
Nearly 200,000 Americans get a pacemaker implant each year. This shows how important these devices are for heart health. Pacemaker en ICD implant pain? It’s minimal. Get best painless facts. Numbing meds ensure a safe and amazing experience. Don’t fear this.
Thinking about getting a cardiac device can be scary. People worry about the pain and what the experience will be like.
Pacemakers and ICDs are used to fix heart rhythm problems. They are put under the skin but do different things. Pacemakers keep the heart beating right. ICDs stop sudden death by shocking the heart when needed.
Key Takeaways
- Pacemaker and ICD implantations are common for heart rhythm issues.
- The process involves putting a device under the skin.
- These devices help keep the heart rhythm steady and prevent dangerous arrhythmias.
- Knowing about the procedure and devices can ease worries about pain and the experience.
- Medical technology has made these procedures safer and more effective.
Understanding Cardiac Devices: Pacemakers and ICDs
Pacemakers and ICDs are advanced medical tools. They help manage irregular heartbeats and prevent sudden death. These devices have greatly improved heart health, giving patients a better life and longer life expectancy.
What is a Pacemaker?

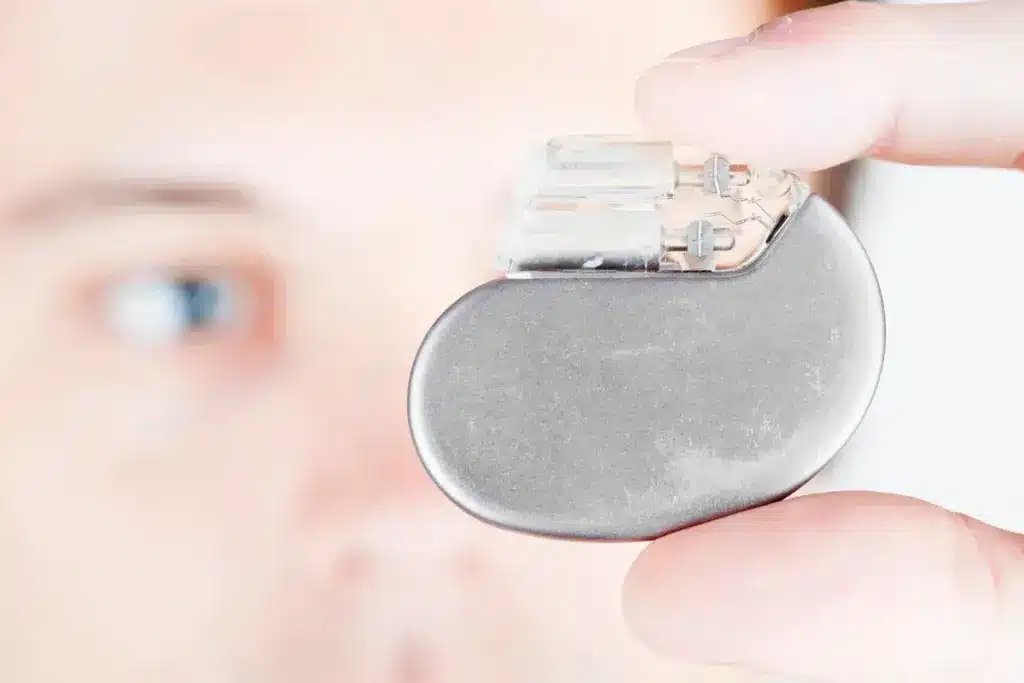
A pacemaker is a small device implanted to control the heartbeat. It sends electrical impulses to keep the heart rate steady. This is mainly for treating bradycardia, when the heart beats too slow. It helps the heart work better overall.
What is an Implantable Cardioverter-Defibrillator (ICD)?
An ICD is a more advanced device. It watches the heart’s rhythm and shocks it when needed. This is to stop dangerous heart rhythms that could be fatal. It’s key in preventing sudden cardiac death.
How These Devices Work
Pacemakers and ICDs use electrical impulses to manage heart rhythm. Here’s how they operate:
- They are implanted under the skin, usually in the chest.
- Leads (thin, insulated wires) are guided through a vein into the heart.
- The devices always check the heart’s rhythm.
- They send electrical impulses or shocks when needed to fix abnormal rhythms.
The main difference is their use. Pacemakers treat slow heart rhythms. ICDs prevent sudden death from dangerous arrhythmias.
