
Did you know that medical technology has made pacemakers last longer and work better? Pacemaker battery life is now a key part of heart care.
Thinking about getting a pacemaker battery replacement can be scary. But knowing when to replace a pacemaker battery is important for heart health. How often you need to replace it depends on the pacemaker type and your health.
As we keep making pacemaker technology better, it’s important to know the latest news. This includes understanding the average pacemaker battery life and when you might need a new one.
Key Takeaways
- Pacemaker technology has advanced significantly, improving battery life.
- The frequency of pacemaker battery replacement varies based on individual health and device type.
- Understanding the signs for replacement is key for heart health.
- Medtronic PLC is a leading innovator in pacemaker technology.
- Staying informed about pacemaker advancements is essential for patients.
Understanding Pacemakers and Their Purpose
Pacemakers are devices that help control the heartbeat. They send electrical impulses to keep the heart beating at a steady rate. These devices are key for people with heart rhythm problems.
What is a Pacemaker and How Does it Work?
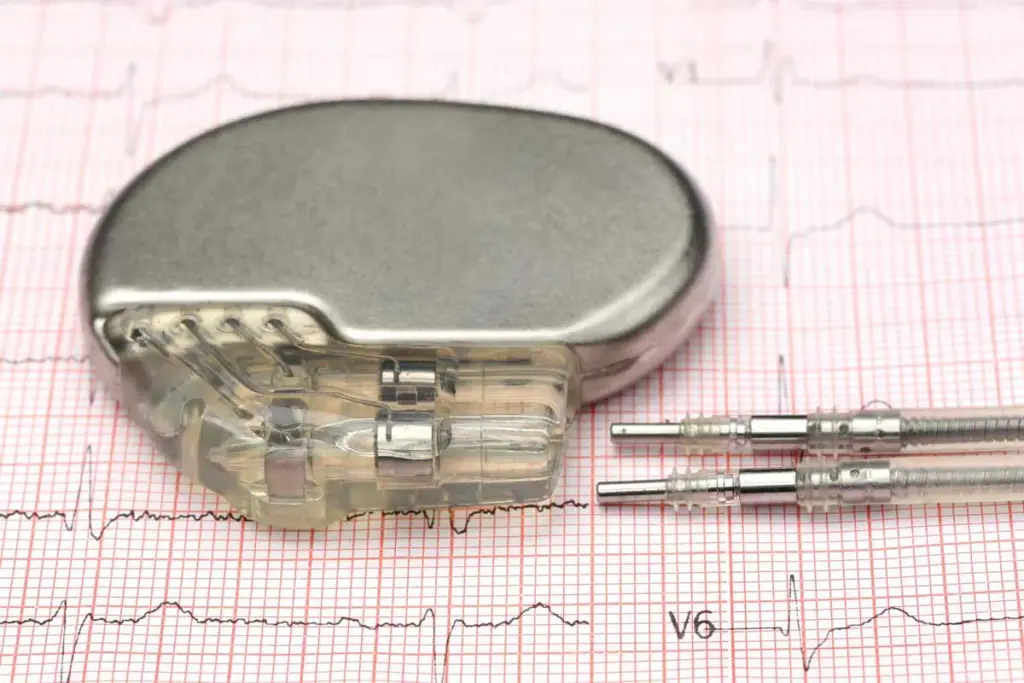
A pacemaker is a small device placed under the skin, usually near the collarbone. It has two main parts: the pulse generator and the leads. The pulse generator has the battery and the circuitry that controls the pacing. The leads are wires that connect the pulse generator to the heart, sending the impulses.
The pacemaker watches the heart’s rhythm and sends impulses when needed. This keeps the heart beating steadily. It helps prevent symptoms like dizziness, fatigue, and shortness of breath caused by irregular heart rhythms.
Types of Pacemakers Available Today
There are many types of pacemakers, each for different heart rhythm needs. Single-chamber pacemakers have one lead and pace one chamber of the heart. Dual-chamber pacemakers have two leads, pacing both the atrium and ventricle for better coordination.
Biventricular pacemakers, or CRT devices, are for heart failure patients. They have three leads to synchronize ventricle contractions, boosting heart efficiency.
New advancements have brought leadless pacemakers. These small devices are implanted directly in the heart, without leads. These innovations help manage heart rhythm disorders better.
The Lifespan of Modern Pacemakers
Modern pacemakers have seen big improvements in how long they last. They are now more efficient and durable. This means patients can live better lives with these devices.
