Many women feel persistent pelvic pain after menopause. This can be confusing and worrying. At Liv Hospital, we know that postmenopausal ovarian discomfort is a big issue for many women going through or past menopause. Why do ovaries ache after menopause? Discover the surprising causes and the best, simple fixes for finding quick relief.
Studies show that common reasons for postmenopausal pelvic pain are ovarian cysts, uterine fibroids, and pelvic inflammatory disease. Knowing what causes postmenopausal ovary pain is key to getting the right treatment.
Key Takeaways
- Postmenopausal ovarian discomfort can arise from various causes, including ovarian cysts and uterine fibroids.
- Understanding the causes is vital for managing the discomfort.
- Liv Hospital offers a detailed, patient-focused approach to dealing with postmenopausal ovary pain.
- Getting the right diagnosis is important for effective treatment.
- Women with ongoing pelvic pain should get medical help.
Understanding Postmenopausal Ovarian Pain
Ovarian pain after menopause is a symptom that needs attention. Women go through big changes in their reproductive system during menopause. This can lead to discomfort or pain in the ovarian area.
What Happens to Ovaries After Menopause
After menopause, the ovaries stop making estrogen. The egg follicles also stop working. This big change can cause various symptoms, including pain in the ovaries.
Research shows that ovarian cysts are a common cause of pain in women going through menopause. The ovaries, once key in releasing eggs and making hormones, change after menopause. Some women may continue to feel pain, pointing to other factors.
Prevalence of Ovarian Pain in Postmenopausal Women
Many postmenopausal women feel pain in their ovaries, even though they’re not making eggs anymore. This symptom is common and needs to be understood and treated.
It’s important for doctors to know about postmenopausal ovarian pain. This way, they can give the right care and support to women who are experiencing it.
Why Do My Ovaries Ache After Menopause? Common Causes
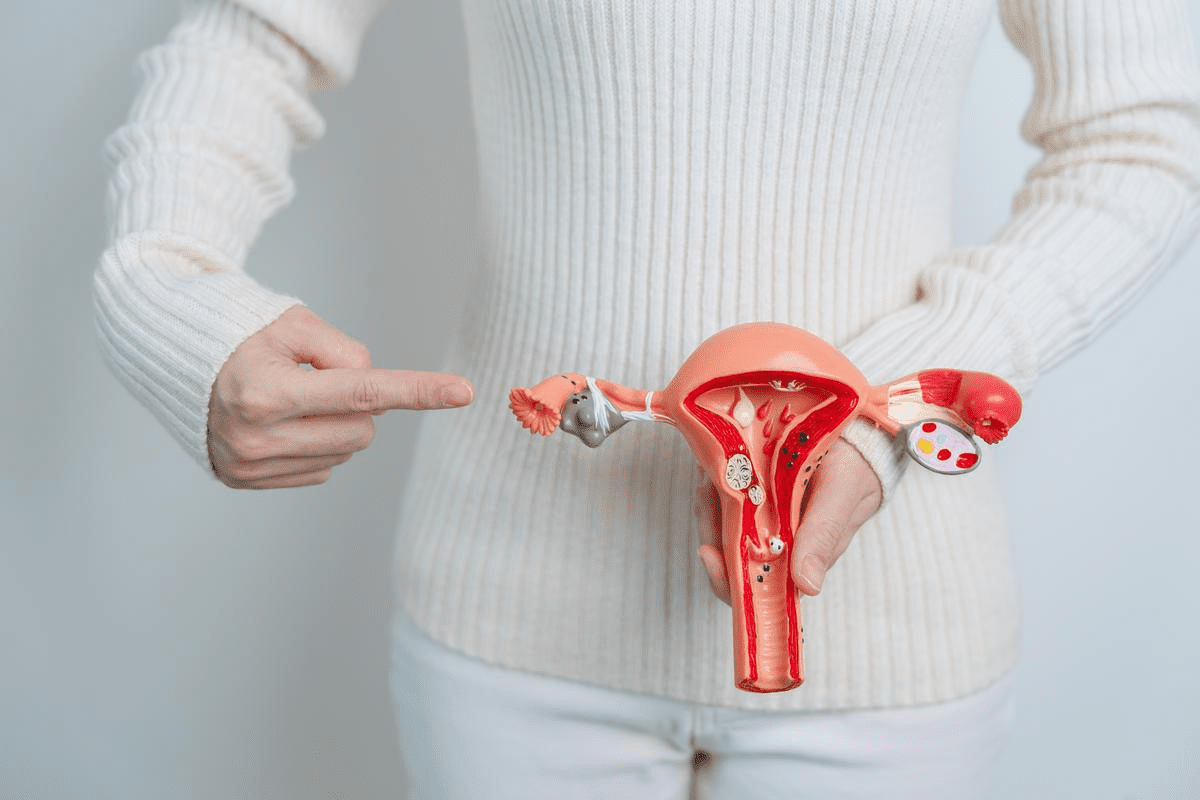
After menopause, women might feel pain in their ovaries. This pain can come from several gynecological conditions. We will look at the main reasons for this pain, like ovarian cysts, uterine fibroids, pelvic inflammatory disease, and ovarian neoplasms.
