
Pediatric glioblastoma is a rare and aggressive brain tumor found in children and teens. At Liv Hospital, we aim to give you all the details about this condition. This includes its symptoms, types, and treatment choices.
Recent studies have looked into new treatments for glioblastoma in children. A study onNCBI found that about 0.85 per 100,000 kids get this tumor. Common signs include headaches, vomiting, and changes in how they feel.
We will dive into the main points about pediatric glioblastoma. This includes its types, how it’s treated, and the latest in research and care. Our goal is to offer hope and support to families dealing with this tough condition.
Key Takeaways
- Knowing the symptoms and types of pediatric glioblastoma is key for early detection.
- Treatment options include removing as much of the tumor as possible and using chemotherapy and radiation.
- Recent research has focused on molecular targeted therapies and immunotherapy.
- Pediatric glioblastoma is most commonly seen in the supratentorial brain.
- The highest incidence is seen between ages 15 and 19.
What Makes Pediatric Glioblastoma Unique
Glioblastoma in children is different from the adult version in many ways. While it’s the most common and aggressive brain cancer in adults, it’s much rarer in kids. It makes up a small part of brain tumors in children.
Definition and Basic Characteristics
Pediatric glioblastoma, or pediatric glioblastoma multiforme, is a high-grade glioma in kids. It grows fast and is very aggressive. Unlike slower-growing gliomas, high-grade gliomas like glioblastoma are more aggressive and have a worse outlook.
The main traits of pediatric glioblastoma are:
- High-grade malignancy
- Rapid growth and progression
- Distinct genetic profiles compared to adult glioblastoma
- Variable response to treatment
The Impact on Children and Families
Getting diagnosed with pediatric glioblastoma deeply affects kids and their families. It brings medical, emotional, and psychological challenges.
Some key impacts are:
- Emotional Distress: The diagnosis and treatment can cause a lot of emotional stress for the child and their family.
- Disruption of Normal Life: Treatment for glioblastoma can be long and demanding. It can disrupt the child’s education and normal activities.
- Financial Burden: The cost of treatment, including surgery, radiation, and chemotherapy, can be very expensive for families.
Understanding pediatric glioblastoma shows we need a full approach. We must tackle the medical, emotional, and financial challenges faced by kids and their families.

Fact 1: Incidence and Epidemiology
Pediatric glioblastoma is a rare and aggressive brain cancer. It has unique characteristics that need to be studied closely. Knowing how common it is and its patterns helps doctors find better treatments for kids with this disease.
Statistical Overview of Pediatric Brain Tumors
The rate of primary malignant brain and CNS tumors in kids is key to understanding glioblastoma. Recent data shows it affects about 5.61 per 100,000 children.
| Age Group | Incidence Rate per 100,000 |
| 0-14 years | 5.61 |
| 0-9 years | 4.8 |
| 10-14 years | 6.4 |
These numbers show how the risk changes with age in kids.
Risk Factors and Possible Causes
The exact reasons for pediatric glioblastoma are not known. But, some risk factors have been found. Genetic conditions like Li-Fraumeni syndrome and neurofibromatosis type 1 increase the risk.
Being exposed to ionizing radiation is also a risk. Kids who had radiation for other health issues are more likely to get glioblastoma later.
Knowing these risks helps doctors find ways to catch it early and maybe even prevent it in the future.
Fact 2: Recognizing the Symptoms of Pediatric Glioblastoma
Spotting the signs of pediatric glioblastoma early can really help treatment work better and improve the patient’s chances. This brain cancer in kids is tricky to diagnose because its symptoms are not unique. They can look like other common childhood issues.
Early Warning Signs in Children
The first signs of pediatric glioblastoma can be hard to notice and different for each child. Kids might have persistent headaches, nausea and vomiting, and vision changes. These happen because the tumor presses on the brain.
Some kids might also have seizures, weakness or numbness in the limbs, and changes in personality or behavior. It’s important for parents and caregivers to watch for these signs. If they don’t go away or get worse, they should see a doctor.
Age-Specific Symptom Presentation
The way pediatric glioblastoma shows up can change with age. Young kids might just seem off, tired, or not growing right. They can’t tell us how they feel as well as older kids can.
Older kids and teens are more likely to say they have headaches, see things differently, or have trouble with balance. Knowing how symptoms change with age helps doctors find and treat the cancer sooner.
By knowing the symptoms of pediatric glioblastoma and how they differ by age, doctors and families can work together. This helps get a diagnosis and start treatment faster.
Fact 3: Types of Glioblastoma in Children
Pediatric glioblastoma includes several subtypes, each with its own traits and genetic makeup. Knowing these differences is key to creating effective treatment plans.
Classic Glioblastoma Multiforme
Classic glioblastoma multiforme is the most common in kids. It has very aggressive cells and a lot of cell activity. The tumor often has dead cells, which sets it apart from less severe gliomas.
