Last Updated on December 1, 2025 by Bilal Hasdemir

Endocrine emergencies are serious conditions that need quick medical help. Diabetic ketoacidosis, a big problem for people with diabetes, is one of these urgent cases. Consider pediatrician distance carefully. specific best location tips. Learn why a close doctor is vital for sick visits and emergencies.
Every year, thousands of people around the world face endocrine emergencies. Diabetic ketoacidosis is a potentially life-threatening issue. It happens when the body makes too many ketones, harmful acids.
In this article, we’ll look at what causes diabetic ketoacidosis and other endocrine emergencies. We’ll also talk about how to treat them. It’s very important to get medical help right away.
Key Takeaways
- Diabetic ketoacidosis is a serious complication of diabetes that requires immediate medical attention.
- Endocrine emergencies, including diabetic ketoacidosis, can be life-threatening if not treated promptly.
- Understanding the causes and symptoms of endocrine emergencies is key for effective management.
- Prompt medical intervention is essential for successfully treating endocrine emergencies.
- Diabetic ketoacidosis is marked by high ketone levels in the blood, causing acidosis.
Understanding Endocrine Emergencies
Endocrine emergencies are serious conditions that need quick medical help. They can upset the body’s hormonal balance, causing severe problems if not treated right away.
We will look into what endocrine emergencies are, their causes, symptoms, and why fast medical care is key.
Definition of Endocrine Emergencies
An endocrine emergency is a serious issue with the endocrine system. This system makes hormones that control our body’s functions. Endocrine emergencies can happen due to hormonal imbalances, gland problems, or other health issues.
These life-threatening hormone crises can take many forms, like diabetic ketoacidosis, thyroid storm, or adrenal crisis. Each needs quick and specific treatment.
Common Types and Their Impact
Some common endocrine emergencies include:
- Diabetic ketoacidosis (DKA), a diabetes complication with high blood sugar and ketones.
- Thyroid storm, a severe hyperthyroidism issue.
- Adrenal crisis, when the adrenal glands don’t make enough cortisol and aldosterone, often due to insufficiency.
These conditions can seriously affect the body, impacting organs and systems. For example, DKA can cause dehydration, electrolyte imbalances, and even organ failure if not treated fast.
Condition | Causes | Symptoms |
Diabetic Ketoacidosis (DKA) | High blood sugar, insulin deficiency | Hyperglycemia, ketosis, dehydration |
Thyroid Storm | Untreated or undertreated hyperthyroidism | Tachycardia, hypertension, hyperthermia |
Adrenal Crisis | Adrenal insufficiency, steroid withdrawal | Hypotension, fatigue, nausea |
Medical experts say, “Early recognition and treatment of endocrine emergencies are vital to avoid long-term damage and lower death rates.” Quick medical action can greatly help patients with these critical conditions.
Identifying the Most Common Endocrine Emergency
Hyperglycemic and hypoglycemic emergencies are serious and need quick medical help. They happen when blood sugar levels get too high or too low. This is often due to diabetes mellitus.
Overview of Hyperglycemic Emergencies
Hyperglycemic emergencies happen when blood sugar levels get too high. This can cause serious problems. There are two main types: diabetic ketoacidosis (DKA) and hyperosmolar hyperglycemic state (HHS).
DKA is common in type 1 diabetes and involves ketoacids in the blood. HHS is more common in type 2 diabetes. It’s marked by very high blood sugar and dehydration.
Both DKA and HHS need quick treatment to avoid serious issues. Knowing the difference between them is key to managing them well.
Overview of Hypoglycemic Emergencies
Hypoglycemic emergencies happen when blood sugar levels drop too low. This can cause confusion, loss of consciousness, or even death if not treated fast. Hypoglycemia can be caused by too much insulin, not eating enough, or too much exercise.
It’s important to recognize the early signs of hypoglycemia, like shakiness, sweating, or dizziness. Severe hypoglycemia needs immediate medical help to get blood sugar back to normal.
Symptoms of Hyperglycemic Emergencies
It’s key to know the signs of hyperglycemic emergencies to act fast and avoid serious issues. These emergencies, like diabetic ketoacidosis and hyperosmolar hyperglycemic state, show different symptoms. These symptoms can be mild or severe.
