Ovarian cysts are fluid-filled structures that grow in the ovaries during the menstrual cycle. They are common in women of reproductive age. These cysts can worry people, mainly if they affect menstrual cycles ovarian cystic.
These growths appear on or inside the ovaries. Most are harmless and disappear on their own. But knowing why they happen is key to keeping menstrual health in check. At places like Liv Hospital, they offer thorough checks and care plans based on science.
Key Takeaways
- Ovarian cysts are a common condition in reproductive-age women.
- Most ovarian cysts are harmless and resolve without treatment.
- Understanding the causes of ovarian cysts is essential for managing menstrual health.
- Comprehensive evaluation and evidence-based care can address concerns related to ovarian cysts.
- Ovarian cysts can potentially impact menstrual periods.
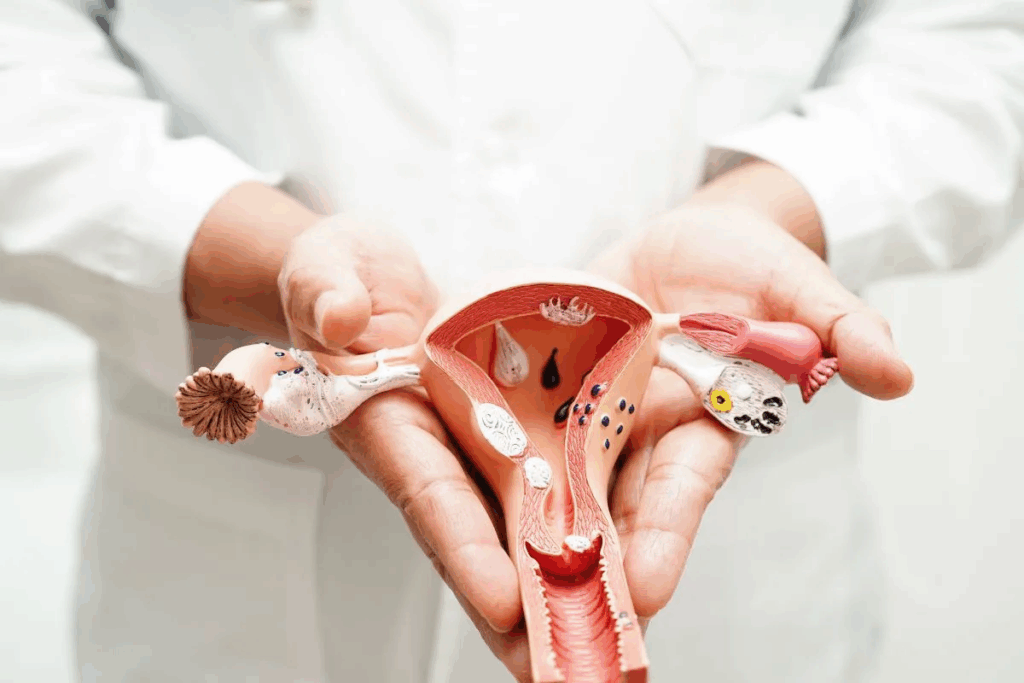
Understanding Ovarian Cysts: Definition and Prevalence
Ovarian cysts are fluid-filled sacs that grow on the ovaries. They are more common than you might think. These cysts can vary in size and are usually harmless.
What Are Ovarian Cysts?
An ovarian cyst is a fluid-filled sac on an ovary. They are common and often don’t cause symptoms. Most ovarian cysts are harmless and go away on their own in a few months.
Ovarian cysts can be different types. The most common type is the functional or physiological cyst. These cysts are usually harmless and may go away by themselves.
How Common Are Ovarian Cysts?
Ovarian cysts are common among women. About 10 out of 100 women have them. This shows how widespread they are.
Studies also show that postmenopausal women have an 18% chance of getting ovarian cysts over 15 years. This data shows how common ovarian cysts are at different stages of a woman’s life.
This information is key to understanding ovarian cysts. It helps us know their causes and how they affect women’s health. This is important for menstrual cycles and reproductive health.