Average Longevity of Different Pacemaker Models
The lifespan of a pacemaker depends on its model and maker. Most last between 5 to 15 years. But, the newest ones with better batteries can last up to 20 years or more.
Each pacemaker model has its own features that affect how long it lasts. Here’s a table showing how long different models last on average.
|
Pacemaker Model |
Average Longevity (Years) |
|---|---|
|
Medtronic Azure |
14-16 |
|
Boston Scientific Resonate |
13-15 |
|
St. Jude Medical Ellipse |
12-14 |
Factors Affecting Pacemaker Durability
Many things can affect how long a pacemaker lasts. These include the patient’s lifestyle, the device’s technology, and how well it’s cared for. For example, active patients might need more pacing, which can shorten battery life.
Electrophysiology cardiology is key in caring for pacemaker patients. Regular check-ups and monitoring can spot problems early. This keeps the device working well.
Knowing what affects a pacemaker’s lifespan is important. Selecting the appropriate device and ensuring regular maintenance can help patients lead longer, healthier lives with their pacemaker.
Pacemaker Battery Life Explained
For those with pacemakers, knowing about battery life is key. It affects how well the device works and how often you need to see a doctor. Understanding this can improve your life and reduce medical visits.
How Long Do Pacemaker Batteries Typically Last?
Pacemaker batteries are made to last a long time, from 5 to 15 years. Regular checks help figure out when it’s time for a new one.
” “But, how long they last can change based on the pacemaker type, settings, and how active you are.”
Variables That Impact Battery Longevity
Several things can affect how long a pacemaker battery lasts. These include:
- The type of pacemaker and its settings
- The patient’s heart condition and how often the pacemaker needs to intervene
- The patient’s overall health and activity level
An electrophysiology study helps see how well the pacemaker is working. It shows when a battery might need to be replaced. This test lets doctors check the heart’s electrical activity and adjust the pacemaker to save battery life.
By knowing these factors and getting regular check-ups, patients and doctors can manage battery life better. This ensures timely replacements and reduces risks.
Signs That Your Pacemaker Battery Needs Replacement
Knowing when your pacemaker battery is running low is key to staying healthy. As someone with a pacemaker, spotting the signs of a battery needing a swap is vital. It helps avoid problems and keeps your device working right.
Physical Symptoms to Watch For
Even though pacemakers are reliable, some signs show your battery is running low. Look out for:
- Fatigue or Weakness: Feeling very tired or lacking energy.
- Dizziness or Lightheadedness: Feeling dizzy or like you might faint.
- Shortness of Breath: Having trouble breathing or feeling winded easily.
- Swelling in the Legs or Feet: Fluid buildup could mean your pacemaker isn’t working right.
- Palpitations or Irregular Heartbeats: Noticing your heart beats irregularly or skips beats.
If you notice any of these symptoms, reach out to your doctor right away. They can check your pacemaker and see if it needs a new battery.
How Doctors Monitor Pacemaker Battery Status
Regular visits with your doctor are important for checking your pacemaker’s battery. They use different methods to check your pacemaker’s health, like:
- Interrogation Device: A tool that talks to your pacemaker to check its status and battery level.
- Electrocardiogram (ECG): A test that looks at your heart’s electrical activity to make sure it’s working well.
- EP Lab Tests: Sometimes, more detailed tests are done in an Electrophysiology (EP) lab to closely watch your heart and pacemaker.
Your healthcare team keeps an eye on your pacemaker’s battery to find the best time for a replacement. This ensures your device keeps managing your heart rhythm well.
The Pacemaker Battery Replacement Process
Learning about pacemaker battery replacement can ease your worries. It’s a minor surgery that needs careful planning and aftercare. We’ll walk you through it, from getting ready to recovering, and why follow-up care is key.
Pre-Procedure Preparation
Your healthcare team will give you specific instructions before the surgery. You might need to stop certain medicines, find a driver, and fast for a while. It’s vital to follow these steps to avoid risks.
a top cardiologist, says, “Being prepared is essential for a smooth pacemaker battery replacement. By following your doctor’s advice and asking questions, you can make the process easier.”
“The more prepared you are, the less stressful the experience will be.”
What Happens During the Replacement Surgery
The surgery involves several steps. First, you’ll get local anesthesia to numb the area. The procedure is done under conscious sedation to keep you relaxed. Your doctor will then make a small cut to access the pacemaker, replacing the battery or the whole unit if needed.
