients usually do better than older ones. This is because of their health, other health problems, and how aggressive the cancer is.
Younger patients often have fewer health problems. They can handle tough treatments better, which helps them live longer. Older patients face more challenges because of their health issues.
“Age is an important factor in determining the survival rate of ovarian cancer patients. Younger women tend to have more favorable outcomes due to fewer comorbid conditions and better tolerance to treatment.”
Five-Year Survival Rates by Age Group
Survival rates for ovarian cancer change with age. Recent data shows younger women do better than older ones.
- Women under 40 years old have a relatively high five-year survival rate, often cited around 70-80%.
- For women between 40 and 59 years old, the five-year survival rate is generally lower, typically ranging from 40-60%.
- Women aged 60 and above often have the lowest five-year survival rates, usually between 20-40%.
These numbers highlight the need for early detection. They show how age affects survival rates. Knowing this helps doctors plan better treatments and improve patient results.
How Age Influences Treatment Decisions
Ovarian cancer treatment choices change with a patient’s age. Age affects health, cancer stage, and tumor type. These factors are key in deciding treatment.
Treatment Approaches for Younger Patients
Young women with ovarian cancer need special care. Fertility preservation is a big concern. Doctors might choose surgery that saves fertility and use targeted treatments.
Younger patients can handle more aggressive treatments. This is because they are healthier. They might also join clinical trials.
Treatment Considerations for Middle-Aged Women
Women in their 40s and 50s face unique challenges. Hormonal therapies might be an option for some. The goal is to treat the cancer well while keeping quality of life high.
Surgery and chemotherapy are key. The type and extent of surgery depend on age and health.
Treatment Adaptations for Elderly Patients
Elderly patients with ovarian cancer have special needs. They often have other health issues and are less resilient. Treatment plans must be made with their health in mind.
For some, less intense treatments or palliative care are better. These focus on managing symptoms and improving quality of life, not just curing the cancer.
| Age Group | Treatment Considerations | Key Factors |
| Younger Patients (<40) | Fertility-sparing options, aggressive treatments | Fertility preservation, overall health |
| Middle-Aged (40-64) | Balancing efficacy and quality of life, hormonal therapies | Menopausal status, comorbidities |
| Elderly (65+) | Palliative care, less intensive treatments | Comorbid conditions, physiological reserve |
Screening and Prevention Strategies by Age
Age is key in choosing the right screening and prevention for ovarian cancer. As women age, their risk and screening needs change a lot.
Recommendations for High-Risk Young Women
Young women at high risk, due to genes like BRCA1 or BRCA2, might start screening at 25-30. Genetic counseling is very important for them to know their risks and screening choices.
Risk-reducing salpingo-oophorectomy (removal of ovaries and fallopian tubes) might be an option for them after they’re done having kids.
Screening Guidelines for Women 35-50
Women aged 35 to 50 face different screening needs based on their risk. Those with a family history or genetic risk might need more tests.
| Age Group | Risk Level | Screening Recommendation |
| 35-40 | Average Risk | No routine screening |
| 35-40 | High Risk | Annual TVUS and CA-125 |
| 40-50 | Average Risk | Discuss risks and benefits with doctor |
| 40-50 | High Risk | Annual TVUS and CA-125, consider risk-reducing surgery |
Prevention Strategies for Post-Menopausal Women
Post-menopausal women should watch for signs of ovarian cancer. Routine screening isn’t advised, but seek medical help for any symptoms that don’t go away.
High-risk post-menopausal women might need ongoing tests like CA-125 and ultrasound. But, talk to a doctor about the pros and cons.
When to Start Discussing Ovarian Cancer Risk with Your Doctor
It’s important to know when to talk to your doctor about ovarian cancer risk. This can lead to early detection and prevention. It helps identify risk factors and find the best health plan for you.
