Last Updated on November 20, 2025 by Ugurkan Demir
Getting a correct polycythaemia diagnosis is key for good treatment and safety. Polycythemia vera is a condition where too many red blood cells are made. It needs a detailed check to confirm it’s present. The diagnostic criteria include high red cell mass. This is often found with an erythrocytosis blood test showing high haematocrit or hemoglobin levels.
To diagnose polycythaemia, doctors look for the JAK2 mutation. This genetic change is common in those with this condition. The 2016 WHO criteria say that for an accurate polycythaemia diagnosis, you need high hemoglobin or hematocrit levels, the JAK2 mutation, and specific bone marrow findings.
Key Takeaways
- Polycythaemia diagnosis relies on identifying elevated red cell mass.
- Erythrocytosis blood tests are key for spotting high haematocrit or hemoglobin.
- The JAK2 mutation is a major genetic change in polycythemia vera.
- The 2016 WHO criteria outline major and minor criteria for diagnosis.
- A detailed polycythemia vera workup is vital for confirming the condition.
Understanding Polycythemia Vera and Its Clinical Significance

It’s key for doctors to understand polycythemia vera well. This is because it can lead to serious problems. A full approach is needed to diagnose and treat it.
What is Polycythemia Vera?
Polycythemia vera is a rare blood disorder. It causes too many red and white blood cells and platelets. Most cases come from a JAK2 gene mutation, which turns on a key signaling pathway.
Prevalence and Risk Factors
In the U.S., about 1.97 per 100,000 people have polycythemia vera. It usually starts in people over 60. Age and genetics, like the JAK2 V617F mutation, play big roles.
| Risk Factor | Description |
| Age | Increased incidence after 60 years |
| JAK2 V617F Mutation | Genetic mutation present in majority of cases |
| Family History | Possible increased risk with family history of myeloproliferative neoplasms |
Importance of Early and Accurate Diagnosis
Spotting polycythemia vera early is vital. It helps avoid serious issues like blood clots. Quick diagnosis means better care and fewer risks.
Early diagnosis offers many benefits:
- Less chance of blood clots
- Better control of symptoms
- Lower risk of turning into worse blood diseases
The Pathophysiology of Polycythemia Vera
Polycythemia vera has unique features, including the JAK2 mutation. This mutation is key to the disease’s development.
JAK2 Mutation and Its Role in Disease Development
The JAK2V617F mutation is found in about 95% of polycythemia vera patients. It activates the JAK-STAT pathway, leading to cell growth and survival. A study on clinical manifestations and diagnosis of polycythemia vera shows this mutation is a major diagnostic marker.
The JAK2V617F mutation does not directly affect PV survival or transformation rates. But, higher allele burdens are linked to fibrotic transformation.