- The procedure is done in an electrophysiology lab or a catheterization laboratory.
- It usually takes 1-2 hours, depending on the case.
- Your healthcare team will watch your vital signs during the procedure.
Recovery and Follow-up Care
After the surgery, you’ll be in a recovery area where your team will watch for any issues. You might go home the same day or the next, based on your health and the procedure. It’s important to follow your doctor’s advice on aftercare, including wound care and activity levels.
Your doctor will schedule check-ups to make sure the pacemaker is working right. Regular visits are key to keeping your heart healthy and catching any problems early.
How Often Do Pacemakers Need to Be Completely Replaced?
It’s important for patients and doctors to know how often pacemakers need to be replaced. This is key for managing heart health in those with these devices.
Pacemakers are advanced medical tools that need to be replaced over time. This is due to battery wear or new technology. The exact timing depends on the pacemaker type, battery life, and the patient’s needs.
Battery Replacement vs. Full Device Replacement
It’s important to know the difference between replacing a pacemaker battery and replacing the whole device. Replacing the battery is usually done through surgery. But, replacing the whole pacemaker is needed for major updates or changes in the patient’s health.
Most pacemaker batteries last between 5 to 15 years before needing a replacement. A full device replacement is usually for new technology or a change in the patient’s health.
|
Replacement Type |
Typical Interval |
Reasons for Replacement |
|---|---|---|
|
Battery Replacement |
5-15 years |
Battery depletion |
|
Full Device Replacement |
Varies |
Technological advancements, change in patient condition |
Technological Advancements Extending Replacement Intervals
New pacemaker technology has changed how often they need to be replaced. Modern pacemakers last longer and work better.
For example, rate-responsive pacemakers adjust to how active the patient is. This can mean fewer replacements. Also, cardiac resynchronization therapy (CRT) has improved heart failure management, making pacemakers last longer.
As technology keeps getting better, pacemakers will likely need to be replaced even less often. This is great news for ep cardiology and helps patients live better lives.
The Average Number of Pacemakers in a Lifetime
The number of pacemaker replacements varies among people. This is due to several factors, including age at first implant. It’s important to look at the average number of pacemakers and how age affects replacements.
Statistical Data on Pacemaker Replacements
Studies show that the number of pacemaker replacements changes with age at first implant. Younger patients might need more replacements because their pacemakers last longer compared to their age.
Statistical insights reveal that those who get a pacemaker young tend to have more replacements. On the other hand, those who get one later in life might need fewer.
Age at First Implantation and Its Impact
The age at first pacemaker implant greatly affects the total number of pacemakers in a person’s life. Younger patients often need more replacements because they live longer.
Understanding these factors helps healthcare providers manage patient expectations and treatment plans better.
Medical Considerations for Multiple Pacemaker Replacements
When you need more than one pacemaker replacement, it’s a big deal. Doctors have to think a lot about it. Pacemaker tech keeps getting better, so people live longer with them. Sometimes, they need new ones many times.
Replacing a pacemaker is usually safe. But, having to do it over and over again comes with risks. We’ll look at these risks and how doctors decide if a replacement is needed.
Risks Associated with Repeated Procedures
While pacemaker replacements are mostly safe, they’re not without risks. These include:
- Infection at the site of the pacemaker
- Bleeding or hematoma formation
- Damage to the surrounding tissue or blood vessels
- Reaction to the anesthesia used during the procedure
- Potential for lead damage or malfunction
Healthcare providers must carefully consider these risks against the benefits of replacing the pacemaker. This is very important for people who have had many replacements before.
How Doctors Determine When Replacement is Necessary
Doctors use a lot of information to decide if a pacemaker needs to be replaced. They look at:
- The battery status of the current pacemaker
- The patient’s overall health and any changes in cardiac condition
- The presence of any symptoms indicating pacemaker malfunction
- Advancements in pacemaker technology that may offer improved outcomes
An electrophysiology test might be done to check how well the pacemaker is working. This test helps doctors decide if a replacement is needed.
By looking at all these factors, doctors can figure out the best time for a pacemaker replacement. This helps patients who need multiple replacements get the best care possible.
The Role of Cardiac Electrophysiology in Pacemaker Management
Cardiac electrophysiology is key in diagnosing and treating heart rhythm problems, like pacemaker management. It helps us guide pacemaker therapy for better heart function in our patients.
