
How do I treat pediatric ITP? Follow the latest pediatric ITP treatment guidelines. This crucial guide details the most powerful and effective strategies.
Pediatric Immune Thrombocytopenic Purpura (ITP) is a condition where the immune system attacks platelets. Platelets are key to blood clotting. This autoimmune disorder can lower platelet counts, raising the risk of bleeding. Luckily, up to 80% of kids with ITP get better on their own within six months.
For kids needing therapy, the aim is to stop bleeding. First-line treatments are corticosteroids and intravenous immune globulin (IVIg). These help boost platelet counts. Researchers are also looking into new treatments like avatrombopag for ITP.
Key Takeaways
- Understanding ITP is key to managing it well.
- Most children with ITP recover without treatment.
- First-line treatments include corticosteroids and IVIg.
- New therapies are being developed to manage ITP.
- The goal of treatment is to prevent bleeding complications.
Understanding Pediatric Immune Thrombocytopenic Purpura
It’s important to understand Pediatric ITP well for the right treatment. Pediatric Immune Thrombocytopenic Purpura (ITP) occurs when a child has too few platelets. This happens because their body destroys platelets and doesn’t make enough new ones.
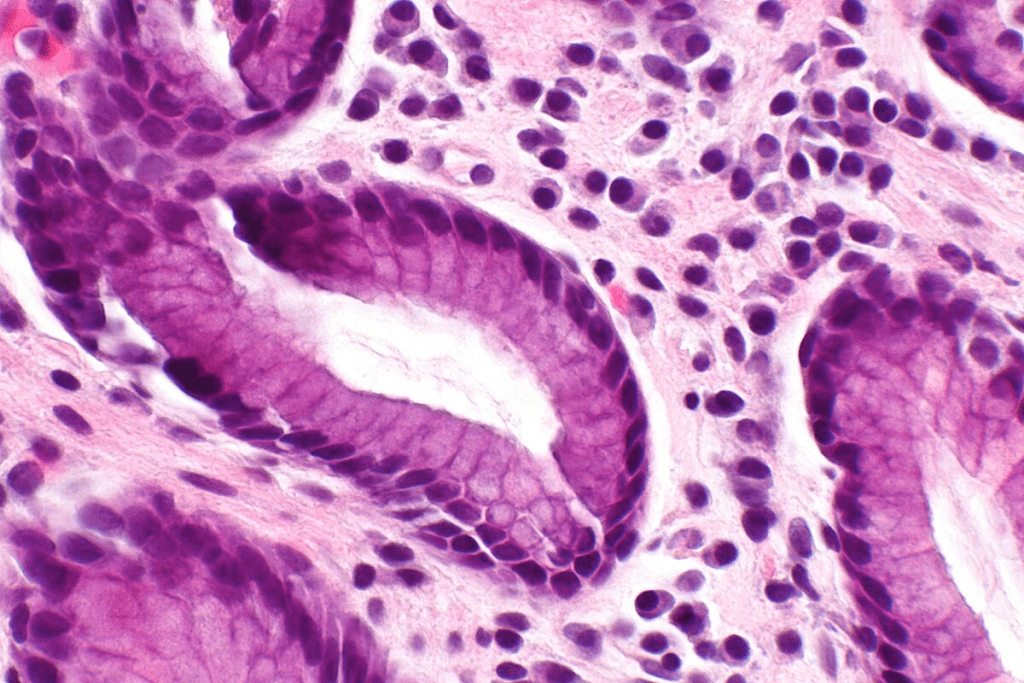
Pathophysiology of ITP in Children
ITP in kids is caused by the immune system attacking platelets. This usually starts after a viral infection. Autoantibodies mark platelets for destruction, leading to low platelet counts.
Impaired platelet production also plays a part. The bone marrow can’t keep up with the loss of platelets. Knowing this helps doctors find better treatments.
Clinical Manifestations and Symptoms
Children with ITP may show different symptoms because of low platelets. They might have bruising, bleeding, and a petechial rash. How bad these symptoms are can vary a lot.
Some kids might not show any symptoms at all. They might only find out they have ITP when they get blood tests. Others might have serious bleeding that needs quick medical help. Spotting these symptoms early is key the right treatment.
Diagnosis and Initial Assessment
To diagnose pediatric ITP, we need a detailed approach. This includes looking at the patient’s medical history and doing a physical exam. We also check for signs and lab results to make an accurate diagnosis.
The first step is a complete blood count (CBC). This test shows if the platelet count is low, which is common in ITP. We might also do other tests to rule out other reasons for low platelets.