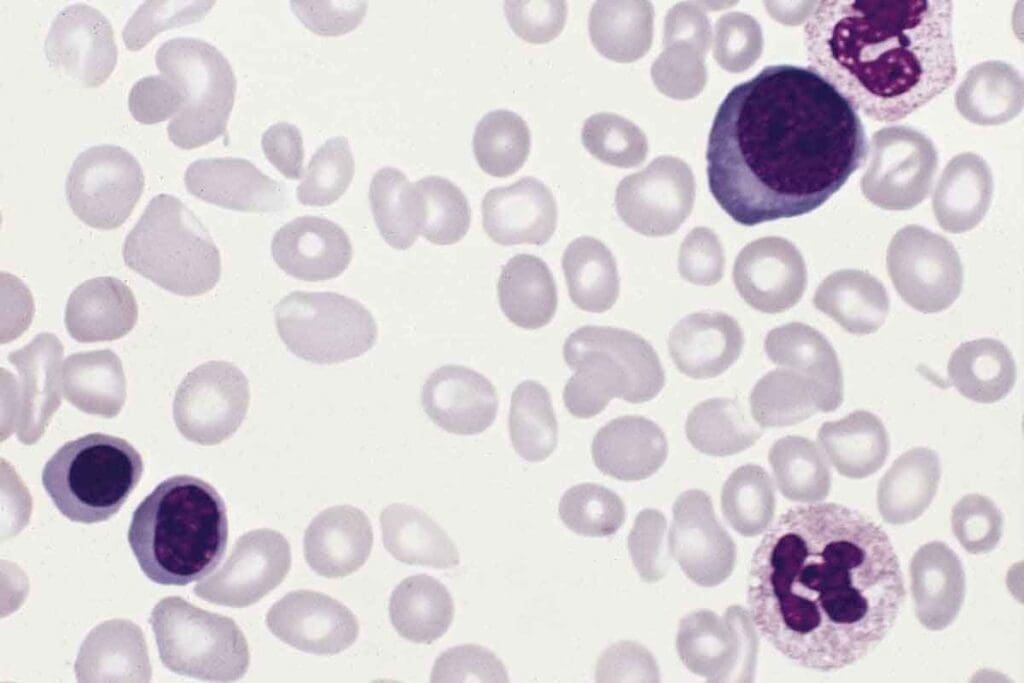
Bone Marrow Abnormalities
Bone marrow in polycythemia vera shows trilineage myeloproliferation. This means all three cell types grow too much.
The bone marrow in polycythemia vera is often very busy. It has too many red blood cell precursors. This leads to too many red blood cells.
| Characteristics | Normal Bone Marrow | Polycythemia Vera Bone Marrow |
| Cellularity | Normocellular | Hypercellular |
| Erythroid Precursors | Normal proportion | Increased proportion |
| Myeloid Lineage | Normal | Often increased |
Mechanisms of Erythrocytosis
Erythrocytosis in polycythemia vera comes from too many red blood cells. This is because of the abnormal growth of red blood cell precursors. The JAK2 mutation causes this by activating the JAK-STAT pathway.
Knowing how this works helps doctors diagnose and treat polycythemia vera better.
Clinical Presentation and Initial Evaluation
Polycythemia vera can show different symptoms, making it hard to diagnose. People might have non-specific symptoms or be found during blood tests for other reasons.
Common Signs and Symptoms
People with polycythemia vera might feel headaches, weakness, dizziness, and sweat a lot. These signs can also appear in other diseases, making it tough to figure out what’s wrong.
Common symptoms include itching, often after a bath, and a condition called erythromelalgia. This causes pain and redness in the hands and feet.
Physical Examination Findings
Doctors often find splenomegaly in polycythemia vera patients. This is seen in about 30-40% of cases. It can cause belly pain and help doctors diagnose the condition.
Distinguishing Primary vs. Secondary Polycythemia
It’s important to tell primary (polycythemia vera) from secondary polycythemia. Secondary polycythemia is caused by chronic low oxygen or other factors that raise erythropoietin levels.
| Characteristics | Primary Polycythemia (PV) | Secondary Polycythemia |
| Erythropoietin Level | Low | Normal or High |
| JAK2 Mutation | Present in majority | Absent |
| Splenomegaly | Common | Less Common |
Knowing the differences is key to correct diagnosis and treatment. A detailed check-up, including lab tests and genetic analysis, is needed to tell primary from secondary polycythemia.
The Complete Polycythaemia Diagnosis Approach
Diagnosing polycythemia vera is a detailed process. It combines clinical checks and lab tests. This method ensures patients get the right diagnosis and treatment.
Diagnostic Algorithm
The first step in diagnosing polycythemia vera is a detailed clinical check. This includes looking at the patient’s medical history and doing a physical exam. It helps spot signs that might point to the condition.
The 2016 WHO diagnostic criteria guide the diagnosis. They list major and minor criteria that must be met to confirm the diagnosis.
