Last Updated on November 13, 2025 by
How is pediatric thrombocytopenia treatment? Get the amazing guide to managing low platelets in children. Powerful strategies for quick and effective recovery.
Pediatric thrombocytopenia is a condition where kids have low platelet counts. It’s often caused by Immune Thrombocytopenia (ITP). We work hard to give the best care for this challenge.
At Liv Hospital, we lead in ITP treatment with the latest methods. We use corticosteroids, IVIG, and TPO-RAs. Our goal is to offer top-notch support with the newest research and ideas.
Key Takeaways
- Immune Thrombocytopenia (ITP) is the most common cause of pediatric thrombocytopenia.
- Up to 30% of children develop chronic ITP, requiring further intervention.
- Liv Hospital offers a range of therapies, including corticosteroids, IVIG, and TPO-RAs.
- Our approach incorporates the latest academic protocols and innovative solutions.
- Comprehensive support is available for international patients.
Understanding Pediatric Thrombocytopenia
To understand pediatric thrombocytopenia, we need to look at its types and causes. It’s a condition where kids have low platelet counts. This can make them more likely to bleed.
Definition and Normal Platelet Values in Children
Definition and Normal Platelet Values in Children
Pediatric thrombocytopenia means kids have fewer platelets than normal. Platelet counts should be between 150,000 and 450,000 per microliter of blood. Knowing these numbers is key to spotting thrombocytopenia.
“Diagnosing thrombocytopenia means finding counts below normal and checking for other reasons for low counts,” says recent guidelines.
Types of Pediatric Thrombocytopenia
Pediatric thrombocytopenia has different types based on its causes and symptoms. The main types are:
- Immune thrombocytopenia (ITP), when the immune system attacks platelets by mistake.
- Non-immune thrombocytopenia, caused by bone marrow problems, infections, or medicines.
Each type needs its own treatment plan.
Immune vs. Non-immune Causes
It’s important to tell the difference between immune and non-immune causes. Immune thrombocytopenia (ITP) happens when the immune system attacks platelets. Non-immune causes include bone marrow failure, infections, and some medicines.

Knowing the cause helps pick the best treatment. “Getting the right diagnosis is key to managing pediatric thrombocytopenia well,” say experts.
Pathophysiology of Immune Thrombocytopenia (ITP)
ITP’s pathophysiology is complex. It involves autoantibodies and immune responses that cause thrombocytopenia. This affects how platelets are made and destroyed, making it important to understand for treatment.
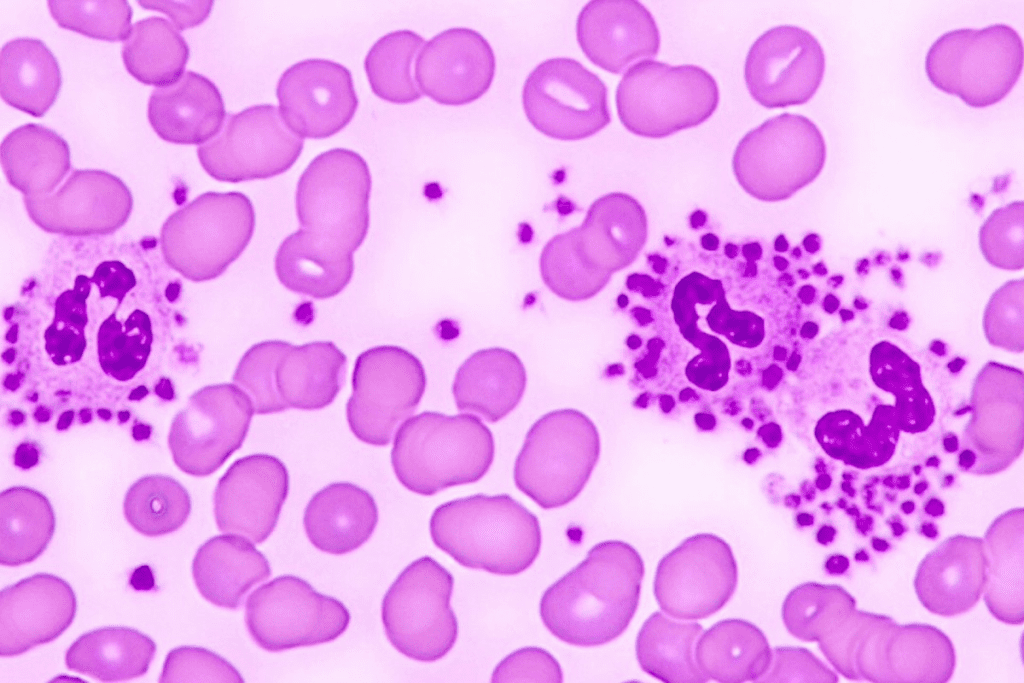
Autoimmune Mechanisms
ITP is an autoimmune disease. It happens when the body makes autoantibodies against platelet glycoproteins. These autoantibodies mark platelets for destruction, mainly in the spleen.