Ovarian Cysts
Ovarian cysts are a big reason for pain in postmenopausal women. They are fluid-filled sacs on the ovaries. Monitoring and sometimes surgery are needed to handle them well.
Uterine Fibroids
Uterine fibroids are non-cancerous growths in or around the uterus. They are more common during reproductive years but can also cause pain after menopause. Hormonal changes and other factors can affect their growth and symptoms.
Pelvic Inflammatory Disease
Pelvic inflammatory disease (PID) is an infection of the female reproductive organs. It’s less common after menopause but can happen, mainly with certain risk factors. PID can cause a lot of pain and needs quick medical care to avoid serious problems.
Ovarian Neoplasms
Ovarian neoplasms, or tumors, can be benign or malignant. Though less common, they are important to consider in postmenopausal women with pain. Early detection and diagnosis are key for effective treatment.
The main reasons for ovarian pain after menopause show why a detailed medical check-up is vital. By knowing these causes, doctors can create a treatment plan that fits each woman’s needs.
Serious Conditions Associated with Postmenopausal Ovarian Pain
Postmenopausal ovarian pain can signal serious health issues that need quick medical help. While it’s not always a worry, knowing the risks is key. We’ll look at serious conditions that might cause or add to ovarian pain in postmenopausal women.
Ovarian Cancer
Ovarian cancer is a big worry for postmenopausal women and can lead to pain. Though rare, it’s often caught late because its symptoms are vague. Regular check-ups and screenings are vital to catch it early.
Symptoms of ovarian cancer may include persistent bloating, abdominal pain, trouble eating, and urgent need to pee. If you’re feeling these, see your doctor right away.
Ovarian Torsion
Ovarian torsion is a rare but urgent issue that needs fast medical care. It happens when the ovary twists, cutting off blood supply. Even without function after menopause, leftover tissue or cysts can cause it.
Symptoms of ovarian torsion include sharp, severe pain in the ovary, often with nausea and vomiting. Quick diagnosis and treatment are key to avoid serious problems.
Endometriosis After Menopause
Endometriosis is usually seen in younger women, but it can also happen after menopause. Hormonal changes, like those from hormone replacement therapy, can make it worse.
Symptoms include pelvic pain, heavy bleeding, or cysts on the ovaries. Treating endometriosis after menopause often means focusing on symptom relief and managing hormones.
Pelvic Adhesions
Pelvic adhesions are fibrous tissue bands that can form between organs or the abdominal wall. They can come from surgeries, infections, or other issues, leading to pain.
Pelvic adhesions can be hard to diagnose and might need imaging or surgery to find. Treatment usually involves surgery to remove the adhesions and ease symptoms.
Knowing about these serious conditions linked to postmenopausal ovarian pain shows why seeing a doctor for ongoing or severe pain is important. Early diagnosis and treatment can make a big difference.
Distinguishing Between Left and Right Ovary Pain
Ovarian pain after menopause can be on either side. Knowing the difference is key for the right treatment. This helps doctors find the cause and treat it.
Why Left-Sided Ovary Pain Is More Common
Studies show left-sided pain is more common in postmenopausal women. Anatomical differences might play a role. The left ovarian vein’s path can lead to more pressure and pain.
Specific Causes of Right-Sided Ovary Pain
Right-sided pain is less common but needs attention. It could be due to cysts, tumors, or pelvic inflammatory disease. Finding the cause is vital for the right treatment.
When Side-Specific Pain Indicates an Emergency
Some pains are urgent and need quick action. Ovarian torsion is one, causing severe pain. It’s a serious issue that needs immediate care to avoid damage.
Characteristics | Left-Sided Ovary Pain | Right-Sided Ovary Pain |
Prevalence | More common | Less common |
Possible Causes | Venous congestion, cysts, tumors | Ovarian cysts, pelvic inflammatory disease, tumors |
Emergency Indicators | Severe pain, ovarian torsion | Severe pain, ovarian torsion, appendicitis |
It’s important to know the difference between left and right ovary pain. If you have persistent or severe pain, see a doctor. They can help find the cause and treat it.
Types of Ovarian Pain Sensations After Menopause
Women often feel different kinds of pain in their ovaries after menopause. These can range from sharp to aching. Knowing what these feelings mean is key to finding out why and getting the right help.