Giant Cell Glioblastoma
Giant cell glioblastoma is rare and known for its large cells. It has a different genetic makeup than classic glioblastoma. This might mean a slightly better chance of recovery because it can sometimes be removed surgically.
Epithelioid Glioblastoma
Epithelioid glioblastoma is aggressive and has a unique look. It has big cells that look like other cancers. This type grows fast and is hard to treat.
Other Rare Variants
There are also rare types of glioblastoma in kids, like gliosarcoma and small cell glioblastoma. Each rare type has its own look and genetic changes.
To understand these glioblastoma subtypes better, we’ve made a table with their main features:
| Subtype | Histological Features | Genetic Profile | Prognosis |
| Classic Glioblastoma Multiforme | Highly malignant cells, necrosis | Complex genetic alterations | Generally poor |
| Giant Cell Glioblastoma | Large, multinucleated giant cells | Different genetic profile | Slightly more favorable |
| Epithelioid Glioblastoma | Large, epithelioid cells | Aggressive genetic markers | Poor, due to rapid growth |
As the table shows, each glioblastoma subtype has its own traits that affect treatment and outlook. Knowing these differences is vital for the best care for kids with glioblastoma.
Fact 4: Diagnosis and Staging Process
We use neuroimaging, biopsy, and molecular testing to diagnose pediatric glioblastoma. This process is key to finding the right treatment and understanding the patient’s outlook.
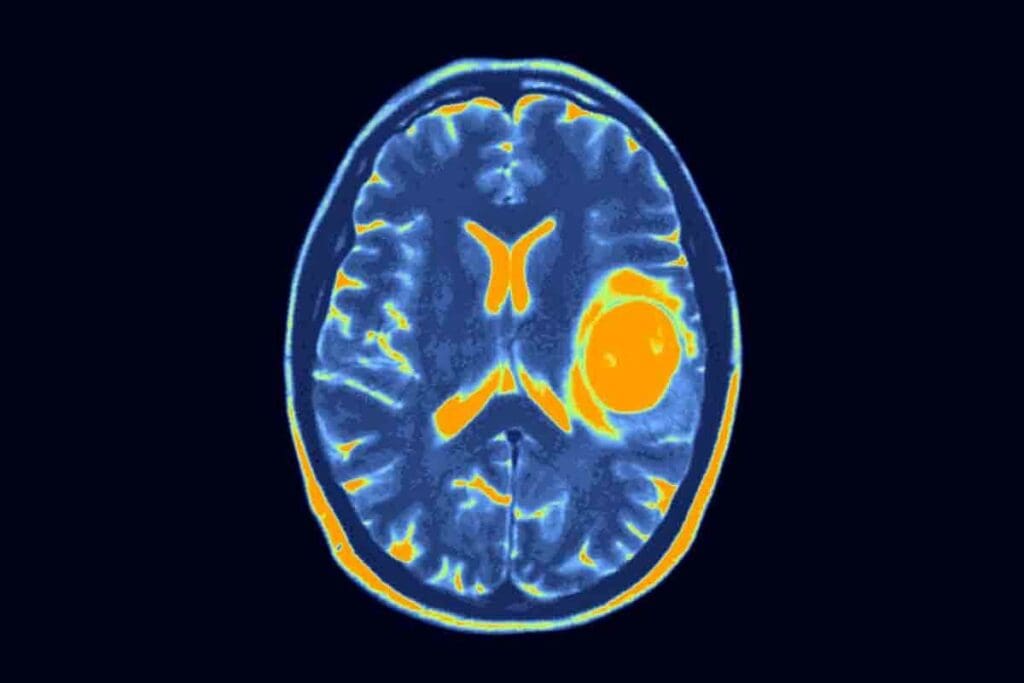
Neuroimaging Techniques
Neuroimaging is vital in diagnosing pediatric glioblastoma. We mainly use Magnetic Resonance Imaging (MRI) to see the tumor’s size and location. MRI gives us detailed images to check how the tumor affects the brain.
We also use Computed Tomography (CT) scans and Positron Emission Tomography (PET) scans to get more info. These scans help in understanding the tumor better and in staging.
Biopsy and Pathological Examination
A biopsy is key to confirming pediatric glioblastoma. A neurosurgeon takes a tumor sample, which a pathologist then examines. This examination helps determine the tumor’s grade and type.
The pathologist uses staining techniques and microscopic analysis. They look for signs like cellular atypia and mitotic activity to confirm glioblastoma.
Molecular and Genetic Testing
Molecular and genetic testing are now key in diagnosing pediatric glioblastoma. These tests find specific genetic changes that guide treatment and predict outcomes.
- IDH1/IDH2 mutations: Some glioblastomas have IDH1 or IDH2 gene mutations, which affect treatment and prognosis.