- Major Criteria:
- Hemoglobin or hematocrit above specific thresholds
- Presence of JAK2 mutation
- Bone marrow biopsy showing hypercellularity
- Minor Criteria:
- Serum erythropoietin level below the normal range
Stepwise Evaluation Process
The evaluation process for polycythemia vera has several steps:
- Initial clinical assessment and laboratory tests
- Complete blood count (CBC) to evaluate hemoglobin, hematocrit, and red blood cell count
- Genetic testing for JAK2 V617F mutation
- Bone marrow biopsy to assess hypercellularity
Coordination Between Laboratory and Clinical Assessment
Diagnosing polycythemia vera needs teamwork between lab results and clinical checks. The table below shows the key parts of this process.
| Laboratory Test | Clinical Significance |
| CBC | Evaluates hemoglobin, hematocrit, and red blood cell count |
| JAK2 Mutation Testing | Confirms presence of JAK2 V617F mutation |
| Bone Marrow Biopsy | Assesses bone marrow hypercellularity |
| Serum Erythropoietin Level | Helps differentiate primary from secondary polycythemia |
By combining lab results with clinical checks, doctors can accurately diagnose polycythemia vera. They can then create a good treatment plan.
Complete Blood Count: Detecting Erythrocytosis
A complete blood count (CBC) is key in finding erythrocytosis, a sign of polycythemia vera. Erythrocytosis means more red blood cells, which can make blood thicker and cause problems.
The CBC checks important levels like hemoglobin, hematocrit, and red blood cell count. These numbers tell a lot about a patient’s health.
Hemoglobin Thresholds for Diagnosis
Hemoglobin levels are very important for diagnosing polycythemia vera. A level over 16.5 g/dL in men and over 16.0 g/dL in women is too high. High hemoglobin levels show erythrocytosis.
“The 2016 World Health Organization (WHO) guidelines highlight the role of hemoglobin levels in diagnosing polycythemia vera,” experts say.
Hematocrit Evaluation
Hematocrit checks are also key in finding erythrocytosis. It shows the red blood cell percentage in the blood. A level over 49% in men and over 48% in women points to polycythemia vera.
- Hematocrit above 49% in men
- Hematocrit above 48% in women
These levels are important because they help tell the difference between primary and secondary erythrocytosis.
Red Blood Cell Count Analysis
Checking the red blood cell count is also important for diagnosing and managing polycythemia vera. More red blood cells mean erythrocytosis. The CBC gives an exact count, helping doctors treat the condition well.
In summary, a complete blood count is essential for finding erythrocytosis and diagnosing polycythemia vera. By looking at hemoglobin, hematocrit, and red blood cell count, doctors can make the right decisions for patient care.
The 7 Key Diagnostic Criteria for Polycythemia Vera
The 2016 WHO guidelines outline seven key criteria for diagnosing polycythemia vera. It’s important to understand these criteria. They help doctors accurately diagnose and differentiate from other myeloproliferative neoplasms.
Major Criteria According to 2016 WHO Guidelines
The 2016 WHO guidelines list three major criteria for diagnosing polycythemia vera. These include:
- Hemoglobin or Hematocrit Levels: Hemoglobin above 16.5 g/dL in men or hematocrit above 49%.
- JAK2 Mutation: Presence of JAK2V617F or JAK2 exon 12 mutation.
- Bone Marrow Findings: Typical bone marrow biopsy findings showing hypercellularity for age with trilineage growth (panmyelosis) including prominent erythroid, granulocytic, and megakaryocytic proliferation.
Minor Criteria and Their Significance
There is one minor criterion in addition to the major criteria:
- Subnormal Serum Erythropoietin Level: Low serum erythropoietin level.
To diagnose polycythemia vera, either all three major criteria must be present. Or, the first two major criteria and the minor criterion must be present.
Meeting Diagnostic Requirements
To meet the diagnostic requirements, the following conditions must be satisfied:
- All three major criteria must be present.
- Alternately, the first two major criteria and the minor criterion must be present.