Sharp vs. Aching Pain
Ovarian pain can feel sharp or aching. Sharp pain is sudden and intense. It might mean something serious like an ovarian torsion or a ruptured cyst. On the other hand, aching pain is more ongoing and could be due to things like pelvic adhesions or endometriosis.
Knowing if pain is sharp or aching helps doctors figure out what’s wrong. Sharp pain might need quick medical care. Aching pain might need more tests to find the cause.
Intermittent vs. Constant Discomfort
Ovarian pain can also be either intermittent or constant. Intermittent pain comes and goes, and its intensity can change. This might be linked to things like ovarian cysts that can rupture or change size. Constant pain, on the other hand, lasts longer and could be a sign of chronic issues like endometriosis or pelvic inflammatory disease.
Knowing if pain is intermittent or constant helps narrow down what might be causing it. It also helps decide the best treatment plan.
Pain Accompanied by Other Symptoms
In some cases, ovarian pain after menopause comes with other symptoms. These can include bloating, feeling like the belly is swollen, or abnormal vaginal bleeding. These symptoms can give clues about what’s causing the pain.
For example, pain with bloating and swelling could mean ovarian cancer. This is a serious issue that needs quick medical attention.
Type of Pain | Possible Causes | Associated Symptoms |
Sharp Pain | Ovarian torsion, ruptured cyst | Sudden onset, severe pain |
Aching Pain | Pelvic adhesions, endometriosis | Pelvic discomfort, heavy feeling |
Intermittent Pain | Ovarian cysts | Bloating, pelvic pressure |
Constant Pain | Endometriosis, pelvic inflammatory disease | Continuous discomfort, pelvic pain |
Diagnosing the Cause of Postmenopausal Ovarian Pain
Figuring out why women get ovarian pain after menopause is complex. It involves looking at many things. We need to find out what’s causing the pain.
Physical Examination
The first step is a physical check-up. A doctor will look at the whole body and the pelvic area. This can show if there’s something wrong, like tenderness or a mass.
Imaging Tests
Imaging tests are key in finding the cause of pain. They include:
- Ultrasound: Shows the ovaries and can spot cysts or tumors.
- CT Scan: Gives detailed pictures of the pelvic area. It can find issues like ovarian torsion or tumors.
- MRI: Gives clear images for complex cases.
Blood Tests and Tumor Markers
Blood tests are also important. They help find the cause of pain. Tests may include:
- Complete Blood Count (CBC): Looks for signs of infection or inflammation.
- Tumor Markers: Like CA-125, which can show ovarian cancer.
- Hormone Levels: Checks for hormonal imbalances that might cause pain.
These tests give important info. When combined with imaging, they help find the cause of pain.
Diagnostic Procedures
Sometimes, more tests are needed. These can include:
- Laparoscopy: A small surgery to see the pelvic organs.
- Biopsy: If a mass is found, it’s checked for cancer.
These tests are vital when other methods don’t work. They help find the exact cause and guide treatment.
By using physical exams, imaging, blood tests, and more, doctors can find the cause of pain. Then, they can create a good treatment plan.
Treatment Options for Ovarian Pain After Menopause
Managing ovarian pain after menopause needs a detailed plan. The right treatment depends on the pain’s cause, how bad it is, and your health.
Medication Approaches
For many, the first step is medication. Nonsteroidal anti-inflammatory drugs (NSAIDs) help with pain and swelling. Hormone therapy might also be suggested if the pain is due to hormone changes.
Other options include pain modulators or antidepressants for chronic pain. Always talk to your doctor about the best medicine and how much to take.
Surgical Interventions
If pain is from something like ovarian cysts or uterine fibroids, surgery might be needed. The type of surgery depends on the problem.
Laparoscopic surgery can remove cysts or fix other pain causes. Sometimes, removing the uterus or ovaries is considered, but it’s rare.
Hormone Therapy Considerations
Hormone therapy can help with pain caused by hormone changes after menopause. Estrogen therapy can stabilize hormone levels and ease symptoms.
But, hormone therapy isn’t right for everyone and has risks. Always talk to your doctor about the pros and cons.
Alternative and Complementary Treatments
Many women find relief with alternative and complementary therapies. These include acupuncture, herbal supplements, yoga, and mindfulness.
These methods can be helpful, but check with your doctor first. They need to make sure they’re safe and won’t interfere with other treatments.
Exploring different treatments and talking to your doctor can help you manage ovarian pain after menopause.
Prevention and Lifestyle Modifications
Regular health check-ups, a balanced diet, and stress management can prevent ovarian pain after menopause. These steps help reduce the risk of ovarian pain and improve life quality.
Regular Health Screenings
Regular health screenings are key for early detection and management of conditions that may lead to ovarian pain. We suggest annual check-ups with your healthcare provider. These should include pelvic exams and ultrasounds to monitor ovarian health.