The Normal Ovarian Function and Menstrual Cycle
To understand ovarian cysts, we must first know how ovaries work and their role in the menstrual cycle. The ovaries are key to the female reproductive system. They must function well for reproductive health.
How Ovaries Work
The ovaries have two main jobs. They release an egg every 28 days and make estrogen and progesterone. These hormones control the menstrual cycle and get the uterus ready for pregnancy. The balance between these hormones and the ovaries is key for menstrual health.
Each menstrual cycle, the ovaries change a lot. They have many follicles, each with an egg. Usually, one egg is released in ovulation. The empty follicle then turns into the corpus luteum, making progesterone for a possible pregnancy. Physiological cysts, like follicular and luteal cysts, can form because of these hormonal changes.
The Role of Ovaries in Menstruation
The ovaries are vital for menstruation by controlling the cycle with hormones. Estrogen and progesterone levels change, affecting the uterine lining. If there’s no pregnancy, the corpus luteum breaks down, causing a drop in progesterone. This leads to menstruation. Knowing this helps us see how cysts can affect menstrual health.
Physiological cysts, like follicular and luteal cysts, are common and usually harmless. They come from normal ovary function. But, they can sometimes mess with the menstrual cycle. This shows why understanding normal ovary function is so important.
Types of Ovarian Cystic Conditions and Their Formation
Ovarian cysts can be divided into different types based on how they form and what they are like. Knowing these types helps us understand their causes and how to treat them. These cysts are fluid-filled sacs on the ovaries, and they can affect women’s health in many ways.
Functional/Physiological Cysts
Functional or physiological cysts are the most common type. They happen as part of the menstrual cycle and are usually harmless and short-lived. They can be either follicular or corpus luteum cysts.
Follicular cysts happen when a follicle doesn’t burst to release an egg. Corpus luteum cysts form when the corpus luteum doesn’t dissolve after releasing an egg.
Studies show that about 14% of women have simple cysts when first checked, with an 8% chance of new cysts in a year. These cysts often don’t cause symptoms and might go away without treatment.
Pathological Cysts
Pathological cysts are less common and not tied to the menstrual cycle. They can be benign or cancerous and might need medical help. They include dermoid cysts and mucinous cystadenomas.
These cysts can grow big and cause pain or discomfort. They’re often found during a pelvic exam or imaging tests.
Endometriomas and Other Complex Cysts
Endometriomas are linked to endometriosis, where tissue like the uterus lining grows outside the uterus. These cysts are filled with old blood. Other complex cysts include dermoid cysts and mucinous cystadenomas, which can be benign or cancerous.
Endometriomas can cause a lot of pain and may lead to infertility. Treatment depends on the cyst size, symptoms, and reproductive plans.
The table below shows the main types of ovarian cysts and their characteristics:
Type of Cyst | Description | Common Symptoms |
Functional/Physiological | Develops as part of the menstrual cycle | Usually asymptomatic, may resolve on their own |
Pathological | Not related to the menstrual cycle, can be benign or malignant | Pelvic pain, discomfort, may grow larger |
Endometriomas | Associated with endometriosis, filled with old blood | Pain, infertility, may require surgical intervention |
It’s important to know the different types of ovarian cysts to choose the right treatment. While some cysts might go away on their own, others need medical help to ease symptoms and prevent problems.
Common Causes of Ovarian Cysts
Knowing why ovarian cysts happen is key to treating them. These cysts are common and can be caused by many things.
Hormonal Imbalances
Hormonal changes are a big reason for ovarian cysts. When hormone levels change, it can mess with the ovaries. This can lead to cysts. Hormonal issues, like thyroid problems, can also raise the risk.
Polycystic Ovary Syndrome (PCOS)
Polycystic Ovary Syndrome (PCOS) is a big risk for ovarian cysts. It affects 5 to 10% of women of childbearing age. It’s marked by many cysts, hormonal imbalances, and irregular periods. Women with PCOS are more likely to get cysts because of the hormonal and metabolic issues.
Endometriosis
Endometriosis can also lead to ovarian cysts, like endometriomas. These cysts are filled with endometrial tissue and are linked to endometriosis. They can cause a lot of pain and problems, like infertility and chronic pain.
