Last Updated on October 21, 2025 by mcelik

Cancer in children is a tough diagnosis that hits the whole family hard. Childhood cancer is rare, but it’s a top cause of death in kids. Pediatric oncology provides specialized support and care for children with cancer. Understand pediatric oncology and how specialists care for children with cancer.
Pediatric oncology deals with diagnosis, treatment, and management of cancers in kids. It’s not just about treating cancer. It also includes care that helps the child feel better overall. We’re trained to tackle the special challenges of treating cancers in kids, who are always growing.
Key Takeaways
- Understanding pediatric oncology is key for the right care in children with cancer.
- Pediatric oncology takes a full approach to treating childhood cancers.
- Supportive care is essential for kids with cancer.
- Healthcare providers need special training for kids with cancer.
- Childhood cancer treatment needs a team effort.
Overview of Pediatric Oncology
Pediatric oncology is a special field of medicine. It deals with diagnosing, treating, and caring for children with cancer. This field is different from adult oncology because it focuses on the unique needs of kids.
Cancer in children is rare but needs special care. Pediatric oncology has grown to offer treatments that fit a child’s age. It knows that kids and adults have different types of cancer.
Definition and Scope
Pediatric oncology is about treating children with cancer. It involves a team of doctors and specialists. They work together to give kids the best care.
This field covers many areas. It includes diagnosing, treating, and supporting kids with cancer. It also helps with the physical and emotional effects of cancer on kids and their families.
“The care of children with cancer requires a multidisciplinary team approach, with pediatric oncologists playing a central role in coordinating care.”
– A leading pediatric oncology expert
Importance in Child Health
Pediatric oncology is key for kids’ health. It provides care that fits a child’s age and needs. This helps improve survival rates and quality of life for kids with cancer.
Early diagnosis and treatment are vital in pediatric oncology. The field stresses the importance of quick and right actions. This helps improve outcomes for kids with cancer.
| Aspect | Pediatric Oncology | Adult Oncology |
| Cancer Types | Leukemia, Neuroblastoma, Wilms Tumor | Carcinomas (Breast, Lung, Colon) |
| Treatment Approach | Tailored to the child’s age and development | Based on cancer type and stage |
| Care Focus | Family-centered, supportive care | Primarily disease-focused |
The table shows big differences between pediatric and adult oncology. These differences include cancer types, treatment methods, and care focus.
Common Types of Pediatric Cancers
It’s important to know about the different types of pediatric cancers. This knowledge helps doctors find and treat cancer better. Each type of cancer needs a special plan based on the child’s situation.
Leukemia
Leukemia is the most common cancer in kids. It affects the blood and bone marrow, causing too many bad white blood cells. Symptoms include feeling very tired, looking pale, and getting sick a lot. Doctors usually treat it with chemotherapy. Sometimes, they also do a bone marrow transplant.
Brain Tumors
Brain tumors are also common in kids. They can be either good or bad and grow at different rates. Symptoms depend on where and how big the tumor is. They might include headaches, feeling sick, and problems with the nervous system. Doctors use surgery, radiation, and chemotherapy to treat them. They often use these methods together.