What is Cardiac Electrophysiology?
Cardiac electrophysiology studies the heart’s electrical properties. It helps diagnose and treat heart rhythm disorders, or arrhythmias. Electrophysiology studies (EP studies) are vital for understanding the heart’s electrical activity and finding treatment areas.
In an EP study, we use catheters through a leg vein to reach the heart. These tools record the heart’s electrical signals. This helps us diagnose arrhythmias and plan the best treatment.
How EP Studies Guide Pacemaker Therapy
EP studies are essential in pacemaker therapy. They help us understand the heart’s electrical activity. This lets us choose the right pacemaker and settings for each patient.
For example, EP studies can show who needs cardiac resynchronization therapy (CRT). CRT helps the left and right ventricles work together better. This improves heart function in heart failure patients.
|
EP Study Findings |
Pacemaker Therapy Implications |
|---|---|
|
Abnormal electrical activity in the heart |
Need for pacemaker implantation or adjustment |
|
Identification of arrhythmia type |
Selection of appropriate pacing mode |
|
Assessment of heart’s response to pacing |
Optimization of pacemaker settings |
The EP Lab and Pacemaker Monitoring
The EP lab is where we do EP studies and pacemaker procedures. It has advanced technology for real-time heart monitoring. This lets us make precise pacemaker adjustments.
Regular monitoring in the EP lab is critical. It helps ensure the pacemaker works well. We can adjust settings as needed to keep the heart rhythm right.
By using EP study insights and advanced pacemaker tech, we offer personalized care. This approach is vital for effective pacemaker management and better patient outcomes.
Technological Innovations in Pacemaker Battery Technology
The field of pacemaker technology is changing fast. New innovations aim to make batteries last longer and devices work better. This means patients with pacemakers can go longer without needing a new battery, improving their life quality.
Recent Advancements in Battery Longevity
New battery technologies have made a big difference in pacemakers. For example, high-energy density batteries let pacemakers run for longer without needing a new battery. Also, better power management systems use less energy, making batteries last even longer.
The use of Li-ion batteries has been a game-changer. They pack more energy than old batteries, cutting down on the need for replacements. Research into solid-state batteries could bring even more improvements in the future.
|
Battery Technology |
Average Lifespan |
Key Features |
|---|---|---|
|
Traditional Pacemaker Batteries |
5-7 years |
Reliable, established technology |
|
High-Energy Density Batteries |
8-10 years |
Longer lifespan, improved efficiency |
|
Li-ion Batteries |
10+ years |
Higher energy density, potentially longer lifespan |
Future Developments on the Horizon
The future of pacemaker batteries looks bright. Researchers are working on wireless charging to make battery replacements a thing of the past. They’re also exploring energy harvesting to power pacemakers with the body’s energy, making them last forever.
Another exciting area is biocompatible batteries. These are designed to work better with the body, reducing risks. These advancements will make pacemakers more reliable and last longer for patients.
As we keep improving pacemaker technology, we’re also looking into artificial intelligence and machine learning. These technologies will help make devices work better and improve patient care. It shows our dedication to helping those who rely on pacemakers.
Pacemaker Battery Replacement Cost and Coverage
Pacemaker battery replacement costs vary a lot in the United States. This is because of different factors like the pacemaker type, procedure complexity, and provider fees. It’s important for patients to know these costs and the financial help available.
Average Costs in the United States
In the U.S., the average cost for replacing a pacemaker battery is between $40,000 and over $100,000. This price includes the device, the procedure, and any follow-up care.
- Device costs: The pacemaker generator and leads.
- Procedure costs: Surgeon fees, hospital charges, and anesthesia.
- Follow-up care: Post-procedure monitoring and check-ups.
Insurance Coverage and Financial Assistance Options
Most health insurance plans, including Medicare and Medicaid, cover pacemaker battery replacements. But, the details of coverage can differ a lot between providers and policies.
Insurance Coverage: Patients should check their insurance coverage. This includes deductibles, copays, and any out-of-pocket costs for the procedure.
Financial Assistance Programs: For those without enough insurance, there are financial help programs. These might come from pacemaker manufacturers, non-profit groups, or government programs.
It can be hard to figure out these options. So, it’s key for patients to talk about their financial worries with their healthcare provider. The provider can help find the right resources and support.
Living with a Pacemaker: Lifestyle Considerations
A pacemaker can greatly improve heart health. But, it also means making some lifestyle changes. Knowing these changes is key to keeping your device working well and staying healthy.