It’s important for patients to understand these devices before getting them. Knowing how pacemakers and ICDs work helps them see the benefits and risks. This knowledge is key to making informed decisions about these life-saving technologies.
Medical Conditions Requiring Pacemaker or ICD Implantation
Heart conditions like arrhythmias and heart failure often need pacemakers or ICDs. These devices help manage symptoms and improve life quality. They are key in treating irregular heartbeats and preventing sudden cardiac death.
Arrhythmias and Bradycardia
Arrhythmias are irregular heartbeats that can be too fast, too slow, or irregular. Bradycardia, where the heart beats too slowly, often leads to pacemaker implantation. We’ll look at how these conditions are diagnosed and treated with cardiac devices.
- Symptoms of bradycardia include dizziness, fatigue, and shortness of breath.
- Diagnosis involves electrocardiogram (ECG) tests and sometimes a Holter monitor.
- Treatment with a pacemaker can help regulate the heartbeat.
Heart Block
Heart block is when electrical signals between heart chambers are delayed or blocked. This can make the heart beat too slowly. We’ll explore the different types of heart block and their treatments.
- First-degree heart block is usually without symptoms and might not need treatment.
- Second-degree heart block can cause dizziness and might need a pacemaker.
- Third-degree heart block is serious and often requires a pacemaker.
Heart Failure
Heart failure happens when the heart can’t pump enough blood. In some cases, a cardiac device like an ICD or CRT (Cardiac Resynchronization Therapy) device is recommended. We’ll discuss how these devices help manage heart failure.
Understanding these conditions and their treatments helps patients make better care choices. It improves their heart health.
Types of Pacemaker and ICD Systems
Cardiac technology has grown a lot, leading to many pacemaker and ICD systems. These systems help patients with different heart problems. They improve life quality for many people.
Single-Chamber vs. Dual-Chamber Pacemakers
Pacemakers come in single-chamber and dual-chamber types. Single-chamber pacemakers have one lead in the heart. They help with some arrhythmias. Dual-chamber pacemakers have two leads, one in each chamber. They pace the heart better.
Choosing between single-chamber and dual-chamber pacemakers depends on the patient’s condition. Dual-chamber pacemakers are better for heart block or pacing in both chambers.
Subcutaneous vs. Transvenous ICDs
ICDs can be put in with subcutaneous or transvenous methods. Transvenous ICDs go through a vein into the heart. Subcutaneous ICDs are under the skin, without leads in the heart or veins.
Subcutaneous ICDs are good for those at risk of lead problems or don’t need pacing. They lower the risk of some complications.
Leadless Pacemakers
Leadless pacemakers are a big step forward. They go straight into the heart with a catheter, no leads needed. They’re great for those at risk of lead issues or with limited access.
The creation of leadless pacemakers has given new options for pacing therapy. They offer a less invasive choice than traditional pacemakers.
The Pacemaker and ICD Implantation Procedure Explained
Understanding the procedure for pacemaker or ICD implantation can alleviate patient anxiety. We aim to make this process clear and comforting for you.
Pre-Procedure Preparation
Preparation is key before the procedure starts. Local anesthesia is given to reduce pain. Antibiotics are also given to lower infection risk. We make sure you’re comfortable and all equipment is ready.
The area for the implant is cleaned and prepared. This is important to avoid complications. Our team makes sure everything is set for a smooth procedure.
Step-by-Step Implantation Process
The implantation process has several steps. A small incision is made for the device. Leads are guided through a vein to the heart and secured. The device is then connected and programmed for the patient’s needs.
After the device is in place, it’s tested. This checks if it can pace the heart or deliver a shock. Our team watches the heart rhythm to make sure it works right.
Duration of the Procedure
The procedure’s length varies based on the device and patient health. It can take from one to several hours. Our team keeps you informed at every step.
Understanding the pacemaker and ICD implantation steps helps patients prepare. We’re dedicated to giving you the best care, ensuring great outcomes.
Anesthesia Used During Pacemaker Implantation
Anesthesia is key to making pacemaker implantation pain-free. It reduces discomfort and anxiety. This makes the procedure smoother for patients.
Local vs. General Anesthesia
Local anesthesia is often used for pacemaker implantation. It numbs the chest area where the device is placed. General anesthesia, which makes you unconscious, is less common but used in some cases.
