
Peripheral Artery Disease (PAD) is a serious condition. It happens when the arteries to the body’s limbs get narrowed. This can lead to severe health issues. The American Heart Association says PAD affects a lot of people. Lower-extremity PAD is the most common type.
It’s very important to catch PAD early. This helps manage the condition and prevent worse problems. Doctors use different diagnostic procedures to find PAD. These include simple tests and more detailed imaging methods.
Learn about peripheral artery disease diagnostic tests. Explore the crucial methods doctors use to detect PAD early and ensure your vascular health.
Key Takeaways
- PAD is a big problem that affects millions globally.
- Spotting PAD early is key to managing it well.
- There are many tests to find PAD.
- Simple tests are usually the first step.
- More detailed imaging might be needed later.
Understanding Peripheral Artery Disease (PAD)
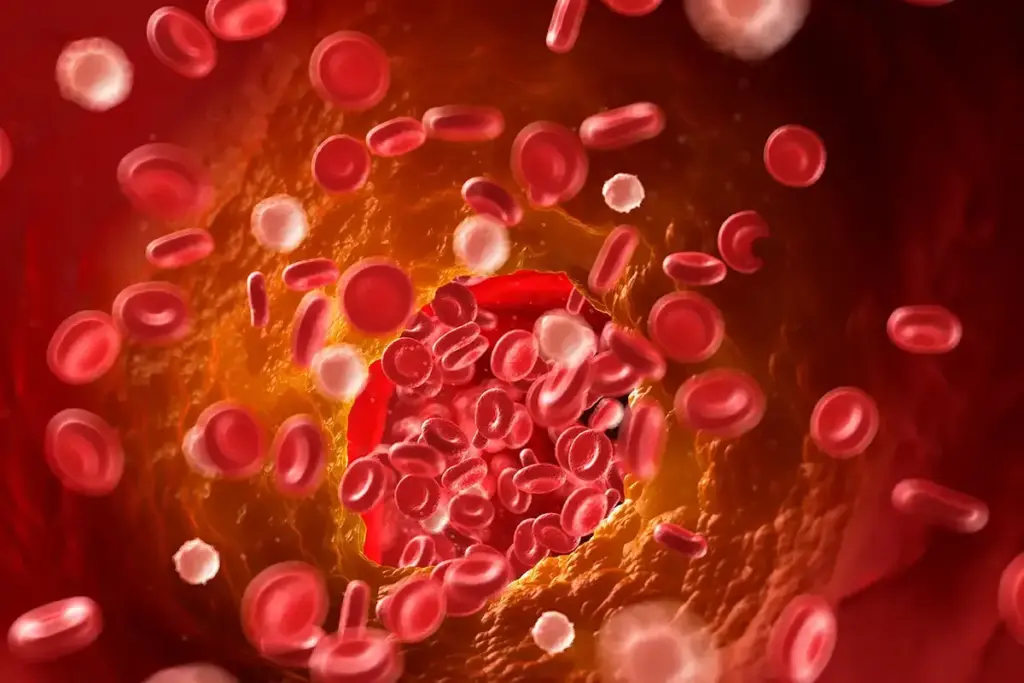
It’s important to know about Peripheral Artery Disease (PAD) to catch it early. PAD is a condition that affects the arteries outside the heart. It leads to less blood flow to the limbs.
What is Peripheral Artery Disease?
Peripheral Artery Disease (PAD) happens when plaque builds up in arteries. This causes them to narrow or block. It reduces blood flow to the legs and other areas, causing pain and discomfort.
The American Heart Association says PAD is a big warning sign. It shows atherosclerotic disease in the body, which can also harm the heart and brain.
Common Symptoms and Warning Signs
Symptoms of PAD include leg pain when walking, coldness, or weakness in the legs. Some people also feel pain at rest or have non-healing wounds on their legs or feet.
It’s key to catch these symptoms early. If you notice them, see a doctor for a peripheral artery disease evaluation.
Risk Factors for Developing PAD

Several things can increase your chance of getting PAD. These include smoking, diabetes, high blood pressure, high cholesterol, and a family history of PAD or heart disease.
Knowing these risk factors helps with prevention. If you have these risks, talk to your doctor. They can help with pad diagnosis and management.
|
Risk Factor |
Description |
Impact on PAD |
|---|---|---|
|
Smoking |
Damages the inner lining of blood vessels |
Increases the risk of PAD significantly |
|
Diabetes |
High blood sugar damages blood vessels |
Accelerates the progression of PAD |
|
High Blood Pressure |
Excessive pressure on artery walls |
Contributes to the development of PAD |
Early detection and treatment of PAD are key. They help prevent serious problems and improve life quality for those affected.