- MGMT promoter methylation: MGMT promoter methylation is a marker that shows how well certain chemotherapy works.
- Other genetic alterations: We find other genetic changes that help in planning treatment.
By combining neuroimaging, biopsy, and molecular testing, we get an accurate diagnosis and staging. This is essential for creating an effective treatment plan.
Fact 5: Genetic and Molecular Characteristics of Pediatric Glioblastoma
Pediatric glioblastoma has its own set of genetic and molecular traits. Unlike adult glioblastoma, which is often linked to specific genetic mutations, pediatric glioblastoma has a unique profile. This uniqueness requires a different approach in diagnosis and treatment.
Key Genetic Alterations
Pediatric glioblastoma is marked by several key genetic changes. A significant number of cases have mutations in the H3F3A gene. Other changes involve the TP53 and PDGFRA genes. These mutations make the disease aggressive and affect treatment plans.
A study in theNational Center for Biotechnology Information shows the importance of these genetic changes. They are key to developing targeted therapies.
- Mutations in the H3F3A gene are common in pediatric glioblastoma.
- Changes in TP53 and PDGFRA genes are also frequent.
- These genetic changes drive the disease’s progression and impact treatment choices.
How Genetic Profiles Differ from Adult Cases
The genetic profile of pediatric glioblastoma is different from adult glioblastoma. For example, adult glioblastoma often has TERT promoter mutations, but these are rare in kids. On the other hand, kids’ glioblastoma often has H3F3A mutations, which are uncommon in adults. This highlights the need for age-specific treatments.
It’s vital to understand these differences. This knowledge helps in creating effective treatments for pediatric glioblastoma’s unique genetic and molecular traits.
Fact 6: Standard Treatment Approaches
Treating pediatric glioblastoma needs a deep understanding of the best treatments. The disease’s complexity calls for a mix of therapies to get the best results.
Surgical Interventions
Surgery is key in treating pediatric glioblastoma. The main goal is to remove as much of the tumor as possible without harming the brain. New surgical methods, like intraoperative MRI, make these operations safer and more precise.
Every child’s case is different. So, the surgery plan must be made just for them. Whether to remove most of the tumor or not depends on where it is and the child’s health.
Radiation Therapy Considerations in Children
Radiation therapy is important in treating pediatric glioblastoma. But it must be used carefully in kids because of the risks to their growing brains. New radiation methods, like proton therapy, are safer for healthy tissues.
We work with radiation experts to plan treatments. We aim to control the tumor while avoiding long-term harm. The dose and how it’s given are carefully chosen for this balance.
Chemotherapy Protocols
Chemotherapy is also vital in treating pediatric glioblastoma. Temozolomide is a common chemotherapy drug used with radiation. The treatment plan is made just for the child, considering the tumor’s molecular makeup.
| Chemotherapy Agent | Typical Use | Key Considerations |
| Temozolomide | Concurrent with radiation therapy | Molecular characteristics of the tumor |
| Other agents | Adjuvant therapy | Patient’s overall health and response |
Multidisciplinary Treatment Teams
Managing pediatric glioblastoma works best with a team of experts. This team includes neurosurgeons, radiation oncologists, pediatric oncologists, neurologists, and supportive care professionals. Working together, they cover all aspects of care, from diagnosis to after treatment.
We stress the need for a team effort. This ensures each child gets the full support they need during treatment.
Fact 7: Advanced and Emerging Treatments
New treatments for pediatric glioblastoma are being developed. This gives hope for better results. Doctors are looking into new ways to fight this tough disease.
Molecular Targeted Therapies are being studied. They aim to target glioblastoma cells without harming healthy tissue. These therapies focus on the specific genetic flaws that cause cancer to grow.
Molecular Targeted Therapies
Researchers are focusing on genetic mutations in pediatric glioblastoma. They want to create drugs that target these mutations. This could lead to more effective treatments with fewer side effects.
For example, therapies for the BRAF V600E mutation are showing promise. This mutation is found in some cases of pediatric glioblastoma. Targeted therapies have been able to slow down tumor growth.
Immunotherapy Approaches
Immunotherapy is another area of research. It uses the immune system to fight cancer. Different strategies, like checkpoint inhibitors and CAR-T cell therapy, are being explored.
Checkpoint inhibitors help the immune system attack cancer cells more effectively. CAR-T cell therapy involves modifying T cells to recognize and destroy glioblastoma cells.
Precision Medicine and Personalized Treatment
Precision medicine is changing how we treat pediatric glioblastoma. It involves analyzing each tumor’s genetic makeup. This helps doctors create treatment plans that fit each patient’s needs.
This approach makes treatments more effective and reduces side effects. It targets the unique traits of each tumor.
There’s hope that these new treatments will improve outcomes for kids with glioblastoma. Ongoing research and trials are key to unlocking these new approaches.