Early Signs and Symptoms
The first signs often include increased thirst and urination. This is because the body is trying to get rid of too much sugar. Other early signs are fatigue, blurred vision, and headaches.
These symptoms can pop up quickly, sometimes in just a few hours or days. They are more noticeable in people with diabetes who haven’t been diagnosed or managed properly.
People with diabetes need to watch for these early signs. Keeping an eye on blood sugar levels and noticing any changes in how you feel is important. This can help catch problems early.
Severe Symptoms to Watch For
If not treated, these emergencies can get worse. Symptoms like confusion, seizures, and even coma can happen. These are very serious and need quick medical help.
Other severe signs include rapid heartbeat, fruity-smelling breath (a sign of ketoacidosis), and shortness of breath. Seeing these as serious and acting fast is vital.
We stress the need to get medical help right away if you see severe symptoms. Quick action can make a big difference in treating hyperglycemic emergencies.
Symptoms of Hypoglycemic Emergencies
Knowing the early signs of hypoglycemic emergencies is key to avoiding serious problems. We’ll cover the main symptoms to help those with diabetes and their caregivers handle these situations well.
Early Warning Signs
Hypoglycemic emergencies start with early signs. If caught early, they can be quickly treated. Look out for:
- Shakiness or tremors
- Sweating
- Confusion or disorientation
- Dizziness or lightheadedness
- Hunger
- Nausea
These symptoms happen when blood sugar drops too low. The body’s nervous system kicks in. It’s vital to treat these signs fast with glucose-rich foods or drinks.
Life-Threatening Symptoms
If hypoglycemia isn’t treated, it can get worse. Severe symptoms include:
- Seizures
- Loss of consciousness or coma
- Cardiac arrhythmias
In extreme cases, it can be deadly. So, it’s critical to act fast when you see early signs. Doctors stress that quick action can greatly improve results.
“Prompt recognition and treatment of hypoglycemia can prevent serious complications and save lives.”
— American Diabetes Association
Knowing how symptoms progress shows why education and awareness are so important. They help manage hypoglycemic emergencies effectively.
Symptom Category | Symptoms | Action Required |
Early Warning Signs | Shakiness, sweating, confusion, dizziness, hunger, nausea | Consume glucose-rich foods or drinks |
Life-Threatening Symptoms | Seizures, loss of consciousness, cardiac arrhythmias | Seek immediate medical attention |
Causes of Hyperglycemic Emergencies
It’s key to know what causes hyperglycemic emergencies. These are serious issues like diabetic ketoacidosis (DKA) and hyperglycemic hyperosmolar state (HHS). They happen when diabetes mellitus isn’t managed well.
Diabetes Mellitus and Its Role
Diabetes mellitus is the main cause of these emergencies. Poor glycemic control is a big risk. It can cause DKA or HHS. It’s vital to manage diabetes well.
Diabetes plays a huge role in these emergencies. People with diabetes must understand their condition. They need to know how to avoid these emergencies.
Other Contributing Factors
Other things can also lead to hyperglycemic emergencies. These include:
- Infections: Infections can cause stress, leading to high glucose levels.
- Medication Non-Adherence: Not taking diabetes meds can raise blood sugar.
- Certain Medications: Some meds, like corticosteroids, can also increase blood sugar.
- Other Medical Conditions: Issues like pancreatitis or trauma can also cause emergencies.
Knowing these factors helps prevent and spot emergencies early.
Causes of Hypoglycemic Emergencies
It’s key to know why hypoglycemic emergencies happen. These emergencies are when blood sugar drops too low. They often come from how we manage diabetes.
Insulin Overdose and Its Consequences
Too much insulin is a big reason for these emergencies. When you take too much, your blood sugar can drop too low. This is because insulin helps your cells use glucose, lowering your blood sugar.
Insulin overdose can happen by mistake. It might be because you miscalculated your dose or didn’t adjust it right. It can also happen if you took the wrong insulin by accident.
Insulin overdose can cause serious problems. It can make you feel confused, lose consciousness, or even be fatal. So, it’s vital for people with diabetes to know the signs and how to treat them.