Local anesthesia is preferred because it keeps patients awake and responsive. This reduces risks from general anesthesia. But, the choice depends on the patient’s health and the procedure’s complexity.
Conscious Sedation Options
Conscious sedation is also used to relax patients during the procedure. It uses medications to make you calm without making you unconscious.
Medications like midazolam or fentanyl are common for conscious sedation. They help patients feel more at ease during the implantation.
How Anesthesia Affects Pain Perception
The type of anesthesia used greatly affects pain perception. Local anesthesia numbs the area, reducing pain. Conscious sedation also helps by reducing anxiety and promoting relaxation.
It’s important to understand how anesthesia impacts pain perception. This helps manage patient expectations and ensures a successful procedure. Local anesthesia and conscious sedation are often the best combination for pacemaker implantation.
|
Type of Anesthesia |
Description |
Benefits |
|---|---|---|
|
Local Anesthesia |
Numbness in the surgical area |
Minimizes pain, allows patient to remain awake |
|
General Anesthesia |
Induces unconsciousness |
Used in complex cases or when necessary |
|
Conscious Sedation |
Relaxation and reduced anxiety |
Enhances patient comfort, reduces stress |
Pain Levels During Pacemaker Implantation
Pacemaker implantation is a common treatment for heart conditions. Many wonder about the pain involved. We’re here to clear up what you can expect during the procedure.
What Patients Feel During the Procedure
Patients usually get local anesthesia or conscious sedation during the procedure. This makes the pain much less. Most patients say they feel only a little pain, like a pinch or pressure when the device is put in.
Thanks to advanced technology and techniques, the procedure is more comfortable. For example, leadless pacemakers make the implantation simpler, which might reduce discomfort.
Common Sensations and Discomfort
Even though the procedure is generally okay, some patients might feel certain sensations or discomfort. Common feelings include:
- A feeling of pressure or mild discomfort at the implant site
- Slight pain when the local anesthetic is administered
- Awareness of the device being implanted, though this is not typically painful
These feelings are usually short-lived and can be managed well with the right pain management.
Factors Affecting Pain Experience
Several things can change how much pain or discomfort a patient feels during pacemaker implantation. These include:
|
Factor |
Impact on Pain Experience |
|---|---|
|
Anxiety Levels |
Higher anxiety can increase perceived pain |
|
Practitioner’s Skill |
A more skilled practitioner can minimize discomfort |
|
Individual Pain Tolerance |
Patients with lower pain tolerance may experience more discomfort |
Knowing these factors can help manage expectations and make the experience better for patients getting a pacemaker implant.
Post-Procedure Pain: What to Expect
After getting a pacemaker, many wonder about the recovery and pain. The time after the procedure can be a bit uncomfortable. But knowing what to expect can ease your worries. We’ll walk you through the usual pain during the first few days and when it should go away.
Immediate Recovery Period
Right after the procedure, you might feel some pain at the implant site. Your doctor will give you pain medicine to help with this.
First Few Days After Implant
In the days after, you might notice soreness or bruising where the pacemaker was put in. This is usually mild and gets better with time.
When Pain Should Subside
Most people find their pain or discomfort goes down a lot within a week. But, how fast you recover can depend on your health and the details of your procedure.
|
Recovery Aspect |
Immediate Recovery |
First Few Days |
Expected Timeline for Improvement |
|---|---|---|---|
|
Pain/Discomfort Level |
Moderate |
Mild to Moderate |
Within 1 week |
|
Activity Level |
Limited |
Gradually increasing |
Full recovery in 4-6 weeks |
|
Pain Management |
Prescribed medication |
Over-the-counter pain relievers |
As directed by healthcare provider |
Pain Management After Pacemaker Implantation
Managing pain well after a pacemaker implant is key for a smooth recovery. We know patients worry about pain after this procedure.
Prescribed Medications
Your doctor might give you medicines to help with pain and discomfort after the procedure. These could be:
- Analgesics to ease pain
- Anti-inflammatory drugs to lessen swelling
It’s important to take the medicines as directed and tell your doctor about any side effects.
Over-the-Counter Pain Relief Options
There are also OTC pain relief options that can help with post-implantation pain. Some common ones are:
|
Medication |
Dosage |
Purpose |
|---|---|---|
|
Acetaminophen |
As directed |
Pain relief |
|
Ibuprofen |
As directed |
Pain relief and anti-inflammatory |
Always check with your doctor before using OTC medicines, if you have any health issues.