When to Seek Medical Evaluation for PAD
Knowing when to get medical help is key to catching PAD early. PAD often goes unnoticed until it’s too late. Getting help quickly is very important.
Recognizing Symptoms That Warrant Testing
If you feel pain in your legs when walking, or if they feel cold or numb, see a doctor. These signs mean your blood flow is low, a sign of PAD.
Common symptoms to watch out for include:
- Leg pain or cramping during physical activity
- Coldness or numbness in the legs or feet
- Weak or absent pulses in the legs
- Sores or wounds on the legs or feet that are slow to heal
High-Risk Groups Who Should Be Screened
Some people are more likely to get PAD and should get checked. The American Heart Association says people over 65, smokers, and those with diabetes should get screened.
|
Risk Factor |
Description |
|---|---|
|
Age |
65 years or older |
|
Smoking History |
Current or former smokers |
|
Diabetes |
Individuals diagnosed with diabetes |
The Importance of Early Diagnosis
Finding PAD early is vital to stop it from getting worse. The American Heart Association says early detection leads to better treatment. This can greatly improve life for those with PAD.
By knowing the risks and symptoms, you can get checked early. This could stop serious problems from happening with PAD.
Initial Clinical Assessment for PAD
A thorough initial assessment is key to spotting Peripheral Artery Disease (PAD) and planning further tests. It’s a detailed check that sets the stage for more tests.
Medical History Evaluation
The first step in assessing PAD is looking at the patient’s medical history. Doctors ask about symptoms, risk factors, and past health to spot PAD signs. They look for intermittent claudication, pain in the legs when walking, and other signs of poor blood flow.
Important parts of this evaluation are:
- Checking for risk factors like smoking, diabetes, high blood pressure, and cholesterol.
- Looking at the patient’s family history of heart disease.
- Recording any past vascular events or surgeries.
Physical Examination Procedures
Doctors perform a physical exam to find PAD signs. They check for:
- Leg signs of poor circulation, like hair loss, skin color changes, or ulcers.
- Leg pulses, including femoral, popliteal, posterior tibial, and dorsalis pedis.
- Leg and foot temperatures to see if they’re cool, which could mean less blood flow.
Initial Symptom Assessment
Doctors assess the patient’s symptoms to understand PAD’s impact. They look at the severity of intermittent claudication and how it affects the patient’s life.
|
Symptom |
Description |
Clinical Significance |
|---|---|---|
|
Intermittent Claudication |
Leg pain during walking that goes away with rest. |
Shows reduced blood flow to muscles during exercise. |
|
Rest Pain |
Pain in the legs or feet when not moving. |
Means severe PAD with a lot of ischemia. |
|
Non-healing Wounds |
Wounds on the legs or feet that won’t heal. |
Points to poor circulation and possible advanced PAD. |
The initial PAD assessment is a detailed process. It combines medical history, physical exam, and symptom check. This helps doctors decide the best next steps for diagnosing and treating PAD.
The Diagnostic Pathway for PAD
Diagnosing Peripheral Artery Disease (PAD) is a detailed process. It helps doctors from the first check to the final diagnosis. This method makes sure patients get the right diagnosis quickly, helping them get the right treatment.
Stepwise Approach to PAD Diagnosis
The PAD diagnosis starts with a detailed medical history and physical check-up. This first step helps find out who might need more tests. Early detection is key to managing PAD well. It lets doctors suggest lifestyle changes and treatments that can really help.
Next, doctors use non-invasive tests like the Ankle-Brachial Index (ABI) test. This test quickly checks blood flow in the legs. Other tests, like Doppler ultrasound and segmental pressure measurements, also help understand PAD better.
Primary Care vs. Specialist Evaluation
Primary care doctors are the first to check patients with PAD worries. They do the first checks and figure out who needs to see specialists.
When the diagnosis is not clear or more tests are needed, specialists step in. Vascular specialists do detailed tests like duplex ultrasound and angiography. They give a clear diagnosis and help decide the best treatment.
Diagnostic Algorithms Used by Physicians
Doctors use algorithms to make the PAD diagnosis process easier. These algorithms use what they find, risk factors, and test results to make decisions. This way, doctors make sure patients get a full check-up and the right diagnosis.
Algorithms also help pick the best tests and treatments for each patient. This makes the most of resources and helps patients get better faster.
