Many women feel ovarian pain as they get closer to menopause. This symptom can be both unsettling and confusing. As the body goes through big hormonal changes, it’s common for women to feel discomfort or pain in their ovaries.
During perimenopause and menopause, hormonal changes can cause ovarian discomfort. This discomfort can be mild or severe. It’s important to understand the causes of this pain to get the right care and relief. Experiencing ovary discomfort during menopause? Get the key facts on why it happens and discover powerful strategies for relief.
Ovarian pain can really affect a woman’s quality of life. Our healthcare providers are here to offer caring, evidence-based help. They aim to support women through this big life change.
Key Takeaways
- Ovarian pain is a common concern during menopause and perimenopause.
- Hormonal fluctuations can cause ovarian discomfort.
- Ovarian pain can range from mild to severe.
- Understanding the causes is key for proper care and relief.
- Compassionate, evidence-based treatment is available.
The Menopausal Transition and Your Ovaries
The menopausal transition is a complex process. It involves hormonal shifts that affect ovarian function. As women approach menopause, their ovaries change significantly. These changes can cause discomfort or pain.
Physiological Changes in Ovarian Function
During menopause, the ovaries produce fewer hormones, like estrogen. Estrogen is key for menstrual cycles. The drop in estrogen levels is a main reason for ovarian pain during perimenopause and menopause. This hormone drop can also change the ovarian tissue, causing discomfort.
Some key changes include:
- A decrease in estrogen production
- Alterations in ovarian follicle development
- Changes in the structure and function of the ovaries
These changes can lead to ovary discomfort or pain. Women may feel this during the menopausal transition.
Timeline of Hormonal Shifts
Hormonal changes during menopause don’t happen quickly. They are part of a gradual process that can start years before menopause. This period, known as perimenopause, is marked by fluctuating hormone levels. This can cause various symptoms, including menopause and ovary discomfort.
The timeline of hormonal shifts varies among women. But generally, it follows this pattern:
- Perimenopause: Hormone levels start to fluctuate, causing irregular menstrual cycles and possible ovarian pain.
- Menopause: It’s marked by the end of menstrual cycles and a big drop in estrogen levels.
- Post-menopause: Hormone levels stabilize at a lower level. But some women may continue to feel ovarian discomfort.
Knowing these changes can help women navigate the menopausal transition better. It can also help them manage symptoms like ovarian pain.
Ovary Discomfort During Menopause: What You Need to Know
Menopause brings big changes to the ovaries, causing discomfort. It’s important for women to know about ovarian pain during this time. We’ll look at how common it is, what it feels like, and when to worry.
How Common is Ovarian Pain During Menopause?
Ovarian pain is more common than you might think during menopause. Many women feel pelvic or ovarian discomfort. Hormonal changes and ovarian function shifts are big reasons why.
Characteristics of Menopausal Ovarian Pain
Ovarian pain can feel different for everyone. Some feel sharp pains, while others have dull aches. The pain might come and go or stay the same, affecting one or both ovaries.
The Difference Between Normal Discomfort and Concerning Pain
It’s key to tell normal discomfort from pain that’s a worry. Normal pain can often be managed with lifestyle changes. But, if the pain is severe, lasts a long time, or comes with other symptoms like heavy bleeding or fever, see a doctor.
Many things can cause pain in the ovaries during menopause. Knowing what these are can help figure out the cause of the pain.
Condition | Description | Symptoms |
Hormonal Imbalance | Changes in estrogen and progesterone levels | Hot flashes, mood swings, ovarian pain |
Ovarian Cysts | Fluid-filled sacs on the ovaries | Pelvic pain, bloating, discomfort during sex |
Endometriosis | Tissue similar to uterine lining outside the uterus | Pelvic pain, heavy bleeding, infertility |
Perimenopause vs. Menopause: When Ovarian Pain Most Commonly Occurs
The transition to menopause, known as perimenopause, can bring about significant changes in ovarian activity, potentially leading to pain. Understanding when ovarian pain is most likely to occur during this transition is key to managing symptoms effectively.
Perimenopause: The Storm Before the Calm
Perimenopause is the transitional period leading up to menopause, during which hormone levels fluctuate significantly. This phase can last several years and is characterized by unpredictable ovarian activity, which may lead to ovarian pain. The hormonal fluctuations during perimenopause can cause changes in ovulation patterns, potentially resulting in discomfort or pain.