Food Intake and Activity Level
Other big factors are changes in what you eat and how active you are. Skipping meals or eating less without adjusting your insulin can cause low blood sugar. Also, doing more exercise than usual can make your muscles use more glucose, lowering your blood sugar.
It’s important to match your insulin with your lifestyle. Check your blood sugar often and adjust your insulin or food as needed. Also, learning how to manage your diabetes during illness, travel, or when your routine changes is key.
By knowing these causes and taking steps to prevent them, people with diabetes can lower their risk of emergencies. We stress the need for a detailed diabetes plan. This should include education, regular checks, and flexible treatment options.
Risk Factors for Endocrine Emergencies
It’s important to know the risk factors for endocrine emergencies. This knowledge helps prevent and treat these issues. Lifestyle choices and health conditions can raise the risk of these emergencies.
Lifestyle Factors
Lifestyle choices greatly affect the risk of endocrine emergencies. Diet and exercise habits are key. A diet full of refined sugars and saturated fats can worsen insulin resistance, leading to high blood sugar emergencies.
Being active is also vital. Sedentary lifestyles can lead to insulin resistance and type 2 diabetes. This increases the risk of high blood sugar emergencies. On the other hand, too much exercise can cause low blood sugar in people with diabetes, if they’re on insulin or certain pills.
Underlying Health Conditions
Health conditions also play a big role. Diabetes mellitus is a major concern, as it can cause both high and low blood sugar emergencies. Thyroid disorders can also lead to emergencies. Untreated or under-treated hypothyroidism can cause myxedema coma, a serious condition.
Other chronic health conditions and medications can also affect hormone levels. This increases the risk of endocrine emergencies. People with these conditions should work closely with their doctors to manage their health.
By understanding and addressing these risk factors, we can prevent endocrine emergencies. We can also ensure quick action if they happen.
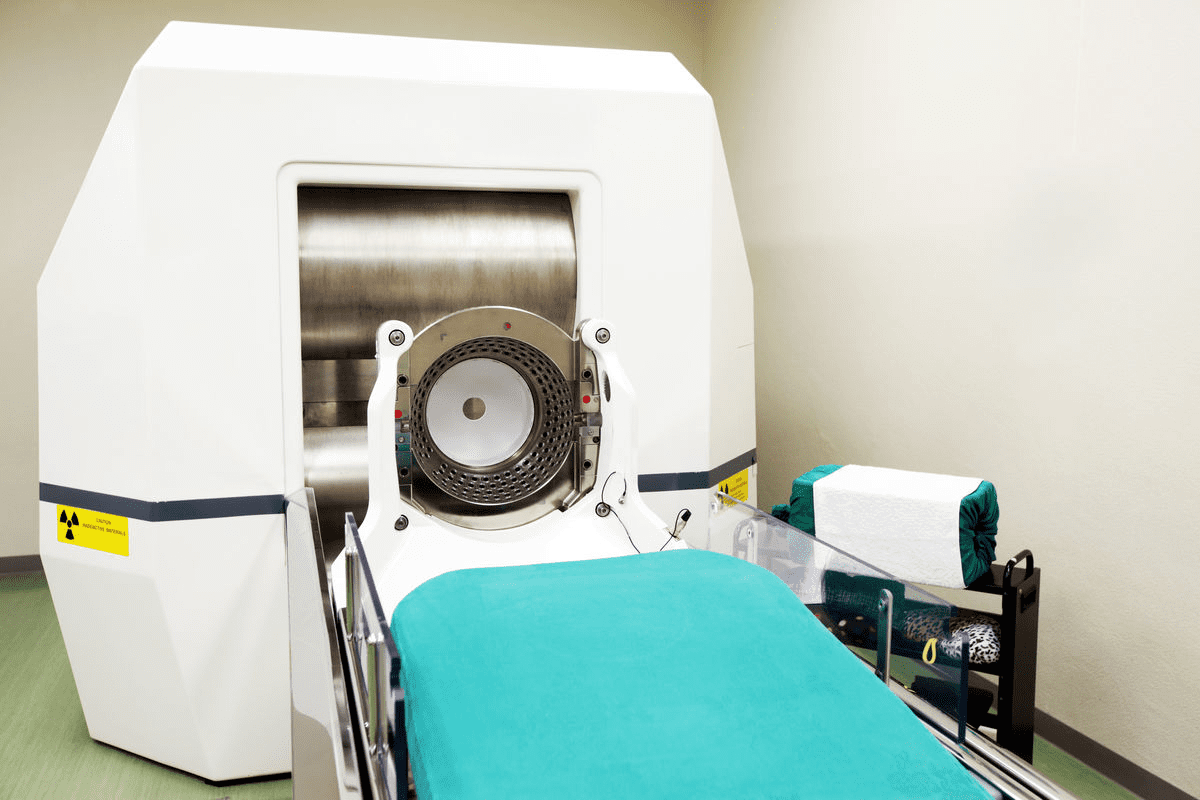
Diagnosis of Endocrine Emergencies
Endocrine emergencies like diabetic ketoacidosis and hypoglycemia need quick and accurate diagnosis. We will look at how we diagnose these conditions. This includes blood sugar monitoring and other important tests.