Diet and Exercise Impact
Keeping a healthy lifestyle through diet and exercise can help prevent ovarian pain. Eating a balanced diet rich in fruits, vegetables, and whole grains is important. Regular physical activity helps manage weight and reduces the risk of conditions like uterine fibroids and ovarian cysts.
Nutritional Recommendations:
- Increased intake of omega-3 fatty acids
- High consumption of antioxidant-rich foods
- Adequate hydration
Exercise Guidelines:
- At least 150 minutes of moderate-intensity aerobic exercise per week
- Incorporating strength training exercises twice a week
- Flexibility and balance exercises, such as yoga or Pilates
Stress Management Techniques
Stress can make ovarian pain worse, so managing it is key. Techniques like mindfulness meditation, deep breathing exercises, and progressive muscle relaxation can help. They reduce stress levels.
Exploring alternative therapies like acupuncture and massage therapy can also help. These have been shown to reduce stress and improve well-being.
Supplements and Natural Remedies
Certain supplements and natural remedies may help with ovarian pain. But, it’s important to talk to your healthcare provider before trying any new supplements.
Supplement/Natural Remedy | Potential Benefits |
Omega-3 fatty acids | Anti-inflammatory properties |
Turmeric/Curcumin | Anti-inflammatory and antioxidant effects |
Vitamin D | Regulation of calcium levels and bone health |
By following these preventive measures and lifestyle changes, women can lower their risk of ovarian pain after menopause. It’s important to work with healthcare providers to create a personalized prevention plan.
Conclusion
Ovarian pain after menopause can be very worrying and painful. Understanding what causes it and how to treat it can help women feel better. This can greatly improve their life quality.
We looked at why ovaries might hurt during menopause. This includes things like ovarian cysts and serious conditions like ovarian cancer. It’s important to know if the pain is on the left or right side and what it feels like.
Figuring out why ovaries hurt involves several steps. Doctors use physical exams, imaging tests, and blood tests. Treatment can include medicines, surgery, hormone therapy, and other options.
Women can also try to manage their pain by changing their lifestyle. Eating well, exercising, and managing stress can help. By understanding and managing ovarian pain, women can take back control of their health.
We hope this information helps women who are worried about ovarian pain after menopause. By getting medical help and trying different treatments, women can reduce their pain and live better lives.
FAQ
What are the common causes of ovarian pain after menopause?
Ovarian pain after menopause can stem from several sources. These include ovarian cysts, uterine fibroids, and pelvic inflammatory disease. Ovarian neoplasms are also a possible cause. Knowing these can help figure out the right treatment.
Can ovarian pain after menopause be a sign of a serious condition?
Yes, it can signal serious issues like ovarian cancer or ovarian torsion. Other conditions like endometriosis and pelvic adhesions can also cause pain. It’s vital to get medical help quickly to find out why.
Why does ovarian pain occur on one side, and what does it indicate?
Ovarian pain can happen on either side. The side it occurs on might hint at the cause. Left-sided pain is more common, but right-sided pain can point to specific issues needing medical attention.
What are the different types of ovarian pain sensations after menopause?
Ovarian pain can feel sharp or aching. It might come and go or stay constant. The kind and how long it lasts can give clues about what’s causing it.
How is the cause of ovarian pain after menopause diagnosed?
Figuring out why ovarian pain happens after menopause involves several steps. These include physical exams, imaging tests, blood tests, and other procedures.
What are the treatment options for ovarian pain after menopause?
Treatment for ovarian pain after menopause varies based on the cause. It might include medicines, surgery, hormone therapy, or alternative therapies.
Can ovarian pain after menopause be prevented?
Not all ovarian pain after menopause can be prevented. But, regular health checks, healthy living, and managing stress can lower the risk.
How do diet and exercise impact ovarian pain after menopause?
Eating well and exercising regularly can help with ovarian pain. They reduce inflammation and improve health, making you feel better overall.
Are there any supplements or natural remedies that can help with ovarian pain after menopause?
Some supplements and natural remedies might ease ovarian pain after menopause. But, it’s important to talk to a doctor before trying them.
What is the significance of accompanying symptoms with ovarian pain after menopause?
Other symptoms like bloating or vaginal bleeding can help figure out why you’re in pain. They give clues about what might be causing the pain.
Can stress management techniques help with ovarian pain after menopause?
Yes, managing stress can help with ovarian pain. Techniques like meditation, yoga, or deep breathing can reduce stress and ease pain.
How often should I have health screenings to detect possible causes of ovarian pain after menopause?
Regular health checks, including pelvic exams and imaging, can spot possible causes of pain. How often you need these depends on your risk factors and medical history.
References
National Health Service (NHS). Postmenopausal Ovarian Pain: Causes and Considerations. Retrieved from https://www.nhs.uk/conditions/pelvic-inflammatory-disease-pid/