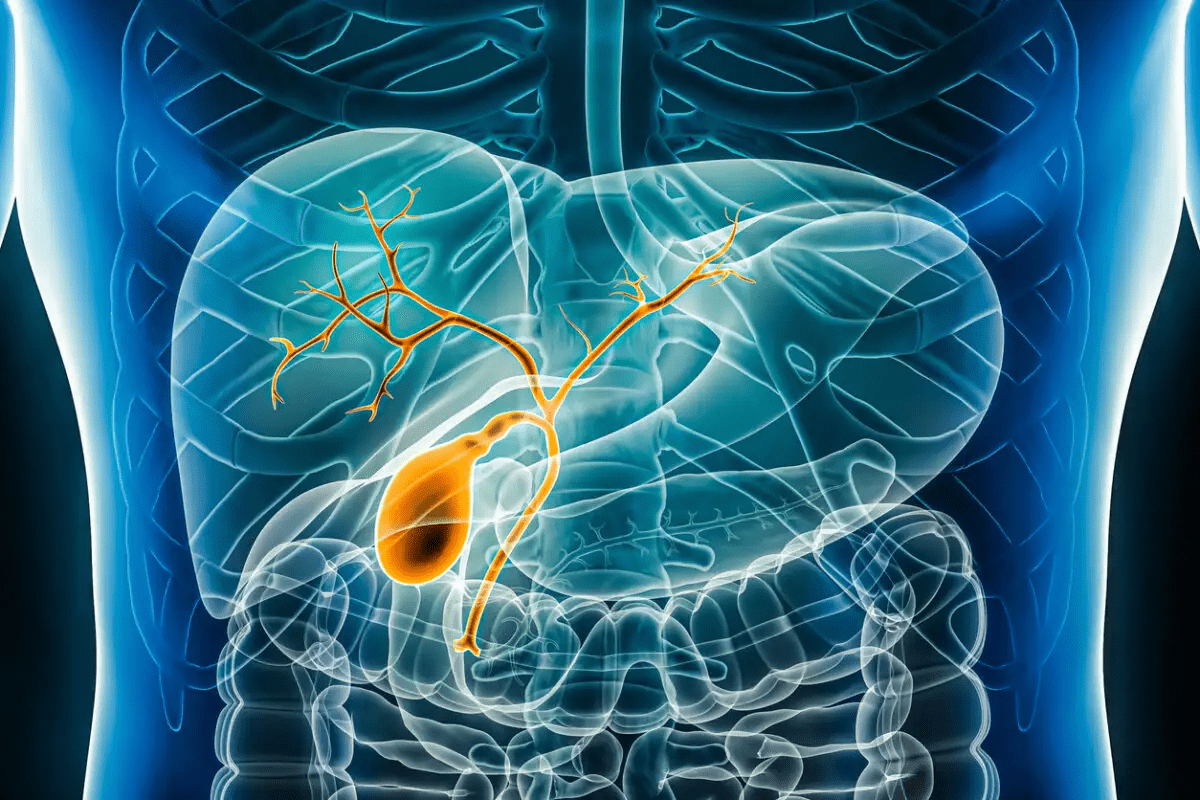
Neuroblastoma
Neuroblastoma starts in nerve tissue, often in the adrenal glands. It’s most found in young kids. Symptoms can be different, like a lump in the neck or belly. In serious cases, symptoms can show the cancer has spread. Treatment depends on how serious the cancer is. It might include surgery, chemotherapy, and radiation.
These cancers need quick diagnosis and good treatment to help kids get better. Thanks to ongoing research, we’re getting better at understanding and treating these diseases.
Symptoms and Diagnosis
Finding cancer in kids is hard because the early signs are not clear. Parents and doctors must watch closely. Cancer in children can look like common illnesses, making it hard to diagnose. We will talk about early signs of cancer in kids and how doctors find out for sure.
Early Symptoms to Watch For
Early signs of cancer in kids are often vague. They might include constant tiredness, unexpected weight loss, and frequent fevers. Kids might also show pale skin, bruises, or tiny spots under the skin. It’s key for parents to know these signs and get help if they don’t go away or get worse.
- Persistent fatigue or weakness
- Unexplained weight loss or loss of appetite
- Recurrent fevers without apparent cause
- Pain in bones or joints
- Easy bruising or petechiae
Diagnostic Procedures in Pediatric Oncology
When early signs show up, doctors use several tests to find cancer. These tests include X-rays, CT scans, and MRI scans. They also do blood tests and bone marrow biopsies.
| Diagnostic Procedure | Purpose |
| Imaging Studies (X-rays, CT, MRI) | To see the tumor and know its size and where it is |
| Blood Counts | To find out if there are abnormal blood cells that indicate cancer |
| Bone Marrow Biopsy | To check the bone marrow for cancer cells |
Treatment Options

Treating pediatric cancer is a complex task. It involves several therapies. The right treatment depends on the cancer type, stage, and the child’s health. We’ll discuss the main options: chemotherapy, radiation therapy, and surgical interventions.
Chemotherapy
Chemotherapy uses drugs to kill cancer cells. It’s often used with other treatments like surgery or radiation. This method targets cancer cells in the body.
Chemotherapy can cause side effects like nausea and hair loss. But, these effects are usually temporary and can be managed.
Radiation Therapy
Radiation therapy kills cancer cells with high-energy rays. It’s used for localized tumors or to ease symptoms. We plan it carefully to protect healthy tissues.
Radiation therapy’s side effects depend on the treatment area and dose. Common effects include fatigue and hair loss.
Surgical Interventions
Surgical interventions remove tumors or help diagnose cancer. Surgery can be used alone or with other treatments. We team up with skilled surgeons for the best care.