Differential Diagnosis
It’s important to tell pediatricians ITP apart from other conditions that can cause low platelets. We look at things like leukemia, lymphoma, and other bone marrow problems. A detailed check helps find the real cause of low platelets.
The process of figuring out the difference involves:
- Complete Blood Count (CBC)
- Bone marrow aspiration (in some cases)
- Viral infection screening
- Imaging studies (if needed)
Risk Stratification
Knowing the risk level is key to managing pediatric ITP. We use bleeding scores to see how bad the bleeding is. This helps us decide how to treat the patient.
| Bleeding Score | Clinical Features | Risk Level |
| 0-1 | Petechiae, mild bruising | Low |
| 2-3 | Moderate bleeding, some mucosal bleeding | Moderate |
| 4-5 | Significant mucosal bleeding, life-threatening bleeding | High |
Understanding pediatric ITP’s diagnosis and initial steps is vital. This includes figuring out the difference and knowing the risk level. Our goal is to reduce bleeding risks and improve life quality for these children.
When to Treat vs. Observation Approach
When dealing with pediatric ITP, doctors must decide between treating and watching. This choice depends on how low the platelet count is, if there are any bleeding signs, and the risk of more bleeding. These factors are key in making a decision.
Benefits of Watchful Waiting
Not every child with ITP needs to start treatment right away. Watching and waiting can be good. It avoids the side effects of treatment and lets some kids get better on their own.
Monitoring Protocols for Untreated Patients
For kids not getting treatment, regular checks are important. Doctors will keep an eye on platelet counts and watch for bleeding signs. They also teach families to know when to seek help fast.
American Society of Hematology Guidelines
The American Society of Hematology has guidelines for doctors. They say treatment should focus on the risk of bleeding, not just the platelet count.
Risk-Based Treatment Algorithms
Doctors use special plans to match treatment to each patient’s risk. These plans look at how low the platelet count is, any bleeding, and other factors that might affect bleeding risk.
| Risk Category | Platelet Count | Bleeding Symptoms | Recommended Approach |
| Low Risk | >20,000/μL | No significant bleeding | Observation |
| Moderate Risk | 10,000-20,000/μL | Minor bleeding | Close monitoring, consider treatment |
| High Risk | <10,000/μL | Significant bleeding | Treatment |
First-Line Treatment Options
First-line treatments for pediatric ITP are key to managing the condition well. The main goal is to quickly increase platelet counts and prevent bleeding.
Intravenous Immune Globulin (IVIg)
IVIg is a common first-line treatment for pediatric ITP. It helps by reducing the immune system’s platelet destruction. The usual dose is 1g/kg, and it might be given again based on how the patient responds.
Anti-D Immunoglobulin
Anti-D immunoglobulin is an option for Rh-positive patients. It works by coating red blood cells, which are then removed by the spleen. This reduces platelet destruction.
Platelet Transfusions
Platelet transfusions are usually for patients with severe bleeding or at high risk. They temporarily increase platelet counts.
Combination Therapy Approaches
Some patients might do better with combination therapy. This means using more than one treatment at a time. For example, IVIg with corticosteroids can be effective in some cases.
The choice of first-line treatment depends on several factors. These include the severity of thrombocytopenia, the presence of bleeding symptoms, and the patient’s overall health.
| Treatment Option | Mechanism of Action | Typical Dosage |
| IVIg | Reduces the immune destruction of platelets | 1g/kg |
| Anti-D Immunoglobulin | Coats red blood cells for removal by the spleen | 50-75 mcg/kg |
| Platelet Transfusions | Provides a temporary increase in platelet count | Variable |
Second-Line Therapies for Persistent ITP
For kids with persistent ITP who don’t get better with first treatments, second-line therapies are an option. These treatments are for those with chronic or ongoing ITP. The goal is to lessen symptoms and improve life quality.
Second-line therapies are tried after first treatments like IVIg or corticosteroids don’t work well. The right therapy depends on the patient’s health, how bad their symptoms are, and how they’ve reacted to other treatments.
Rituximab
Rituximab is a monoclonal antibody that targets B cells involved in ITP. It helps by reducing the immune system’s attack on platelets.
Research shows rituximab can help some kids with chronic ITP. But not all kids will respond to it.
Immunosuppressive Agents
Immunosuppressive agents like azathioprine, cyclosporine, or mycophenolate mofetil are another option. They suppress the immune system’s abnormal response, reducing platelet destruction.
Using these agents requires careful monitoring because of possible side effects. There’s a higher risk of infections and long-term risks like cancer. The right agent and dosage depend on the patient.
We weigh the benefits and risks of second-line therapies for each child with persistent ITP. Our goal is to find the best outcome while avoiding side effects.