Post-Menopause: Can Ovaries Stil Cause Discomfort?
After menopause, the ovaries typically cease to produce eggs, and hormone production decreases significantly. Yet, some women may experience ovarian pain or discomfort. While the frequency and intensity may decrease compared to perimenopause, understanding the causes of post-menopausal ovarian pain is essential for proper management.
Characteristics | Perimenopause | Post-Menopause |
Hormonal Fluctuations | Significant and unpredictable | Generally decreased |
Ovarian Activity | Unpredictable, may cause pain | Ceased or significantly reduced |
Frequency of Ovarian Pain | More common due to hormonal changes | Less common, but possible |
In conclusion, ovarian pain can occur during both perimenopause and post-menopause, though the frequency and causes may vary. Understanding these differences is key to managing ovarian health during the menopausal transition.
The Hormonal Rollercoaster: How Fluctuations Trigger Ovarian Pain
During menopause, the drop in estrogen levels is a big reason for ovarian pain. As women go through menopause, hormone levels like estrogen and progesterone change a lot. These changes can hurt the ovaries and cause pain.
Estrogen’s Role in Ovarian Discomfort
Estrogen is key to keeping the ovaries healthy. When estrogen levels drop in menopause, the ovaries can change and feel uncomfortable. Studies show that estrogen helps fight inflammation, which can reduce pain. So, when estrogen levels go down, the ovaries might feel more pain.
Estrogen’s effects on ovarian pain can be summarized as follows:
- Regulation of inflammatory responses
- Maintenance of ovarian tissue health
- Influence on pain perception pathways
Progesterone Changes and Their Effects
Progesterone levels also change a lot during menopause. These changes can mess with how the ovaries work and cause pain. Progesterone helps relax the uterus. When it goes away, the uterus can get active again, causing pain that can spread to the ovaries.
“Hormonal fluctuations, like the drop in estrogen and changes in progesterone, are key in causing ovarian pain during menopause.”
The Science Behind Hormone-Related Pain
The link between hormones and pain is complex. Hormones like estrogen and progesterone affect how we feel pain, from the brain to the body. Knowing how these hormones work can help us understand why some women feel more pain in their ovaries during menopause.
Hormone | Effect on Ovarian Pain |
Estrogen | Decline contributes to increased pain sensitivity |
Progesterone | Fluctuations can lead to increased uterine activity and referred pain |
Primary Causes of Ovarian Pain During the Menopausal Transition
Several primary factors contribute to ovarian pain during the menopausal transition. Understanding these causes is essential for women to navigate this significant life change.
Hormonal Imbalance Mechanisms
Hormonal fluctuations play a big role in ovarian pain during menopause. As estrogen and progesterone levels change, women may feel discomfort. The decline in estrogen levels, in particular, can lead to changes in the ovarian tissue, potentially causing pain.
The hormonal changes during menopause can be broken down into several key mechanisms:
- Decrease in estrogen production
- Fluctuations in progesterone levels
- Changes in the feedback loop between the hypothalamus, pituitary gland, and ovaries
Changes in Ovulation-Related Pain
During the menopausal transition, ovulation becomes less predictable and eventually ceases. The period leading up to this cessation can be associated with changes in ovulation-related pain. Some women may experience more pronounced pain due to the irregular ovulation cycles.
Other symptoms associated with ovarian cysts, which can occur during this time, include:
- Pelvic pain
- Bloating
- Painful intercourse
Referred Pain from Surrounding Structures
Referred pain is another significant factor to consider when evaluating ovarian pain during menopause. Pain from surrounding structures like the uterus, fallopian tubes, or even the lower back can be referred to the ovarian area.
Conditions such as uterine fibroids or endometriosis can cause pain that is perceived in the ovarian region. It’s essential to consider these possible sources when assessing ovarian pain.
By understanding the various factors that contribute to ovarian pain, women and healthcare providers can better address the discomfort associated with the menopausal transition.
Medical Conditions That May Cause or Woren Menopausal Ovarian Pain
Health issues like ovarian cysts and endometriosis can lead to pain in the ovaries for menopausal women. It’s key to know how different health problems can affect the ovaries and cause pain during menopause.