Non-Pharmaceutical Pain Management Techniques
There are also non-medical ways to manage pain and discomfort after a pacemaker implant:
- Rest and relaxation to help with healing
- Applying ice to reduce swelling
- Maintaining a healthy diet to aid in recovery
Comparing Pacemaker and ICD: Differences in Implantation and Pain
Pacemakers and ICDs are both used to help the heart. But they are implanted differently and can feel different to the patient. Knowing these differences helps patients understand what to expect with pain and recovery.
Size and Placement Differences
Pacemakers and ICDs are not the same size or placed in the same way. ICDs are bigger because they need extra parts for defibrillation.
Here’s a table showing the main size and placement differences:
|
Device |
Size |
Typical Placement |
|---|---|---|
|
Pacemaker |
Smaller, about the size of a matchbox |
Under the skin, below the collarbone |
|
ICD |
Larger, due to additional components |
Similar to pacemakers, under the skin |
Recovery Comparison
Recovering from both devices is similar, as it involves a minor surgery. But ICDs might take longer to recover from because they are bigger. This can make the recovery more uncomfortable for some.
Here are some key recovery points:
- Hospital stay: Usually just one night
- Activity restrictions: Both devices have similar rules, like no heavy lifting
- Pain management: Both use similar methods to manage pain at the site
Patient-Reported Pain Differences
People feel pain differently, but studies show little difference in pain between pacemaker and ICD users. Both usually feel mild to moderate pain during recovery.
Here’s a table comparing pain levels reported by patients:
|
Device |
Immediate Post-Procedure Pain |
Pain at Follow-Up |
|---|---|---|
|
Pacemaker |
Mild to moderate |
Minimal |
|
ICD |
Mild to moderate, potentially more discomfort |
Minimal, similar to pacemaker recipients |
Every person’s pain experience is different. Things like how much pain you can handle and the details of your surgery can affect how you feel.
Common Misconceptions About Pacemaker Implantation Pain
Many people think pacemaker implantation is very painful. This can make them anxious, which can change how they feel pain during and after the procedure.
Myth vs. Reality
One big myth is that pacemaker implantation is very painful. But, most patients say it only feels a little uncomfortable. This is because of the local anesthesia and conscious sedation used.
Another myth is that the procedure takes a long time. While it can take a few hours, the actual part where the pacemaker is put in only takes about 30 minutes to an hour.
|
Myth |
Reality |
|---|---|
|
Pacemaker implantation is very painful. |
Most patients experience mild discomfort. |
|
The procedure is lengthy and complicated. |
The actual implantation takes about 30 minutes to an hour. |
How Anxiety Affects Pain Perception
Anxiety can make people feel pain more. It’s important to talk about fears and anxieties with the doctor before the procedure.
Anxiety Management Techniques include deep breathing, meditation, and cognitive-behavioral therapy. These can help lower anxiety and make the experience less stressful.
Managing Pre-Procedure Fears
Knowing what to expect can help reduce fears before the procedure. Patients should ask questions and clear up any doubts they have.
Pre-procedure preparation is important. It’s not just about physical prep but also getting mentally ready. Patients who are well-prepared tend to have a better experience.
By tackling misconceptions and managing anxiety, patients can have a better experience with pacemaker implantation. It’s important for doctors to offer support and clear information to help reduce fears and misconceptions.
Potential Complications That May Cause Pain
Pacemaker and ICD implants are usually safe. But, some complications can cause pain. Knowing these issues helps manage recovery better.
Infection at the Implant Site
Infection is a serious issue after these implants. Look out for redness, swelling, warmth, or drainage. Also, watch for fever or chills.
“Prompt medical attention is key if you see these signs,” as infections can get worse fast.
Lead Displacement
Lead displacement means the leads move from their place. This can lead to pain and might need more surgery. You might feel unusual sensations or movements under your skin.
Pocket Hematoma
A pocket hematoma is blood around the device. It can cause swelling, pain, and bruising. Most times, it goes away by itself. But big ones might need draining to ease pain and prevent more problems.
Device Erosion
Device erosion happens when the device sticks out through the skin. It’s often due to bad tissue coverage. This can cause pain, infection, and might need surgery to fix.
Knowing about these complications helps patients watch their condition closely. It’s important for managing pain and ensuring a good recovery after these implants.