Family History Considerations
A family history of ovarian cancer is a big risk factor. If a first-degree relative (mother, sister, or daughter) has ovarian cancer, talk to your doctor. Genetic mutations like BRCA1 and BRCA2 also raise your risk. Knowing your family history can guide genetic testing.
Creating a family history chart can help. It makes it easier to see cancer patterns in your family.
Age-Based Discussion Timeline
When to talk to your doctor about ovarian cancer risk depends on your family history and health. Women with a big family history should talk to their doctor in their late 20s to early 30s.
| Age Group | Discussion Points | Actions to Consider |
| 20s-30s | Family history, genetic risk | Genetic testing, risk assessment |
| 40s-50s | Screening options, risk factors | Regular check-ups, symptom awareness |
| 60s and beyond | Post-menopausal risks, symptom monitoring | Continued screening, health monitoring |
Questions to Ask at Different Life Stages
At different life stages, ask your doctor specific questions about ovarian cancer risk. Younger women should ask about genetic testing and family history. Older women should focus on screening options and symptoms.
- What are my risk factors for ovarian cancer?
- Should I consider genetic testing?
- What symptoms should I be aware of?
- What screening options are available for me?
Talking to your doctor about ovarian cancer risk at the right time is key. Being informed about your risk factors helps you stay healthy.
Conclusion: Understanding Age-Related Ovarian Cancer Risk
It’s important to know how age affects ovarian cancer risk. Ovarian cancer can happen at any age. But, the risk goes up a lot after 50. The biggest risk is for women between 55 and 64 years old.
Knowing about age-related risks helps everyone make better choices. This includes screening, prevention, and treatment. Women with a family history or genetic risk, like BRCA mutations, should talk to their doctor about their risk.
Spreading the word about ovarian cancer and its age-related risks can help. It can lead to finding cancer early and better treatment. By staying informed and proactive, women can protect their health and lower their risk of ovarian cancer.
FAQ
What is the common age for ovarian cancer diagnosis?
Most ovarian cancer cases are found in women over 55. The median age is 63 years old.
Can ovarian cancer occur in young women?
Yes, it’s rare but ovarian cancer can happen in young women. Women under 40 make up a small part of cases.
Are there any genetic risk factors for ovarian cancer?
Yes, certain genes like BRCA1 and BRCA2 raise the risk. Women with a family history of ovarian or breast cancer should get tested.
How does age affect ovarian cancer survival rates?
Age greatly impacts survival rates. Younger women tend to have better chances than older ones.
What are the symptoms of ovarian cancer that women in their 20s and 30s should watch for?
Women in their 20s and 30s should look out for symptoms like bloating, pelvic pain, and irregular periods. These could be signs of ovarian cancer.
How often should women over 50 be screened for ovarian cancer?
Women over 50 should talk to their doctor about screening. Those with average risk usually don’t need routine tests.
Can hormone replacement therapy increase the risk of ovarian cancer?
Some studies link hormone therapy to ovarian cancer risk. But the evidence isn’t clear. Women should talk to their doctor about their risk.
What are the treatment options for ovarian cancer in elderly women?
Treatment for elderly women depends on their health and the cancer’s stage. Options include surgery, chemotherapy, and more.
How does family history impact ovarian cancer risk?
A family history of ovarian or breast cancer increases risk. Women with this history should discuss their risk with their doctor.
At what age should women start discussing ovarian cancer risk with their doctor?
Women should talk about ovarian cancer risk with their doctor in their 20s or 30s. This is important if they have a family history.
What are the peak age ranges for ovarian cancer diagnosis?
Most ovarian cancer cases happen in women between 55 and 64. This is the peak age range.
How does age influence treatment decisions for ovarian cancer?
Age plays a big role in treatment choices. Younger women might get more aggressive treatments. Older women might need more tailored plans.
References
- Lheureux, S., Gourley, C., Vergote, I., & Oza, A. M. (2019). Epithelial ovarian cancer. The Lancet, 393(10177), 1240-1253.https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(18)32552-2/fulltext