Surgical Management and Splenectomy
For kids with severe ITP, surgery is often needed. Splenectomy is a key procedure used for those who don’t get better with medicine.
Surgical Approaches and Techniques
Splenectomy can be done in different ways. The old method uses a big cut, while the new laparoscopic way uses small cuts. Laparoscopic splenectomy is often preferred because it hurts less, keeps you in the hospital shorter, and you get better faster.
Post-Splenectomy Care and Vaccination
After the surgery, patients need close watch to avoid infections. Post-splenectomy vaccination is key, with shots for pneumococcus, meningococcus, and Haemophilus influenzae type b. We also watch for infection signs and teach families about risks and how to handle them.
Neonatal and Infant ITP
ITP is rare in babies and linked to the om’s ITP. We handle it carefully because of the risks and different symptoms. We team up with neonatologists and pediatric hematologists to treat each baby’s needs.
Adolescent Patients
Teenagers with ITP face special challenges, like the emotional toll of chronic illness. We think about their mental health and life quality when deciding treatment. Splenectomy might be an option for teens with severe ITP, based on their situation and wishes.
In summary, surgery, like splenectomy, is a big part of treating pediatric ITP. We look at each patient’s unique situation to choose the best treatment.
Conclusion: Optimizing Care for Children with ITP
Pediatric Immune Thrombocytopenic Purpura (ITP) is a complex condition. It needs a detailed and team-based approach to manage it well. We’ve talked about different treatments to help children with ITP.
The American Society of Hematology guidelines help in treating pediatric ITP. They stress the need for care that fits each child and treatment plans based on risk. Knowing how ITP works and its symptoms helps doctors choose the right ITP treatment options.
We’ve seen how watching closely can help, and the benefits of treatments like intravenous immune globulin (IVIg) and anti-D immunoglobulin. Sometimes, second-line treatments like rituximab are needed. Surgery, like removing the spleen, is also an option for some.
By following pediatric ITP treatment guidelines and keeping up with new research, we can better help children with ITP. It’s key to keep researching and tailor care to each child’s needs.
FAQ’s:
What is pediatric ITP?
Pediatric ITP, or Immune Thrombocytopenic Purpura, is a condition where the body destroys platelets. This leads to a low platelet count. It increases the risk of bleeding.
What are the symptoms of pediatric ITP?
Symptoms include bruising, bleeding, and a petechial rash. These happen because of the low platelet count.
How is pediatric ITP diagnosed?
Doctors use a detailed evaluation to diagnose pediatric ITP. This includes a medical history, physical exam, and lab tests. They check for other causes of low platelets.
What is the goal of treatment for pediatric ITP?
Treatment aims to prevent bleeding by raising the platelet count. This is the main goal.
When is treatment necessary for pediatric ITP?
Treatment is not always needed. It depends on symptoms, platelet count, and bleeding risk.
What are the first-line treatment options for pediatric ITP?
First-line treatments include IVIg, anti-D immunoglobulin, and corticosteroids. They work to quickly increase platelets.
What is the role of watchful waiting in pediatric ITP?
Watchful waiting is for mild cases. It means monitoring without treatment. It can lead to spontaneous recovery.
What are the benefits and risks of splenectomy in pediatric ITP?
Splenectomy is for those who don’t respond to medicine. It can cure ITP but has risks. It requires post-surgery care and vaccinations.
What are the newer agents used in the treatment of pediatric ITP?
New agents like avatrombopag are used for treatment. They offer options for those not responding to traditional therapies.
How is the risk of bleeding complications assessed in pediatric ITP?
Bleeding risk is assessed with bleeding scores. These scores help decide treatment and identify high-risk patients.
What is the role of combination therapy in pediatric ITP?
Combination therapy uses multiple treatments. It’s effective for those not responding to single treatments.
What are the immunosuppressive agents used in the treatment of pediatric ITP?
Immunosuppressive agents, like rituximab, are used as second-line treatments. They aim to stop platelet destruction by the immune system.
How is pediatric ITP managed in different age groups?
Management varies by age. Neonates and infants need special care. Adolescents face unique challenges and needs.
References
- Pietras, N. M. (2024). Immune Thrombocytopenia. In StatPearls. National Library of Medicine. https://www.ncbi.nlm.nih.gov/books/NBK562282/
Neufeld, E. J., & Fletcher, S. K. (2023). Treatment Landscape in Pediatric Immune Thrombocytopenia. Pediatric Blood & Cancer, 70(7), e31758. https://onlinelibrary.wiley.com/doi/10.1002/pbc.31758