Other Medical Conditions
Other health issues can also cause ovarian cysts. Genetic factors, like a family history of cysts, can increase risk. Also, medical treatments and conditions that affect hormones can contribute to cysts.
Understanding these causes helps doctors create better treatment plans. This can improve outcomes and lower the chance of complications.
Risk Factors for Developing Ovarian Cysts
Knowing the risk factors for ovarian cysts is key to catching them early. These cysts can happen at any age. Some things can make it more likely for them to develop.
Age-Related Factors
Age is a big factor in getting ovarian cysts. Women in their reproductive years are more likely to get them. These cysts are usually linked to the menstrual cycle and often go away on their own in a few months.
Genetic Predisposition
Genetics also play a part. Women with a family history of ovarian cysts or PCOS are at higher risk. This can affect how hormones work and how the ovaries function.
Lifestyle and Environmental Factors
Lifestyle and environment can also affect the risk. While we don’t know all the causes, things like hormonal imbalances, being overweight, and certain exposures might play a role.
To better understand the risk factors, let’s examine the data in the following table:
Risk Factor | Description | Impact |
Age | Women of reproductive age | Higher likelihood of functional cysts |
Genetic Predisposition | Family history of ovarian cysts or PCOS | Increased risk due to hormonal and genetic factors |
Lifestyle Factors | Hormonal imbalances, obesity | Potential contribution to cyst formation |
By knowing these risk factors, women can take steps to protect their reproductive health. Catching and managing cysts early can greatly improve outcomes.
Growth Patterns of Ovarian Cysts
It’s important to understand how ovarian cysts grow to choose the right treatment. These cysts can be different sizes and affect women’s health in various ways.
Typical Size and Development
Ovarian cysts can be small, less than one centimeter, or very large, over 10 centimeters. Most are found by accident during a scan. They might not cause symptoms unless they’re big or not normal. Most ovarian cysts are not cancerous and can go away by themselves.
Studies show that bigger cysts are more likely to cause problems. They can lead to pain, discomfort, or other issues.
Why Do Ovarian Cysts Grow?
Many things can make ovarian cysts grow, like hormonal changes and genetics. Sometimes, cysts grow because of conditions like PCOS or endometriosis.
- Hormonal changes can make cysts grow.
- Genetics can make some women more likely to get bigger or more complex cysts.
- Medical conditions can also help cysts grow.
Resolution Rates and Timeframes
Many ovarian cysts go away by themselves. About 32% of women see their cysts disappear in a year. Around 54% of women have just one cyst left.
How fast a cyst goes away depends on its size, type, and any health issues. Regular check-ups are key to managing cysts and finding the best treatment.
- Small cysts are more likely to go away by themselves.
- Bigger or more complex cysts might need medical help.
- Keeping up with follow-up care helps track cysts.
How Ovarian Cysts Can Affect Your Period
Women with ovarian cysts often face menstrual irregularities. These cysts can mess with how the ovaries work. This can lead to irregular or missed periods. It’s important for women to understand how ovarian cysts affect their cycles.
Can Ovarian Cysts Stop Your Period Completely?
Ovarian cysts can mess with menstrual cycles. But, whether they stop periods completely depends on several factors. Functional cysts can affect hormone levels, which can impact menstruation.
Menstrual Irregularities Associated with Different Types of Cysts
Various types of ovarian cysts can cause different menstrual issues. For example, endometriomas can lead to heavy or painful periods. On the other hand, polycystic ovary syndrome (PCOS) can cause irregular ovulation and menstruation.
When to Be Concerned About Missed Periods
Missed periods are a worry for women with ovarian cysts. If you keep missing periods, see a doctor. They can check for other health issues.
Dealing with ovarian cysts and their effects on periods can be tough. If you’re seeing irregularities or have period concerns, getting medical help is key to managing your health.
Other Symptoms and Signs of Ovarian Cysts
Knowing the symptoms of ovarian cysts is key for early treatment. These cysts can show up in many ways. Being aware of these signs helps women get the care they need.