Real Patient Experiences with Pacemaker and ICD Implantation
Patients with pacemakers and ICDs share a variety of feelings and results after getting them. Their stories offer comfort and insights to those thinking about or have had these procedures.
Testimonials About Pain Levels
People report different levels of pain during and after the procedure. Some say it feels like a mild discomfort during. Others mention feeling more pain, mainly during recovery.
“I was surprised by how little pain I experienced during the procedure. The doctors and nurses were very reassuring, and I felt comfortable throughout.” –
Pacemaker Recipient
The pain level can depend on many things. This includes the device type, the person’s pain tolerance, and the anesthesia’s success.
Coping Strategies from Patients
Patients have found ways to deal with discomfort and adjust to life with a pacemaker or ICD. They include:
- Following the doctor’s instructions for post-procedure care
- Using prescribed pain medication effectively
- Engaging in relaxation techniques such as deep breathing or meditation
- Maintaining a healthy lifestyle to support overall heart health
Sharing these strategies helps new patients smoothly navigate their recovery.
Unexpected Sensations Reported
Some patients have felt unexpected sensations after getting a pacemaker or ICD. These can include:
- Feeling the device under the skin
- Noticing changes in heart rhythm or palpitations
- Experiencing muscle twitches or contractions
These sensations can be surprising, but they usually lessen as the patient gets used to the device.
Knowing what patients have gone through with pacemaker and ICD implantation can ease worries. It prepares people for what to expect. By sharing stories and strategies, we build a supportive community. This helps patients on their journey with these devices.
Recovery Timeline After Cardiac Device Implantation
Knowing the recovery timeline after getting a cardiac device is key. It helps patients know what to expect and how to care for themselves. The recovery time can vary, but there are general steps most people follow.
First Week Post-Procedure
The first week is very important for recovery. Doctors usually tell patients to rest and not do too much. You might feel some pain or discomfort where the device was put in. This can be helped with medicine.
It’s important to follow your doctor’s advice on wound care and what activities to do. Most people can start doing normal things again in a few days. But, it’s best to avoid heavy lifting and hard exercise.
First Month of Recovery
In the first month, you’ll likely start to feel better. The pain at the implant site should get less. Make sure to go to all your follow-up doctor visits. This is to check that the device is working right and to talk about any problems.
By 2-4 weeks, you can usually go back to your usual activities. But, it’s good to avoid heavy lifting, bending, or hard exercise for a bit longer. Your doctor will tell you how long.
|
Activity |
Recommended Timeline |
Notes |
|---|---|---|
|
Light housework |
1-2 weeks |
Avoid heavy lifting |
|
Driving |
3-7 days |
Check with doctor first |
|
Strenuous exercise |
4-6 weeks |
Gradually increase intensity |
Long-Term Adjustment Period
After you get past the initial recovery, you enter a long-term adjustment phase. This is when you get used to having the device and any lifestyle or activity changes.
“I’ve had my pacemaker for over a year now, and it’s been a game-changer. I’ve learned to live with it, and it’s become a part of me.” –
Most people get used to their device in a few months. It’s important to keep in touch with your healthcare team. This is to check how the device is doing and to deal with any problems.
By understanding the recovery timeline and following your doctor’s advice, you can have a smooth recovery after getting a cardiac device.
Living with a Pacemaker or ICD: Long-Term Comfort Considerations
After getting a pacemaker or ICD, you’ll need to make some changes. The first few weeks are key, but getting used to it long-term is just as important. This helps you adjust smoothly to life with your device.
Adapting to the Device’s Presence
Getting used to a pacemaker or ICD takes time. At first, you might feel it, but you’ll get used to it. It’s important to follow your doctor’s advice and go to check-ups. This ensures your device works right and helps with any worries.
Tips for Adapting:
- Be mindful of the device’s location and avoid direct pressure on it.
- Gradually increase physical activities as advised by your healthcare provider.
- Monitor for any unusual sensations or signs of complications.
Physical Activities and Comfort
Staying active is key to staying healthy, even with a pacemaker or ICD. But, you might need to change some activities for comfort and safety.
|
Activity |
Precautions |
Comfort Tips |
|---|---|---|
|
Exercise |
Avoid contact sports that could damage the device. |
Start with low-impact exercises and gradually increase intensity. |
|
Lifting |
Avoid heavy lifting, specially on the side of the device. |
Use proper lifting techniques to avoid straining your back. |
|
Traveling |
Inform security personnel about your device to avoid issues with security scanners. |
Carry your device identification card with you. |
Sleeping Positions and Daily Comfort
At first, sleeping on the side of the device might be uncomfortable. But, it usually gets better over time. Try different sleeping positions to find what works best for you.