The Ankle-Brachial Index (ABI) Test
The Ankle-Brachial Index (ABI) is a non-invasive test. It’s recognized for spotting Peripheral Artery Disease (PAD). The American Heart Association backs its effectiveness.
How the ABI Test Works
The ABI test measures blood pressure at the ankle and in the upper arm. It compares these to see how well blood flows to the lower limbs. A Doppler device and blood pressure cuff are used for this.
Step-by-Step Procedure:
- Measure blood pressure in the upper arm.
- Use a Doppler device to detect the pulse in the ankle.
- Inflate the blood pressure cuff around the ankle until the pulse is occluded, then slowly deflate it.
- Record the pressure at which the pulse returns.
- Repeat the process for the other ankle.
Interpreting ABI Results
The ABI result is found by dividing the ankle pressure by the arm pressure. An ABI of 0.9 or less means PAD. Values between 0.9 and 1.0 are borderline.
|
ABI Value |
Interpretation |
|---|---|
|
1.0 – 1.4 |
Normal |
|
0.9 – 0.99 |
Borderline |
|
0.5 – 0.89 |
Mild to Moderate PAD |
|
0.0 – 0.49 |
Severe PAD |
Limitations of the ABI Test
The ABI test is useful but has its limits. It might not work well for those with calcified arteries. This is because the arteries don’t compress fully, giving false readings. Also, an ABI over 1.4 can mean non-compressible arteries, common in diabetics.
Doppler Ultrasound for PAD Diagnosis
Peripheral Artery Disease diagnosis often uses Doppler ultrasound to check blood flow. This test is key for looking at vascular health and finding blockages or narrow spots in arteries.
Principles of Doppler Ultrasound
Doppler ultrasound detects changes in sound waves bouncing off moving blood cells. This lets doctors see how fast blood is flowing and spot any issues.
A probe sends out sound waves, which bounce off blood cells and come back. The changes in frequency help figure out blood flow speed, showing how arteries are doing.
What Doppler Ultrasound Can Reveal
Doppler ultrasound shows important things about vascular health. It can spot stenosis or blockages, check blood flow speed, and see blood flow direction. It helps find Peripheral Artery Disease by finding areas where blood flow is low or blocked.
This info is key for figuring out how bad PAD is and what treatment to use. Knowing where and how bad blockages are helps doctors plan better treatments.
Advantages and Limitations
Doppler ultrasound is non-invasive, making it safe and comfy for patients. It’s quick and gives results fast, helping doctors make quick decisions.
But, it has its downsides. The test’s accuracy depends on the person doing it. It might not show detailed artery pictures. It also struggles with very small or deep arteries.
Even with its limits, Doppler ultrasound is a big help in diagnosing and managing Peripheral Artery Disease. It gives real-time blood flow info, making it a key part of checking vascular health.
Peripheral Artery Disease Diagnostic Tests: Advanced Non-Invasive Options
Diagnosing Peripheral Artery Disease has become easier with new non-invasive tests. These tests give detailed insights into the blood vessels. They help doctors accurately diagnose PAD, understand its severity, and decide on treatments.
Segmental Pressure Measurements
Segmental pressure measurements take blood pressure at different leg levels. This test finds where and how bad the blockages are. Doctors can see how bad PAD is and track changes over time by comparing these readings.
Pulse Volume Recordings
Pulse Volume Recordings (PVR) track blood volume changes in the limbs with each heartbeat. It’s a non-invasive test that shows how well blood flows to the limbs. PVR is great for people with hard arteries, where other tests might not work as well.
Transcutaneous Oxygen Pressure Measurement
Transcutaneous Oxygen Pressure Measurement (TcPO2) checks if the skin gets enough oxygen. It shows if blood flow is good enough. TcPO2 helps figure out how bad the blood flow is and if a limb needs more blood flow.
Near-Infrared Spectroscopy
Near-Infrared Spectroscopy (NIRS) measures tissue oxygen levels and blood volume. It gives real-time info on blood flow in tiny blood vessels. NIRS helps see how well PAD treatments work and how well blood flows during and after exercise.
These new tests for PAD are big steps forward in vascular medicine. They let doctors give more accurate diagnoses and treatments. This leads to better care for patients.
Duplex Ultrasound Imaging for Arterial Assessment
Duplex ultrasound is a key tool for diagnosing Peripheral Artery Disease (PAD). It combines Doppler and conventional ultrasound. This method gives a detailed look at artery health, helping spot and treat PAD.