Activities That May Affect Pacemaker Function
Some activities and things around us can affect a pacemaker. For example, strong magnetic fields can mess with its work. This includes MRI machines, certain welding tools, and some home appliances.
It’s wise to avoid sports that could hurt your chest, where the pacemaker is. Also, be careful at security checks, as some devices can affect your pacemaker.
Precautions to Take:
- Tell your doctor about any surgeries or medical tests coming up.
- Always carry a pacemaker ID card to let doctors know.
- Don’t lean or stretch in ways that could press on the pacemaker site.
How to Maximize Your Pacemaker’s Lifespan
To make your pacemaker last longer, follow some important steps. Regular check-ups with your cardiologist are key. They help keep an eye on your device and make any needed changes.
Living a healthy lifestyle, like eating right and exercising, helps your heart and can make your pacemaker last longer.
“The key to living a long and healthy life with a pacemaker is not just about the device itself, but also about adopting a heart-healthy lifestyle.”Cardiologist
Keeping your pacemaker’s software current is also vital. Some can be updated remotely, while others need a visit to the clinic.
|
Lifestyle Adjustment |
Benefit |
|---|---|
|
Regular Exercise |
Improves overall heart health |
|
Balanced Diet |
Supports heart health and potentially extends pacemaker battery life |
|
Follow-up Appointments |
Ensures pacemaker is functioning correctly and allows for timely adjustments |
By paying attention to these points and making smart lifestyle choices, people with pacemakers can live active, healthy lives. They can also make their device last longer.
Special Considerations for Different Age Groups
Age is key in pacemaker care. From young kids to the elderly, each group has its own needs. We must tailor our care to meet these needs effectively.
Pediatric Considerations
Pediatric patients face special challenges. Their devices need to grow with them. We plan for future replacements, making sure each device lasts as long as possible.
“The implantation of a pacemaker in a child is not just a matter of correcting a heart rhythm; it’s about ensuring that the device can grow with the child and adapt to their changing needs over time.”
A study on kids with pacemakers showed the importance of cardiac electrophysiology. It’s vital to monitor and act quickly to keep the device working well.
|
Age Group |
Considerations |
Management Strategies |
|---|---|---|
|
Pediatric |
Growth, multiple replacements |
Device selection for longevity, growth accommodation |
|
Elderly |
Comorbidities, device tolerance |
Careful risk assessment, minimizing procedural complications |
Elderly Patients and Replacement Decisions
Elderly patients often have other health issues. When deciding on pacemaker replacement, we consider their health, life expectancy, and the procedure’s risks. It’s important to make decisions that improve their quality of life.
We also think about how other health problems affect the pacemaker and the patient’s ability to handle it. Regular checks and adjustments are essential for good management.
In conclusion, managing pacemakers for different age groups requires a deep understanding of their unique challenges. By tailoring our care to each group’s needs, we can improve their lives and outcomes.
Psychological Impact of Multiple Pacemaker Procedures
Having to go through multiple pacemaker procedures can be tough. It affects patients not just physically but also emotionally. The stress of repeated surgeries and managing a pacemaker can be overwhelming.
Coping with the Need for Repeated Surgeries
Dealing with the need for more pacemaker surgeries requires a broad approach. Understanding why you need more surgeries and finding ways to handle stress and anxiety is key. Open communication with healthcare providers is vital to address concerns and fears.
Patients can use mindfulness, meditation, or join support groups to cope. Building a strong support network of family, friends, and healthcare professionals is also helpful. It offers emotional support and practical help.
Support Resources for Pacemaker Patients
There are many support options for pacemaker patients. Support groups, both online and in-person, let patients share and learn from others. Electrophysiology support teams in healthcare facilities offer specialized care and guidance.
Advances in cardiac electrophysiology have improved pacemaker therapy. This has led to better patient outcomes and a higher quality of life. Patients can find educational materials and counseling services to cope with their condition.
By using these resources and effective coping strategies, patients can handle the challenges of multiple pacemaker procedures. This improves their overall well-being.
Best Practices for Pacemaker Battery Replacement
Replacing a pacemaker battery is a detailed process. It requires careful steps for the best results. Understanding preparation, the role of healthcare providers, and recovery is key.