Common Symptoms
Women with ovarian cysts might feel pelvic pain, pain during sex, or trouble with bowel movements. They might also need to urinate more often, have heavy or irregular periods, feel bloated, or have a swollen tummy. These symptoms can affect daily life in different ways.
Some women feel pelvic pain or pressure, which can be dull or sharp. This pain can be constant or come and go. Pain during intercourse is also common, which can be upsetting and affect relationships.
When Symptoms Indicate a Medical Emergency
In some cases, ovarian cysts can cause serious problems like torsion or rupture. These need immediate medical help. Signs of a medical emergency include severe abdominal pain, vomiting, fever, and heavy vaginal bleeding. If a woman has these symptoms, she should go to the emergency room right away.
- Severe abdominal pain that is sudden and intense
- Vomiting or feeling nauseous
- Fever above 101.5°F (38.6°C)
- Heavy vaginal bleeding
Silent Cysts: When There Are No Symptoms
Many ovarian cysts don’t cause symptoms. They might be found during a routine check-up or imaging tests for other reasons. Even without symptoms, these cysts need to be watched to make sure they don’t cause problems.
It’s important for women with ovarian cysts to see their healthcare provider regularly. This is true even if they don’t have symptoms. Regular visits help catch any changes or issues early on.
Diagnosis of Ovarian Cysts
Healthcare providers use a multi-step approach to diagnose ovarian cysts. They aim to find out if a cyst is present and what it’s like.
Physical Examination
The first step is a physical examination. The doctor checks the patient’s overall health and the belly area for any issues.
The doctor might look for tenderness or pain in the lower belly. This could mean there’s an ovarian cyst.
Imaging Tests
If the physical exam suggests a cyst, imaging tests come next. These tests help confirm the cyst and learn more about it.
The main imaging test is the ultrasound. It uses sound waves to show pictures of the ovaries and nearby areas.
For an ultrasound, a probe is placed inside the vagina. This gives clear images of the reproductive organs.
Blood Tests and Other Diagnostic Methods
Blood tests are also used. They check for markers or hormonal levels that might show an ovarian cyst or other issues.
Other methods include pelvic exams and sometimes MRI or CT scans. These are used based on the case’s complexity.
By using these methods together, doctors can accurately diagnose ovarian cysts. They then create a treatment plan.
Treatment Options for Ovarian Cysts
Managing ovarian cysts can involve several steps, from watching them closely to surgery. The right treatment depends on the cyst’s size, symptoms, and if you’re in menopause.
Watchful Waiting
Many ovarian cysts go away on their own. Watchful waiting is often suggested for small, symptom-free cysts. This means regular ultrasounds to see if the cyst changes.
Medication Options
Some women might need medication to manage symptoms or hormonal issues. For example, birth control pills can stop new cysts from forming and shrink existing ones.
Surgical Interventions
Large, painful, or possibly cancerous cysts might need surgery. Surgery can range from removing just the cyst to taking out the ovary or even the uterus. The choice depends on your age, if you want to have kids, and the cyst’s type.
Treatment Based on Cyst Type
The cyst’s type is key in choosing treatment. For example, dermoid cysts and cystadenomas usually need to be surgically removed. But simple cysts might just need to be watched.
Cyst Type | Typical Treatment Approach | Considerations |
Functional/Physiological Cysts | Watchful waiting | Often resolve on their own; regular monitoring recommended |
Dermoid Cysts | Surgical removal | Can grow and cause complications; surgery often necessary |
Cystadenomas | Surgical removal | May require surgery due to possible growth or complications |
Knowing about ovarian cyst treatments helps women make better choices. Always talk to a healthcare provider to find the best option for you.
Natural Approaches to Managing Physiological Ovarian Cysts
Managing physiological ovarian cysts naturally means making changes in diet, lifestyle, and using complementary therapies. These steps can help reduce cysts and ease symptoms.
Dietary Modifications
Diet is key in managing ovarian cysts. Increasing fiber intake helps get rid of extra hormones. Eating foods rich in antioxidants like berries and leafy greens can also reduce inflammation.