Differences from Standard Doppler Ultrasound
Duplex ultrasound is more advanced than standard Doppler ultrasound. It shows both the structure and function of arteries. Unlike Doppler, duplex ultrasound also uses conventional ultrasound. This lets doctors see the artery’s shape and check blood flow.
Key differences include:
- Anatomical visualization: Duplex ultrasound shows artery images, spotting stenosis, occlusions, and aneurysms.
- Functional assessment: It measures blood flow velocities, showing how arterial lesions affect function.
What Doctors Look for During the Test
Doctors examine several things during a duplex ultrasound for PAD. They look for:
- Stenosis or occlusions
- Blood flow velocities and waveforms
- Aneurysms or vascular abnormalities
Benefits of Duplex Ultrasound in PAD Diagnosis
Duplex ultrasound is great for diagnosing and managing PAD. It’s non-invasive, avoiding risks of invasive tests. It gives detailed info on artery anatomy and function, helping plan treatment.
|
Benefit |
Description |
|---|---|
|
Non-invasive |
Reduces the risk of complications |
|
Comprehensive assessment |
Provides both anatomical and functional information |
|
Aids in treatment planning |
Helps in deciding the appropriate intervention |
CT Angiography for PAD
CT angiography is a key tool for diagnosing Peripheral Artery Disease (PAD). It gives detailed images of the arteries. This method uses X-rays and contrast dye to spot blockages or narrowing in the arteries.
How CT Angiography Works
A patient lies on a table that moves into a CT scanner for this test. A contrast dye is injected into a vein to make the arteries stand out. The CT scanner then takes X-ray images from various angles.
These images are turned into detailed 3D pictures of the arteries. This helps doctors see exactly where and how severe any artery disease is.
Preparation for CT Angiography
Before the test, patients must not eat or drink for a few hours. They should also remove any jewelry or metal objects. It’s important to tell the doctor about any allergies, like to contrast dye, or kidney disease.
Risks and Benefits
CT angiography offers clear images of the arteries, helping with accurate diagnosis and treatment plans. But, it also has risks like radiation exposure and allergic reactions to the dye. The dye can also harm the kidneys, which is a concern for those with kidney problems.
What CT Angiography Can Reveal
CT angiography shows detailed info about the arteries, like stenosis or blockages. This info is key for choosing the right treatment for PAD. It could be medication, angioplasty, stenting, or surgery. CT angiography gives doctors the clear images they need to make the best decisions for patient care.
MRI Angiography for Peripheral Artery Disease
MRI angiography is a key tool for diagnosing Peripheral Artery Disease (PAD). It’s a non-invasive way to see the arteries. This helps doctors diagnose and plan treatment for PAD.
Principles of MRI Angiography
MRI angiography uses magnetic fields and radio waves to create images of arteries. It can be done with or without contrast agents. But, contrast-enhanced MRA is more common for PAD.
The method works because flowing blood looks different from stationary tissue. This lets us see blood vessels.
Patient Experience During MRA
During MRI angiography, patients lie very quietly in the scanner. The scanner can be open or closed, depending on the place. The procedure is usually painless.
But, some people might feel claustrophobic or uncomfortable because they have to stay very quiet for a long time. If contrast agents are used, they are given through an IV.
Advantages Over Other Imaging Methods
MRI angiography has many benefits over other methods for diagnosing PAD. These include:
- It’s non-invasive, which means it’s safer and has fewer risks.
- It gives very clear images that help doctors see how serious the blockages are.
- It doesn’t use harmful radiation, which is good for people who need to have many tests.
- It lets doctors see the arteries from different angles, which helps with planning surgery.
Limitations of MRI Angiography
Even with its benefits, MRI angiography has some downsides. These include:
- It can be more expensive than some other non-invasive tests.
- It’s not safe for people with certain metal implants, pacemakers, or severe fear of being closed in.
- It might sometimes make stenosis seem worse than it really is, mainly in smaller vessels.
Knowing these points is important for using MRI angiography effectively in diagnosing PAD.
Invasive Diagnostic Procedures for PAD
Non-invasive tests are often the first step in diagnosing Peripheral Artery Disease (PAD). But, some cases need more detailed tests. These tests give a clearer picture and help plan the right treatment.
Necessity of Invasive Testing
Invasive tests are needed when non-invasive ones don’t give clear results. They’re also used when detailed images of the arteries are needed. Angiography is a common test that uses dye to show blockages on X-rays.
Doctors decide on invasive tests based on several things. These include how bad the symptoms are, the patient’s health, and risk factors for PAD. Patients with severe symptoms or those needing surgery often get these tests.