The goal of surgery is to remove the tumor while keeping healthy tissue. The surgery type depends on the tumor’s location and size, and the child’s health.
In conclusion, treating pediatric cancer needs a team effort. We create personalized plans using chemotherapy, radiation therapy, and surgical interventions. This approach helps us achieve the best results for our young patients.
The Role of Pediatric Oncologists
Pediatric oncologists are medical experts focused on helping kids with cancer. They play a key role in finding, treating, and managing childhood cancers.
What They Do
Pediatric oncologists diagnose and treat kids’ cancers with various methods. This includes chemotherapy, radiation, and surgery. They work with a team to create treatment plans that fit each child’s needs.
They don’t just treat the cancer. They also help manage symptoms and side effects. This ensures kids have the best quality of life possible.
Necessary Qualifications and Training
To be a pediatric oncologist, one needs a lot of education and training. This includes medical school, residency in pediatrics and oncology, and sometimes fellowship training in pediatric oncology.
They must understand childhood cancers well. They also need to communicate well with kids and their families. This helps provide emotional support during tough times.
The qualifications and training of pediatric oncologists are vital. They keep up with new research and treatments. This way, they can give kids the best care possible.
Supportive Care and Compassionate Services
Supportive care in pediatric oncology
We know that supportive care is key in treating kids with cancer. It helps both the patients and their families feel better. This care includes many services to ease pain and improve life quality.
Importance of Palliative Care
Palliative care is a big part of supportive care in treating kids with cancer. It helps manage symptoms, pain, and stress from treatment. This care makes life better for patients.
- Symptom management
- Pain relief
- Emotional support
A team of experts provides palliative care. They work with the patient’s doctor to give full care. This team includes doctors, nurses, and social workers trained for kids with cancer.
Psychological Support for Patients and Families
Psychological support is also very important in treating kids with cancer. Families often feel anxious, depressed, and scared. Our support helps them deal with these feelings.
We offer different kinds of psychological support. This includes:
- Counseling for patients and family members
- Support groups for parents and siblings
- Recreational therapy to help children feel normal
By giving full supportive care, we can really help kids with cancer and their families. It’s not just about treating the disease. It’s about caring for the whole child and their loved ones.
Clinical Trials in Pediatric Oncology
Clinical trials are key in advancing pediatric oncology. They test new treatments for kids with cancer. These studies help improve care for children with cancer.
How They Work
Clinical trials in pediatric oncology are designed to ensure new treatments are safe and work well. We start by asking a research question, like comparing two treatments for a specific cancer. Then, participants are randomly assigned to a group, and their outcomes are closely watched.
The process has several phases. Phase 1 checks the safety and dosage of a new treatment. Phase 3 compares the new treatment with the current standard. We collect important data on how well the treatment works, its side effects, and long-term effects.
Benefits and Considerations
Being in a clinical trial has many benefits for kids with cancer. They get access to new treatments, close monitoring, and help advance pediatric oncology.
Key benefits include:
- Access to innovative treatments not yet widely available
- Close monitoring and care by a specialized team
- Contribution to the development of future treatments for pediatric cancer
But, there are also things to think about. There’s the risk of unknown side effects, the chance of getting the standard treatment, and the need for consent from parents or guardians.
Choosing to join a clinical trial is a big decision. Our team is here to give you all the information and support you need.
Long-Term Effects of Treatment
As kids who had cancer grow up, they might face long-term effects from their treatment. These can be physical, emotional, or social. Each survivor’s experience is different. We focus on understanding and helping with these challenges to give them the best care.
Survivorship Issues
Survivors of pediatric cancer face many challenges. These can include new cancers, organ problems, and emotional struggles. Early identification and intervention are key to managing these issues well.
We create personalized follow-up care plans for each survivor. This includes watching for late effects and helping with emotional and social issues.
Monitoring for Late Effects
Watching for late effects is vital in survivorship care. Regular check-ups and screenings help catch and manage problems early. Survivors and their families should stay involved in their care for the best results.
A good monitoring plan includes:
- Regular health check-ups
- Screenings for secondary cancers
- Assessment of organ function
- Support for psychological well-being
By being proactive and informed in survivorship care, we can enhance the lives of pediatric cancer survivors. Our goal is to offer ongoing support and guidance on their journey.
Resources for Families
Families dealing with pediatric cancer find solace and support through various resources. We know that a child’s cancer diagnosis affects the whole family. So, it’s important to have access to all the support they need.