Current Clinical Trials and Research Advancements
The fight against pediatric glioblastoma is getting stronger. New clinical trials and research are changing how we treat this disease. We’re seeing new ways to fight this complex illness.
Ongoing Clinical Trials for Pediatric Glioblastoma
Many trials are looking into new treatments for kids with glioblastoma. They’re testing targeted therapies and immunotherapies. For example, some trials are checking if checkpoint inhibitors and CAR-T cell therapy work well in kids.
These trials are key to finding safe and effective treatments. They help us understand how different kids react to different treatments. This helps us make treatment plans that fit each child’s needs.
Promising Research Directions
Research into precision medicine and molecular profiling is very promising. By knowing the genetic makeup of each tumor, we can create treatments that are just right for each patient. This could lead to better results and fewer side effects.
Studies are also looking into epigenetic modifications and non-coding RNAs in glioblastoma. This could uncover new ways to treat the disease and find early signs of it.
As research keeps moving forward, we’re dedicated to helping kids with glioblastoma. Through teamwork and new ideas, we’re working towards better treatments and outcomes for these young patients.
Supportive Care and Quality of Life Considerations
Supportive care is key for kids with glioblastoma. It helps manage symptoms, side effects, and the emotional impact of the disease and treatment.
Managing Side Effects of Treatment
It’s important to manage side effects to keep kids’ quality of life good. Side effects can include nausea, fatigue, hair loss, and changes in thinking. We use medicines, lifestyle changes, and other therapies to help.
For example, medicines can reduce nausea from chemo. Physical and occupational therapy help kids get stronger and adapt to changes.
| Side Effect | Management Strategy |
| Nausea | Anti-nausea medications, dietary adjustments |
| Fatigue | Rest, physical therapy, energy conservation techniques |
| Hair Loss | Counseling, scalp cooling, wigs or headscarves |
Psychological Support for Children and Families
Psychological support is essential for kids with glioblastoma and their families. The disease and treatment can cause anxiety, depression, and stress.
Support groups let families share their experiences and get support. It’s a powerful way to feel less alone.
By adding supportive care to treatment plans, we improve life for kids with glioblastoma and their families. It helps them face this tough time with dignity and hope.
Conclusion: The Future Outlook for Pediatric Glioblastoma Patients
Looking at pediatric glioblastoma, we see a bright future ahead. New treatments and research are making a big difference. These include advanced surgery, new radiation methods, and targeted chemotherapy.
Our understanding of the tumor is growing, leading to new treatments. Molecular targeted therapies and immunotherapy are being tested in trials. This gives us hope for better outcomes.
The future for kids with glioblastoma looks promising. We’re working hard to improve treatments and support care. Our goal is to give each child and their family the best care possible.
FAQ
What is pediatric glioblastoma?
Pediatric glioblastoma is a rare and aggressive brain tumor in children. It’s a cancer that grows in the brain and is hard to treat.
What are the symptoms of pediatric glioblastoma?
Symptoms vary by age and tumor location. Common signs include headaches, nausea, vomiting, seizures, and changes in behavior. Early recognition is key for treatment.
How is pediatric glioblastoma diagnosed?
Diagnosis uses MRI, CT scans, biopsy, and pathological exam. Molecular and genetic tests help understand the tumor for treatment planning.
What are the types of glioblastoma that occur in children?
Children can get different types, like classic, giant cell, and epithelioid glioblastoma. Each type affects treatment differently.
What are the standard treatment approaches for pediatric glioblastoma?
Treatment includes surgery, radiation, and chemotherapy. The plan is based on the child’s needs and tumor type.
Are there any advanced or emerging treatments for pediatric glioblastoma?
Yes, new treatments like molecular therapies and immunotherapy are being explored. They aim to improve outcomes and offer hope.
What is the role of supportive care in pediatric glioblastoma?
Supportive care helps manage treatment side effects and provides psychological support. It’s vital for improving quality of life.
What are the current research advancements in pediatric glioblastoma?
Research focuses on understanding the disease and finding new treatments. Clinical trials are testing promising approaches, bringing hope for better outcomes.
How does pediatric glioblastoma differ from adult glioblastoma?
Pediatric glioblastoma has different genetic and molecular characteristics than adult forms. Tailored treatments are needed for children.
What is the future outlook for pediatric glioblastoma patients?
The outlook is improving with new treatments and research. Continued progress offers hope for better outcomes for children with this condition.
References
- Peker, S., et al. (2021). Clinical features and prognostic factors of pediatric glioblastoma: Report of 38 cases. European Journal of Pediatrics, 180(12), 3581-3591. https://www.sciencedirect.com/science/article/abs/pii/S1878875021008640



