What you wear can also affect your comfort. Wearing loose clothes can help avoid irritation at the implant site.
In conclusion, living with a pacemaker or ICD means making some changes. But, with the right advice and attitude, you can live an active and comfortable life. Always follow your doctor’s advice and stay aware of your device for long-term comfort and health.
When to Contact Your Doctor About Pain
After getting a pacemaker or ICD, it’s key to know when pain is normal and when it’s not. We’ll help you understand pain patterns. This way, you can listen to your body’s signals.
Normal vs. Abnormal Pain Patterns
Some discomfort is okay after the procedure. But, it’s important to tell normal soreness from pain that might mean a problem. Normal pain is usually mild and gets better with time and medicine.
Abnormal pain is different. It’s severe, gets worse, or comes with other bad signs. If your pain doesn’t get better or gets worse, call your doctor.
|
Pain Characteristics |
Normal |
Abnormal |
|---|---|---|
|
Severity |
Mild to moderate |
Severe |
|
Duration |
Improves over a few days |
Persists or worsens |
|
Associated Symptoms |
Minimal |
Swelling, redness, fever |
Warning Signs of Complications
Some symptoms mean you need to see a doctor fast. These include:
- Increasing pain or swelling at the implant site
- Redness or warmth around the device pocket
- Fever or chills
- Discharge or pus from the incision site
- Arm or leg swelling
Emergency Situations
Some problems are emergencies. Severe symptoms like trouble breathing, chest pain, or dizziness need quick help.
It’s hard to know if your symptoms are serious. If unsure, always talk to your doctor.
Conclusion: Balancing Concerns About Pain with Medical Necessity
Pain worries are big for people getting pacemakers or ICDs. These devices might hurt a bit at first, but they’re often really needed. This makes the pain worth it for many.
We’ve looked at pacemaker and ICD implantation in this article. We talked about the process, how much pain you might feel, and ways to handle it. Knowing what to expect helps people get ready for the implant and recovery.
Pacemakers and ICDs are key for heart health. They can save lives. We suggest talking to your doctor about pain worries. This way, you can make a plan to feel better during and after the procedure.
FAQ
What is the difference between a pacemaker and an ICD?
A pacemaker helps control your heartbeat at a normal rate. An ICD can prevent sudden death by delivering an electric shock to restore a normal heartbeat.
Is the pacemaker implantation procedure painful?
Most people feel only mild discomfort during the procedure. This is because local anesthesia and conscious sedation are used.
What type of anesthesia is used during pacemaker implantation?
Local anesthesia numbs the area where the pacemaker is implanted. Conscious sedation helps the patient relax during the procedure.
How long does the pacemaker implantation procedure take?
The procedure usually takes 1-2 hours. This depends on the case’s complexity and the pacemaker type.
What are the possible complications of pacemaker implantation?
Complications include infection, lead displacement, and pocket hematoma. It’s important to follow post-procedure instructions to minimize risks.
How long does it take to recover from pacemaker implantation?
Recovery takes a few weeks. Most people can return to normal activities within a week or two.
Can I exercise with a pacemaker or ICD?
Yes, but follow your doctor’s specific guidelines. Some activities may be restricted.
How often do I need to have my pacemaker or ICD checked?
You need regular follow-up appointments. This is usually every 3-6 months, depending on your device and condition.
Can I undergo an MRI with a pacemaker or ICD?
Some devices are MRI-compatible. Always inform your doctor or the MRI technician before a scan.
What are the signs of possible complications I should watch for?
Look out for redness, swelling, or pain at the implant site. Fever or unusual device behavior are also signs. Contact your doctor if you notice these symptoms.
How do I manage pain after pacemaker implantation?
Your doctor may prescribe medications or recommend over-the-counter options. Rest, ice, or relaxation exercises can also help manage pain.
Can I travel with a pacemaker or ICD?
Yes, but tell your doctor and the airline (if flying) about your device. Carry a device identification card with you.
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://pubmed.ncbi.nlm.nih.gov/PMC9982664/