Support comes in many ways. We aim to give families the tools and info they need to get through this tough time. This includes connecting them with organizations and support groups for emotional and practical help.
Organizations and Support Groups
Many organizations help families of children with cancer. They offer:
- Emotional support through counseling and support groups
- Practical help, like financial aid and transportation services
- Info resources, including educational materials and workshops
Groups like the Children’s Cancer and Leukemia Group (CCLG) and the Pediatric Cancer Research Foundation are key. They help families deal with the diagnosis and treatment of pediatric cancer.
Educational Materials
Educational materials are vital for families. They provide info on the child’s condition, treatment options, and managing side effects. We offer:
- Brochures and pamphlets on pediatric cancer
- Workshops and seminars on nutrition, pain management, and coping
- Online resources, like webinars and video tutorials
These materials aim to empower families with the knowledge they need. By giving them reliable info, we hope to reduce anxiety and uncertainty. This lets families focus on their child’s recovery.
We are committed to supporting families every step of the way. By providing resources, organizations, and educational materials, we aim to positively impact children with cancer and their families.
Future Trends in Pediatric Oncology
The field of pediatric oncology is changing fast. This is thanks to new research and treatments. We’re moving towards more targeted and personalized care. This change is expected to make treatments better and reduce side effects for kids with cancer.
Breakthroughs in Research
Genomic sequencing and molecular diagnostics are leading to big discoveries. They help us understand the genetic causes of pediatric cancers. This knowledge is helping create new, targeted therapies. These are showing great promise in early trials.
Emerging Treatment Modalities
New treatments like immunotherapy and CAR-T cell therapy are being tested. They aim to help kids with cancers that don’t respond to standard treatments. These therapies are being studied in trials, giving hope to families and patients.
As research keeps moving forward, we’re looking forward to better outcomes and fewer side effects. The future of pediatric oncology looks bright. New trends and technologies are set to change the field for the better.
FAQ
What is pediatric oncology?
Pediatric oncology is the study and treatment of cancers in kids. We focus on the unique needs of children with cancer. Our goal is to help them feel better overall.
How does pediatric oncology differ from adult oncology?
Pediatric oncology deals with cancers in children, which are different from adult cancers. Kids’ bodies are growing, and their cancers can grow fast. So, we tailor treatments to fit their needs.
What are the most common types of pediatric cancers?
Common pediatric cancers include leukemia, brain tumors, and neuroblastoma. We also see lymphoma and Wilms tumor. Each cancer type needs its own treatment plan.
What are the early symptoms of pediatric cancer?
Early signs of pediatric cancer vary by type. Look out for persistent fatigue, unexplained weight loss, pain, or swelling. Fever, bruising, or bleeding are also signs. If you notice these, see a doctor right away.
How is pediatric cancer diagnosed?
Diagnosing pediatric cancer involves tests like X-rays, CT scans, and biopsies. Blood tests also play a role. These tools help us understand cancer and plan treatment.
What treatment options are available for pediatric cancer?
Treatments include chemotherapy, radiation, and surgery. We choose the best mix for each child’s cancer and health. This approach helps us fight the cancer effectively.
What is the role of a pediatric oncologist?
Pediatric oncologists specialize in treating kids’ cancers. We work with a team to provide care. This includes treatments and support for the child and family.
What is palliative care in pediatric oncology?
Palliative care helps manage symptoms and support families. It’s part of our treatment plans. This care addresses physical, emotional, and social needs.
What are clinical trials in pediatric oncology?
Clinical trials test new cancer treatments. We conduct them to find better, safer options. Joining a trial is optional, and we explain the risks and benefits.
What are the long-term effects of pediatric cancer treatment?
Treatment effects vary by type and intensity. We watch for late effects like organ damage or secondary cancers. Our goal is to manage these effects and support overall health.
What resources are available to families of children with cancer?
We offer support groups, organizations, and educational materials. These resources help families cope emotionally and navigate healthcare. They also provide valuable information on managing the child’s condition.
What are the future trends in pediatric oncology?
Future trends include new research and treatments. There’s also a focus on survivorship care. These advancements aim to improve outcomes, reduce effects, and enhance survivors’ quality of life.
References:
- Wedekind, M. F. (2018). Pediatric Cancer Immunotherapy: Opportunities and Challenges. Frontiers in Immunology, 9, 1018. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6153971/