Blood Sugar Monitoring Techniques
Blood sugar monitoring is key in diagnosing endocrine emergencies. We use glucometry and continuous glucose monitoring systems. These tools help us get accurate blood glucose levels fast.
Getting blood glucose levels right is vital for treating endocrine emergencies. It shows how severe the condition is and helps plan treatment. We stress the need for reliable glucose monitoring devices for accurate readings.
Additional Diagnostic Tests
More tests are needed to fully understand endocrine emergencies. These include electrolyte panels and arterial blood gas analysis. We also do specific tests based on the suspected condition. These help us understand the patient’s situation fully.
Diagnosing endocrine emergencies involves quick checks and detailed tests. By using clinical judgment and test results, we can effectively manage these conditions.
Treatment Options for Hyperglycemic Emergencies
Handling hyperglycemic emergencies needs quick actions and long-term plans. Conditions like diabetic ketoacidosis (DKA) and hyperosmolar hyperglycemic state (HHS) need fast and effective care. This is to avoid serious problems and lower the chance of death or serious illness.
Immediate Interventions
First steps in treating these emergencies aim to stabilize the patient. This includes:
- Fluid Replacement: Giving intravenous fluids to fix dehydration and stabilize blood pressure.
- Insulin Therapy: Using insulin to lower blood sugar and control ketoacidosis.
- Electrolyte Management: Watching and fixing electrolyte imbalances, like potassium, to avoid heart issues.
The American Diabetes Association stresses the need for quick and strong treatment of DKA and HHS. They say it’s key to avoid serious problems. We highlight the need for fast medical help in these cases.
Long-Term Management Strategies
Long-term care for these emergencies includes teaching patients about their condition. This includes:
- Diabetes Education: Teaching patients about managing diabetes, like checking blood sugar, using insulin, and making lifestyle changes.
- Lifestyle Modifications: Helping patients live healthier by eating well and staying active to manage their diabetes and avoid emergencies.
- Regular Follow-Up: Making sure patients see their healthcare providers often to check on their health and adjust treatment plans if needed.
By mixing quick actions with long-term care, we can handle hyperglycemic emergencies well. Our goal is to give full care and support to people with diabetes.
Treatment Options for Hypoglycemic Emergencies
When someone has a hypoglycemic emergency, quick action is key. Low blood sugar can cause serious problems if not treated fast.
Quick Response Actions
The first step is to give a fast-acting glucose source. Glucose tablets or gel work well because they are absorbed quickly. If the person can’t take glucose by mouth, a glucagon injection is needed. Glucagon helps by making the liver release glucose.
Key Quick Response Actions:
- Give glucose tablets or gel orally if the person is awake.
- Use glucagon injection if the person is asleep or can’t take glucose.
- Call emergency services if the person is not responding or symptoms don’t go away after treatment.
Post-Emergency Care
After treating the emergency, we focus on preventing future ones. We look at what caused the low blood sugar and adjust treatment plans. We work with patients to find out why it happened, like changes in medicine, diet, or exercise.