Ovarian Cysts: Prevalence and Presentation During Menopause
Ovarian cysts can appear after menopause and may cause pain and other symptoms. Most ovarian cysts are not cancerous, but they can be very painful. It’s important to seek medical help if you have ovarian cysts.
Not much research has been done on ovarian cysts in menopausal women. But, it’s known that older women are more likely to have complex cysts. These cysts can lead to pelvic pain, bloating, and other symptoms that might be mistaken for menopause symptoms.
Endometriosis in Perimenopause and Beyond
Endometriosis is when tissue like the uterine lining grows outside the uterus, causing pain. Symptoms of endometriosis may lessen after menopause, but some women can continue to feel pain. This is because some tissue might remain.
During perimenopause, hormonal changes can make endometriosis symptoms worse. It’s important to know that endometriosis can start or get worse during this time, leading to a lot of discomfort.
Uterine Fibroids and Their Impact on Surrounding Tissues
Uterine fibroids are non-cancerous growths in or around the uterus. They can cause pelvic pain, heavy bleeding, and other symptoms. Even though fibroids often shrink after menopause, they can cause pain during the transition.
Fibroids can press on nearby tissues and organs, causing pain that might feel like it’s coming from the ovaries. We should think about fibroids as a possible cause of pelvic pain during menopause.
Other Potencial Pathologies to Consider
Other conditions, such as pelvic inflammatory disease (PID), adhesions, and ovarian remnant syndrome, can also cause ovarian pain during menopause. PID is more common in younger women but can happen in menopausal women too, if they’ve had pelvic infections before.
We need to look at these other conditions when trying to figure out why menopausal women have ovarian pain. Getting a full diagnosis is key to finding the right treatment.
Recognizing Ovarian Pain: Symptoms and Patterns
It’s important to know the signs of ovarian pain to get help quickly. During menopause, ovarian pain can show up in different ways. Women need to know the signs and what they mean.
Location and Characteristics of Ovarian Pain
Ovarian pain usually feels in the lower belly, often on one side. But it can be on both sides too. The pain can be sharp, dull, or crampy and may stay the same or change.
Some women feel pain that spreads to their lower back or thighs. The pain can be different for everyone. It’s key to watch and understand your own pain patterns.
Associated Symptoms to Watch For
There are other associated symptoms to look out for. These include bloating, tender belly, and changes in bowel or urination habits. Ovarian pain might also come with hot flashes or mood swings.
Seeing these symptoms can mean there’s a bigger issue that needs a doctor’s check-up.
“Accurate diagnosis of ovarian pain involves understanding its relationship with other symptoms and overall health context.” Medical Expert, Gynecologist
Distinguishing Ovarian Pain from Other Abdominal Discomfort
It can be hard to tell if it’s ovarian pain or something else. Issues like appendicitis, irritable bowel syndrome, or muscle problems can cause similar pain. So, a detailed medical history and physical check are very important.
Characteristics | Ovarian Pain | Other Abdominal Discomfort |
Location | Typically one-sided, lower abdomen | Varies, can be diffuse or localized |
Nature of Pain | Sharp, dull, or crampy | Can be sharp, dull, crampy, or burning |
Associated Symptoms | Bloating, changes in urination | Nausea, vomiting, changes in bowel habits |
Knowing the differences and what ovarian pain characteristics are can help women get the right medical care.
When to Consult a Healthcare Provider About Menopausal Ovarian Pain
Ovarian pain during menopause can be worrying. It’s key to know when to see a doctor. Knowing the signs that mean you need a medical check-up is important.
Red Flags That Require Immediate Medical Attention
Some symptoms with ovarian pain in menopause are serious. They need you to see a doctor right away. These include:
- Severe or getting worse pain over time
- Bleeding after 12 months without a period
- Pelvic pain with fever or stomach problems
These signs might mean you have a serious health issue. You should get medical help fast.
Persistent Symptoms That Warrant Evaluation
Some symptoms that keep happening need a doctor’s check-up. They’re not as urgent but are important. These include:
- Ovarian pain that keeps coming back
- Pain that changes in pattern or gets stronger
- Other symptoms like bloating or changes in urination
Looking into these symptoms can find the cause. It can also help find the right treatment.