Autoantibody production is a major factor. Cytotoxic T cells also help in destroying platelets.
Platelet Destruction Process
The spleen is key in destroying platelets in ITP. It removes antibody-coated platelets from the blood.
- Autoantibodies bind to platelet surface glycoproteins.
- The spleen recognizes and removes these antibody-coated platelets.
- This process shortens the platelet lifespan.
Impaired Platelet Production
ITP also affects platelet production. Autoantibodies and cytotoxic T cells target megakaryocytes. These are bone marrow cells that make platelets.
Epidemiology and Clinical Significance
The study of pediatric Immune Thrombocytopenia (ITP) shows us how common it is and why it matters. Knowing this helps doctors and researchers find better ways to treat it.
Prevalence in Pediatric Populations
About 1 in 20,000 kids get ITP each year. It can happen at any age, but most cases are in kids aged 2 to 5. This shows why doctors need to be aware of ITP in kids to catch it early.
Key statistics on pediatric ITP prevalence include:
- Annual incidence of about 5 cases per 100,000 children
- A significant proportion of children develop chronic ITP, which persists beyond 12 months
- Variability in incidence rates across different populations and regions
Age and Gender Distribution
ITP can happen at any age in childhood. Some studies say it’s more common in younger kids. Boys and girls get it about equally, but girls might get it a bit more often in some age groups.
The age and gender distribution of pediatric ITP has implications for diagnosis and management. Knowing this helps doctors spot ITP in kids who show symptoms.
Acute vs. Chronic ITP Statistics
There’s a big difference between acute and chronic ITP. About 70-80% of kids have the acute form, which usually goes away in 6 months. But 20-30% will have chronic ITP. Older kids are more likely to have chronic ITP.
“The distinction between acute and chronic ITP is critical for understanding the outlook and planning treatment.”
Knowing about pediatric ITP helps doctors give the best care to kids with it. By understanding how common it is, who gets it, and the difference between acute and chronic ITP, doctors can tailor treatment for each child.
Clinical Presentation and Symptoms
ITP in kids shows up in many ways, making it important to know its signs. Kids with ITP often get symptoms suddenly. This can be scary for them and their families.
Bleeding Manifestations
Signs of bleeding include petechiae, purpura, and bleeding in the mouth or gut. Petechiae are tiny spots on the skin from small bleeds. Purpura are bigger bruises. Nosebleeds, gum bleeding, or bleeding in the gut are signs of mucosal bleeding.
Severity Classification
ITP’s severity depends on the platelet count and bleeding signs. Severe ITP means serious bleeding that needs quick doctor help. Knowing how severe it is helps decide the right treatment and ITP medication.
Warning Signs Requiring Immediate Attention
Some signs mean you need to see a doctor right away. These include bad headaches, vomiting, or signs of bleeding inside, like belly pain or bleeding in the gut. It’s key for families to know these signs to act fast.
Even though there’s no cure, catching it early and treating it right can help a lot. This is good news for kids with ITP.
Diagnostic Approach to Pediatric Thrombocytopenia
Understanding how to diagnose pediatric thrombocytopenia is key to managing it well. To diagnose immune thrombocytopenia (ITP), doctors use a mix of clinical checks, lab tests, and sometimes, a bone marrow exam.