Risks and Complications
Invasive tests are important for diagnosing PAD but come with risks. These include:
- Bleeding or hematoma at the site of catheter insertion
- Infection
- Allergic reactions to the contrast dye
- Damage to the blood vessels or nerves
- Kidney damage due to the contrast dye, mainly in those with kidney problems
Doctors carefully consider these risks against the benefits of a clear diagnosis. Choosing the right patients and preparing them well helps reduce risks.
In conclusion, invasive tests are key in managing PAD, mainly in complex cases. Knowing when to use them and their risks helps doctors make better choices.
Emerging Technologies in PAD Diagnosis
New technologies are changing how we diagnose Peripheral Artery Disease. These changes make diagnosing PAD more accurate and easier for patients. They also make the process more efficient.
Optical Coherence Tomography
Optical Coherence Tomography (OCT) is a new imaging method for PAD diagnosis. It shows detailed images of the arteries. This helps doctors see how severe the blockages are and plan treatments better.
Artificial Intelligence in PAD Detection
Artificial Intelligence (AI) is now used in PAD diagnosis. AI looks at lots of data from tests to find patterns doctors might miss. This helps catch PAD early and tailor treatments for each patient.
Point-of-Care Testing Advancements
Point-of-care testing (POCT) for PAD is getting better. Now, doctors can quickly test ABI and other important values right at the bedside. This is great for quick diagnoses in primary care and during patient visits.
Using these new technologies in medicine will greatly improve PAD diagnosis and care. As they keep getting better, they promise to help patients more and ease the healthcare system’s load.
Conclusion
Getting a correct diagnosis for Peripheral Artery Disease (PAD) is key to managing it well. There are many peripheral artery disease diagnostic tests out there. Each has its own good points and areas for improvement.
The Ankle-Brachial Index (ABI) test, Doppler Ultrasound, and imaging like CT Angiography and MRI Angiography are very important. They help a lot in PAD diagnosis.
For a full peripheral arterial disease assessment, doctors use both clinical checks and tests. Knowing about the different PAD screening methods helps doctors make better choices for their patients. This can lead to better results for people with PAD.
Spotting PAD early and treating it right can really cut down on serious problems. This includes heart issues and losing a limb. It’s very important for people at risk to get checked for PAD diagnosis quickly. Doctors also need to keep up with the newest ways to diagnose PAD.
FAQ
What is Peripheral Artery Disease (PAD)?
PAD is a condition where the arteries in the legs get narrowed or clogged. This reduces blood flow to the muscles.
What are the common symptoms of PAD?
Symptoms include leg pain when walking, cramping, numbness, or weakness. You might also feel coldness or see color changes in your legs or feet.
How is PAD diagnosed?
Doctors use a medical history, physical exam, and tests like the Ankle-Brachial Index (ABI) test. They also use Doppler ultrasound and imaging tests like CT or MRI angiography.
What is the Ankle-Brachial Index (ABI) test?
The ABI test compares ankle and arm blood pressure. It shows how severe PAD is.
What is Doppler ultrasound used for in PAD diagnosis?
Doppler ultrasound checks blood flow in arteries. It finds narrowing or blockages.
What are the benefits of duplex ultrasound in PAD diagnosis?
Duplex ultrasound combines Doppler ultrasound with traditional ultrasound. It gives a full view of arterial health.
What is CT angiography used for in PAD diagnosis?
CT angiography shows the arteries and finds narrowing or blockages. It gives detailed images of the arteries.
What are the advantages of MRI angiography in PAD diagnosis?
MRI angiography is non-invasive. It gives detailed images without ionizing radiation or iodinated contrast.
When are invasive diagnostic procedures necessary for PAD?
Invasive tests like angiography are needed when non-invasive tests are unclear. They’re also used when planning intervention.
What are the risks associated with invasive diagnostic procedures for PAD?
Risks include bleeding, infection, and damage to arteries or tissues. These risks are serious.
What emerging technologies are being used in PAD diagnosis?
New technologies like optical coherence tomography, artificial intelligence, and point-of-care testing are being developed. They aim to improve PAD diagnosis and management.
How can I prepare for a diagnostic test for PAD?
To prepare, avoid certain medications, fast, and wear comfortable clothes. Talk to your healthcare provider about what to do.
What is the importance of early diagnosis in managing PAD?
Early diagnosis is key. It allows for timely treatment to prevent complications and improve your quality of life.
Reference
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://pubmed.ncbi.nlm.nih.gov/28878945/