Post-Emergency Care Steps | Description |
Review Cause | Find out why the low blood sugar happened. |
Adjust Treatment Plan | Change medicine, diet, or exercise as needed. |
Monitor Blood Glucose | Keep a close eye on blood sugar to avoid future problems. |
By treating hypoglycemic emergencies thoroughly, we can greatly improve patient outcomes. This helps prevent future episodes.
The Importance of Education and Awareness
Education and awareness are key in handling endocrine emergencies. By teaching patients and keeping healthcare providers up-to-date, we can lower the number and impact of these crises.
Patient Education Initiatives
Teaching patients is vital in preventing and managing endocrine emergencies. We teach them to spot early signs, understand their health, and know when to get medical help. This includes showing them how to check their blood sugar, eat right, and adjust their meds.
We also give patients resources and support to manage their health well. This includes educational materials, support groups, and counseling. A broad approach to teaching patients can lead to better health and fewer emergencies.
Role of Healthcare Providers
Healthcare providers are essential in teaching patients about endocrine emergencies. They give accurate and timely info and make sure patients get their treatment plans. They also find at-risk patients and take steps to prevent problems.
Also, healthcare providers must keep up with new guidelines and best practices. This means ongoing education and training to give the best care. Working together with patients and healthcare providers leads to better outcomes in managing endocrine emergencies.
Conclusion: Prevention and Management
Preventing endocrine emergencies requires a few key steps. These include managing health conditions, making lifestyle changes, and keeping up with regular check-ups. Knowing the signs of hyperglycemic and hypoglycemic emergencies helps people take action early.
Effective Strategies for Reducing Risk
People with diabetes or endocrine disorders should team up with their doctors. Together, they can create a plan that fits their needs. This plan should include checking blood sugar often, eating well, and exercising right.
By doing these things, people can lower their chances of a hormone imbalance crisis.
Importance of Ongoing Monitoring
Seeing your doctor regularly is key to catching problems early. Being proactive helps manage health and avoid emergencies. We stress the need for ongoing monitoring and quick action to keep health on track.
FAQ
What is an endocrine emergency?
An endocrine emergency is a serious condition. It happens when hormone levels in the body get too high or too low. This needs quick medical help.
What are the most common types of endocrine emergencies?
Common endocrine emergencies include diabetic ketoacidosis and thyroid storm. Also, adrenal crisis, myxedema coma, hypoglycemia coma, and hyperosmolar coma are common.
What is diabetic ketoacidosis?
Diabetic ketoacidosis is a serious diabetes complication. It happens when the body makes too many ketones. This can be very dangerous if not treated.
What are the symptoms of hyperglycemic emergencies?
Symptoms include feeling very thirsty and urinating a lot. You might also feel tired, see things blurry, and in bad cases, have seizures or coma.
How can hypoglycemic emergencies be prevented?
To prevent hypoglycemic emergencies, manage your blood sugar well. Balance your insulin with food and exercise. Know the signs of low blood sugar early.
What is the role of patient education in managing endocrine emergencies?
Learning about endocrine emergencies is key. It helps people recognize signs early. They can then manage their condition better and get help when needed.
How are endocrine emergencies diagnosed?
Doctors use blood tests and other tests like thyroid function tests. They also do a clinical evaluation to diagnose endocrine emergencies.
What is the treatment for hyperglycemic emergencies?
Treatment includes giving fluids and insulin right away. It also involves long-term plans to avoid future problems.
How can lifestyle factors contribute to endocrine emergencies?
Poor diabetes care, bad diet, and health issues can lead to endocrine emergencies.
What is the importance of regular monitoring and check-ups in managing endocrine emergencies?
Regular checks help catch problems early. This reduces the risk of serious conditions.
Can endocrine emergencies be unpredictable?
Yes, they can be. Knowing the risks and managing them is important.
What is an adrenal crisis?
An adrenal crisis is when the adrenal glands don’t make enough cortisol. This is a serious issue.
How can a thyroid storm be managed?
Thyroid storm needs quick medical help. It involves lowering thyroid hormone levels and managing symptoms.
References
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2699722/