Laboratory Evaluation
The first step in diagnosing pediatric thrombocytopenia is a detailed lab check. This includes:
- A complete blood count (CBC) to check platelet count and other blood cells.
- A peripheral smear to look at platelet and blood cell shapes.
These tests help spot isolated thrombocytopenia, a key sign of ITP. Other tests might be done to rule out other reasons for low platelets.
Bone Marrow Examination Indications
A bone marrow test is not always needed for ITP, but might be in some cases, like:
- Other blood cell problems or abnormal shapes.
- Not responding to the first ITP treatment.
- Thinking there might be another bone marrow issue.
Differential Diagnosis
ITP diagnosis is mostly about ruling out other conditions. We look at:
- Infections.
- Autoimmune diseases.
- Myelodysplastic syndromes.
- Other bone marrow failure syndromes.
Diagnostic Criteria for ITP
The criteria for ITP include:
- Just low platelets with a count
- Normal hemoglobin and white blood cells.
- Normal or more megakaryocytes in the bone marrow (if done).
- Not seeing other reasons for low platelets.
By using this method, we can accurately diagnose and treat pediatric thrombocytopenia. This ensures the best care for kids with idiopathic thrombocytopenia.
Pediatric Thrombocytopenia Treatment: First-Line Options
Treating pediatric thrombocytopenia, like immune thrombocytopenia (ITP), uses several methods. These aim to quickly raise platelet counts. We look at first-line treatments, like corticosteroids and intravenous immunoglobulin (IVIG), which are proven to work well for ITP.
Corticosteroids help by cutting down on platelet destruction and boosting production. IVIG quickly raises platelet counts, which is key in severe bleeding cases. At Liv Hospital, we customize these treatments for each patient’s needs.
New treatments, like thrombopoietin receptor agonists (TPO-RAs), are showing great promise. They offer options for those who don’t respond to initial treatments or need ongoing care. Our goal is to keep up with the latest in ITP treatment, ensuring the best results for our patients.
FAQ
What is pediatric thrombocytopenia?
Pediatric thrombocytopenia is when kids have too few platelets. The main reason is Immune Thrombocytopenia (ITP).
What are the normal platelet values in children?
Kids usually have 150,000 to 450,000 platelets per microliter of blood. But, this can change a bit depending on the lab.
What causes Immune Thrombocytopenia (ITP) in children?
ITP happens when the body’s immune system attacks platelets. It marks them for destruction, mainly in the spleen.
How is the severity of ITP classified?
ITP’s severity is based on platelet count and bleeding symptoms. It can range from mild to severe.
What are the common symptoms of ITP in children?
Symptoms include petechiae, purpura, and mucosal bleeding. The severity can vary among kids.
How is ITP diagnosed?
Diagnosing ITP involves lab tests like a complete blood count and peripheral smear. Sometimes, a bone marrow exam is needed.
What are the first-line treatment options for pediatric ITP?
First treatments are corticosteroids and Intravenous Immunoglobulin (IVIG). They aim to quickly raise platelet counts.
Are there newer treatments available for ITP?
Yes, newer treatments like Thrombopoietin Receptor Agonists (TPO-RAs) have shown great results in clinical trials.
What is the difference between acute and chronic ITP?
Acute ITP usually gets better on its own. Chronic ITP lasts more than 12 months and needs ongoing care.
How does Liv Hospital approach the treatment of pediatric thrombocytopenia?
Liv Hospital uses the latest medical protocols and innovative care. They focus on both treating the condition and caring for the patient.
References
- Thakur, Y., et al. (2024). Diagnosis and management of immune thrombocytopenia in pediatric patients: A comprehensive review. Journal of Pediatric Hematology/Oncology, 46(9), 497-511. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC11488990/
- Wang, L., et al. (2023). Treatment landscape in pediatric immune thrombocytopenia: Current status and future prospects. Pediatric Blood & Cancer. https://onlinelibrary.wiley.com/doi/10.1002/pbc.31758