Questions to Prepare Before Your Appointment
Getting ready for your doctor’s visit is smart. Think about asking:
- What could be causing my ovarian pain?
- Do I need any special tests or exams?
- What treatments are there for my condition?
Symptom | Action Required |
Severe or worsening pain | Immediate medical attention |
Post-menopause bleeding | Immediate medical evaluation |
Pelvic pain with fever or GI distress | Urgent medical care |
Knowing when to get medical help for ovarian pain in menopause is vital. Spotting red flags and ongoing symptoms is key. Being ready for your doctor’s visit helps get the right care and support.
Diagnostic Approaches for Ovarian Pain in Menopausal Women
Diagnosing ovarian pain in menopause requires a detailed strategy. This includes looking at medical history, physical exams, and advanced imaging. This thorough method helps find the cause of pain and plan treatment.
Medical History and Physical Examination
The first step is a detailed medical history and physical exam. Doctors will ask about symptoms and past health. They also do a pelvic exam to check the reproductive organs.
Key components of the medical history include:
- Detailed description of the pain, including its location, intensity, and duration
- Menstrual history and any changes in menstrual patterns
- Previous gynecological conditions or surgeries
- Family history of ovarian or breast cancer
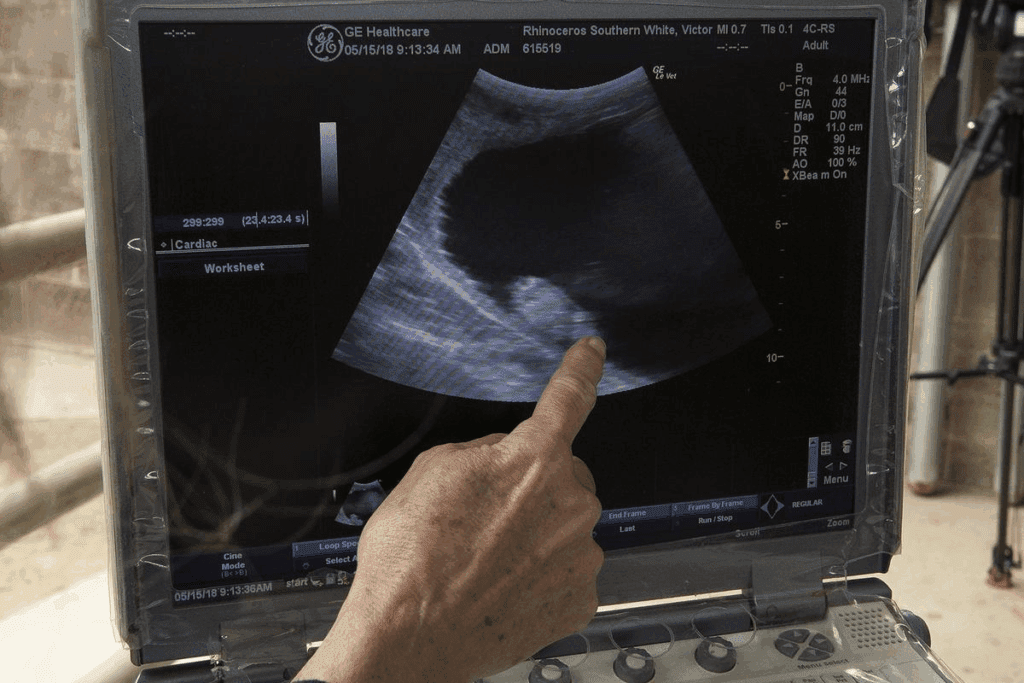
Imaging Studies: Ultrasound, CT, and MRI
Imaging studies are key in finding the cause of ovarian pain. Ultrasound is often the first choice to look at the ovaries. It can spot cysts, tumors, or other issues.
At times, CT or MRI scans are needed for more detailed views. They help see the ovaries and nearby tissues better.
Laboratory Tests and Biomarkers
Laboratory tests help rule out other pain causes and check overall health. These tests include:
- Blood tests for infection or inflammation signs
- Hormone tests to check balance
- Tumor markers like CA-125 for ovarian cancer screening
Ruling Out Serious Conditions
It’s important to rule out serious conditions that need quick attention. Doctors watch for signs of serious issues like ovarian torsion or ruptured cysts.