Preparing for Scheduled Replacements
Getting ready for a pacemaker battery replacement is very important. Patients should follow their cardiologist’s instructions carefully. This may include adjusting medications, avoiding certain foods or drinks, and arranging for a ride home.
Asa renowned cardiologist, notes, “Preparation is key to minimizing risks and ensuring a smooth recovery.”
Questions to Ask Your Cardiologist
It’s important for patients to ask the right questions during their consultation. Some key questions include:
- What are the specific risks associated with my pacemaker battery replacement?
- How will the procedure be performed, and what type of anesthesia will be used?
- What are the expected outcomes, and how will my pacemaker be monitored post-replacement?
Being proactive and informed can significantly enhance the overall experience.
Recovery Tips from Medical Professionals
Recovery from pacemaker battery replacement needs careful attention. Medical professionals recommend:
- Resting for the remainder of the day after the procedure
- Avoiding heavy lifting or strenuous activities for a specified period
- Monitoring the incision site for signs of infection
As one patient shared, “Following the recovery tips provided by my healthcare team made a significant difference in my healing process.”
By following these best practices, patients can have a successful pacemaker battery replacement. It shows how electrophysiology cardiology has advanced, making these procedures routine and effective.
“The advancements in pacemaker technology and replacement procedures have greatly improved patient outcomes. It’s a remarkable field that continues to evolve.”
Conclusion: Living a Full Life with Multiple Pacemakers
Thanks to new pacemaker tech, people with pacemakers can live better lives. We’ve looked at what pacemakers do, how long they last, and how to replace their batteries. With the right care, people can stay active and enjoy life with multiple pacemakers.
Knowing how long pacemakers last and how they work is key. It helps people get the most out of their devices. By staying informed and working with doctors, patients can make good choices and live well.
Having multiple pacemakers means regular check-ups are important. But it shouldn’t stop you from doing things you love. With the right support, you can keep living fully, spending time with family and friends, and following your dreams.
FAQ
What is a pacemaker and how does it work?
A pacemaker is a small device implanted in the body. It helps control the heartbeat by sending electrical impulses. This makes the heart muscle contract. It treats abnormal heart rhythms and helps restore a normal rhythm.
How long do pacemaker batteries typically last?
A pacemaker battery’s lifespan varies. It depends on the pacemaker type, the patient’s condition, and device settings. On average, it lasts 5 to 15 years.
What are the signs that a pacemaker battery needs replacement?
Signs of a dying pacemaker battery include fatigue, dizziness, and shortness of breath. Swelling in the legs and feet is also a sign. Many patients don’t notice symptoms until the battery is almost gone. Regular check-ups with a cardiologist are important.
How is a pacemaker battery replaced?
Replacing a pacemaker battery is a minor surgery. A small incision is made to access the pacemaker. The old battery is swapped for a new one, and the device is reprogrammed.
Can you have multiple pacemakers in a lifetime?
Yes, it’s possible to have multiple pacemakers. The need for a new one depends on the pacemaker type, the patient’s condition, and technology advancements.
What is cardiac electrophysiology, and how does it relate to pacemakers?
Cardiac electrophysiology studies the heart’s electrical properties. It’s key in pacemaker management. EP studies help diagnose and treat heart rhythm problems and guide pacemaker therapy.
How do technological advancements impact pacemaker longevity?
Technological advancements have improved pacemaker battery life and performance. These advancements help extend pacemaker lifespan and reduce replacement needs.
What are the costs associated with pacemaker battery replacement?
The cost of replacing a pacemaker battery varies. It depends on the pacemaker type, location, and healthcare provider. In the U.S., costs range from $20,000 to $50,000 or more.
Are there any lifestyle changes that can help maximize pacemaker lifespan?
While lifestyle changes can’t directly affect pacemaker lifespan, a healthy lifestyle is beneficial. Eating well, exercising regularly, and managing stress can improve overall heart health.
What are the psychological impacts of multiple pacemaker procedures?
Multiple pacemaker procedures can affect patients psychologically. They may feel anxious, stressed, and uncertain. But, with support and care, many patients cope well with repeated surgeries.
What are the best practices for pacemaker battery replacement?
Best practices include preparing for replacements, asking questions, and following recovery tips. This ensures a smooth process.
How often do pacemakers need to be completely replaced?
Pacemaker replacement frequency varies. It depends on the pacemaker type, patient condition, and technology advancements. While battery replacement is needed every 5-15 years, full device replacement is less frequent.
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1769065/