It’s good to avoid some foods too. Cutting down on sugary foods and refined carbohydrates helps control insulin levels. This is important for women with insulin resistance or PCOS.
Lifestyle Changes
Making lifestyle changes is also important. Regular exercise can lower insulin resistance and balance hormones. Yoga and walking are great choices.
Maintaining a healthy weight is also key. Being overweight can worsen hormonal imbalances and increase cyst risk. A balanced diet and exercise can help keep a healthy weight.
Stress Management Techniques
Stress can harm hormonal balance, making stress management vital. Meditation, deep breathing, and mindfulness can help lower stress.
Doing relaxing activities like reading or listening to music can also help manage stress. These activities promote well-being.
Complementary Therapies
Complementary therapies offer extra support for managing ovarian cysts. Acupuncture can help regulate menstrual cycles and balance hormones.
Herbal supplements might also be helpful. But, it’s important to talk to a healthcare provider before starting any supplements.
By using these natural methods, women can actively manage ovarian cysts and improve their health.
Conclusion
Understanding ovarian cysts is key for women’s health. Most are harmless and go away on their own. But knowing what causes them, their symptoms, and how to treat them is important.
We’ve looked at the different types of ovarian cysts and how they affect menstrual cycles. Some cysts can cause irregularities or discomfort. But many women don’t show any symptoms at all. Knowing the risk factors and when to seek medical help is important for managing them.
Being informed about ovarian cysts helps women take care of their reproductive health. It’s also important to know that conditions like endometriosis or PCOS can lead to ovarian cysts. This shows the need for a full medical check-up.
In short, while ovarian cysts are common and usually not serious, knowing about them is essential. By staying informed and getting medical help when needed, women can keep their health in check. This includes understanding what causes cysts in the uterus and how to manage them.
FAQ
What are the causes of ovarian cysts?
Ovarian cysts can come from hormonal imbalances, PCOS, and endometriosis. Other medical conditions also play a role. Factors like genetics, age, and lifestyle can increase the risk.
How do you get an ovarian cyst?
Ovarian cysts can develop from hormonal changes, PCOS, and endometriosis. Knowing these causes helps in managing and treating them.
Can ovarian cysts stop your period?
Yes, ovarian cysts can disrupt menstrual cycles. This can lead to irregular periods or even stop them. The size and type of cyst affect the disruption.
What is the difference between physiological and pathological ovarian cysts?
Physiological cysts are part of normal ovary function and often go away on their own. Pathological cysts are abnormal and may need medical care.
Are ovarian cysts genetic?
Yes, genetics can influence the risk of ovarian cysts, like in PCOS and other family conditions.
Can cysts on the ovaries cause irregular periods?
Yes, ovarian cysts can lead to irregular periods. This includes changes in cycle length, flow heaviness, and frequency.
What are the symptoms of ovarian cysts?
Common symptoms include pelvic pain, bloating, and discomfort. Sometimes, there are no symptoms, making regular check-ups important.
How are ovarian cysts diagnosed?
Diagnosis involves a physical exam, ultrasound, and sometimes blood tests. These help determine the cyst’s nature.
What are the treatment options for ovarian cysts?
Treatment varies. Watchful waiting is for some cysts. For others, medication or surgery may be needed, based on the cyst’s type and symptoms.
Can dietary changes help manage ovarian cysts?
Yes, dietary changes, lifestyle adjustments, and stress management can help manage some cysts and symptoms.
What causes cysts in the uterus lining?
Cysts in the uterus lining are often linked to endometriosis. Hormonal influences and other growth factors are involved.
Do ovarian cysts grow, and why?
Ovarian cysts can grow due to hormones and cyst type. Understanding growth patterns helps in managing treatment plans.
Can ovarian cysts cause anechoic cysts?
Anechoic cysts, seen as fluid-filled on ultrasound, can be related to ovarian cysts, mainly the functional or physiological type.
References
National Center for Biotechnology Information. Postmenopausal Endometrial Thickness: Defining Normality. Retrieved from https://pubmed.ncbi.nlm.nih.gov/15386607/



