Red flags that require immediate evaluation include:
- Severe, sudden pain
- Abdominal tenderness or guarding
- Fever or signs of infection
- Abnormal vaginal bleeding
By using a detailed diagnostic approach, doctors can find the cause of ovarian pain in menopausal women. They then create a good treatment plan.
Treatment Options and Management Strategies
Women going through menopause need to know about treatments for ovarian pain. This is key to better living. Managing ovarian pain in menopause requires a mix of medical treatments and lifestyle changes.
Hormone Replacement Therapy: Benefits and Risks
Hormone replacement therapy (HRT) is a top choice for easing menopause symptoms, like ovarian pain. It adds estrogen and progesterone to the body. This can lessen symptoms caused by hormone changes. But, it’s important to think about the risks, like blood clots and cancer.
Women should talk to their doctor about their health and risks. HRT can greatly help with ovarian pain and other symptoms, making life better.
Pain Management Approaches
Managing pain is key in menopause. There are many ways to do this, like over-the-counter drugs, prescription meds, and other therapies. NSAIDs are often first tried for mild to moderate pain.
For more serious pain, doctors might suggest stronger meds or other treatments. It’s important to work with a doctor to find the best pain relief plan with few side effects.
Lifestyle Modifications That May Provide Relief
Changing your lifestyle can help with ovarian pain in menopause. Eating more omega-3s and antioxidants can help with pain. Also, exercises like yoga and tai chi can help.
Stress management, like meditation, can also help with pain. Making these lifestyle changes can improve your overall health and reduce pain.
Alternative and Complementary Therapies
Some women try alternative therapies for ovarian pain in menopause. This includes acupuncture, herbal supplements, and mind-body therapies. While some find these helpful, it’s important to talk to a doctor first to make sure they’re safe and work well.
Exploring different treatments and strategies can help women find relief from ovarian pain. It’s about finding what works best and working with doctors to create a plan that’s just right.
Conclusion: Navigating Ovarian Health Through the Menopausal Journey
Understanding ovarian health during menopause is key to managing symptoms and improving life quality. Ovarian pain is a big concern for many women during this time.
Managing ovarian pain needs a full approach. This includes knowing its causes, recognizing symptoms, and looking at treatment options. By understanding the changes in menopause, we can face the challenges of ovarian health better.
Empowering women with knowledge about their ovarian health helps them manage symptoms better. We urge women to talk to their healthcare providers. This way, they can create a plan for managing ovarian pain and improving overall well-being during menopause.
FAQ
Can ovaries hurt during menopause?
Yes, many women feel pain in their ovaries during menopause. This pain can come from changes in hormones.
What causes ovarian pain during menopause?
Hormonal changes and shifts in ovulation pain are main causes. Pain can also spread from nearby areas.
How common is ovarian pain during menopause?
Ovarian pain is common during menopause. It affects many women, but to different extents.
Is ovarian pain during menopause a normal symptom?
Some discomfort is normal. But, it’s key to know when pain is a sign of something serious.
Can perimenopause cause ovary pain?
Yes, hormonal changes in perimenopause can lead to ovary pain. Symptoms are similar to menopause.
What are the characteristics of menopausal ovarian pain?
Pain can feel like a dull ache or sharp stabbing. It often happens in the lower abdomen or pelvis.
When should I consult a healthcare provider about menopausal ovarian pain?
See a doctor for persistent or severe pain. Also, if you have heavy bleeding, fever, or trouble urinating.
How is ovarian pain diagnosed in menopausal women?
Doctors use a detailed medical history and physical exam. They might also do imaging and lab tests.
What are the treatment options for ovarian pain during menopause?
Treatments include hormone therapy and pain management. Lifestyle changes and alternative therapies are also options.
Can ovarian cysts cause pain during menopause?
Yes, cysts can cause pain during menopause. But, their occurrence may decrease after menopause.
How can I manage ovarian pain during menopause?
Managing pain involves medical treatments, lifestyle changes, and alternative therapies. These can help reduce symptoms and improve life quality.
Are there any underlying medical conditions that can cause or worsen ovarian pain during menopause?
Yes, conditions like endometriosis and uterine fibroids can cause or worsen pain during menopause.
References
National Center for Biotechnology Information. Ovarian Pain During Menopause: Causes and Understanding. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK507826/