Meeting these criteria ensures an accurate diagnosis. It follows the 2016 WHO guidelines.
Genetic Testing in Polycythemia Vera Workup
Genetic testing is key in diagnosing polycythemia vera. It finds specific genetic mutations. These mutations help doctors diagnose and manage the disease correctly.
JAK2 V617F Mutation Testing Methodology
The JAK2 V617F mutation is a major marker for polycythemia vera. Tests like allele-specific PCR or quantitative PCR check for this mutation in the JAK2 gene.
This testing is very accurate. It can find the mutation even in a few cells. This is important because the mutation might only be in some cells.
JAK2 Exon 12 Mutations
JAK2 exon 12 mutations are also important in diagnosing polycythemia vera. They are less common than JAK2 V617F but can also cause the disease.
Sequencing the JAK2 gene is used to find these mutations. This method can spot different mutations in exon 12 in patients with polycythemia vera.
Interpretation of Genetic Test Results
Understanding genetic test results for polycythemia vera needs expertise. A positive test for JAK2 V617F or exon 12 mutations supports the diagnosis. But, it’s important to look at all the diagnostic criteria together.
Doctors must consider the test results with other signs like blood counts and bone marrow findings. This helps make a correct diagnosis and plan the right treatment.
Bone Marrow Biopsy: Confirming Trilineage Hypercellularity
Trilineage hypercellularity is a key sign of polycythemia vera. It’s confirmed through a bone marrow biopsy. This test checks the bone marrow’s cells and spots any oddities linked to polycythemia vera.
Procedure and Patient Preparation
A bone marrow biopsy takes a sample by inserting a needle into the bone marrow. Patient preparation is key to avoid pain and issues. Patients get local anesthesia to numb the area.
The test is done in a clinic, and the sample goes to a lab for study. It’s important to handle and process the sample right for accurate results.
Characteristic Histological Findings
The biopsy sample is looked at for signs of polycythemia vera, like trilineage hypercellularity. This means more red, white blood cells, and platelets are made.
| Histological Feature | Description |
| Trilineage Hypercellularity | Increased production of red blood cells, white blood cells, and platelets |
| Pleomorphic Megakaryocytes | Variation in size and shape of megakaryocytes, indicative of myeloproliferative neoplasms |
| Fibrosis | Presence of reticulin or collagen fibrosis, which can be associated with disease progression |
When Bone Marrow Examination is Necessary
A bone marrow biopsy isn’t always needed for polycythemia vera diagnosis. It’s done when the diagnosis is unsure or to check for disease growth. The choice to do a bone marrow biopsy depends on clinical judgment and certain criteria.
In summary, bone marrow biopsy is a key test for finding trilineage hypercellularity and checking the bone marrow in polycythemia vera patients.
Additional Laboratory Tests for Complete Evaluation
After the first diagnosis, more tests are key to fully understand polycythemia vera. These tests help see how the disease is growing, rule out other issues, and help decide on treatments.
Serum Erythropoietin Levels
Erythropoietin (EPO) levels in the blood are very important for diagnosing polycythemia vera. Usually, EPO levels are low or suppressed in those with this disease. This is because the JAK2 mutation causes the body to make red blood cells without needing EPO. Testing EPO levels helps tell if someone has primary polycythemia vera or another reason for having too many red blood cells.
White Blood Cell and Platelet Count Analysis
Looking at white blood cell and platelet counts gives us important info on polycythemia vera. Leukocytosis (high white blood cell count) and thrombocytosis (high platelet count) are often seen in this disease. These findings show that all three types of blood cells are being made too much, which is a hallmark of this condition.
| Laboratory Test | Typical Findings in Polycythemia Vera |
| Serum Erythropoietin (EPO) | Low or Suppressed |
| White Blood Cell Count | Elevated (Leukocytosis) |
| Platelet Count | Elevated (Thrombocytosis) |
| Iron Studies | May show decreased iron stores |
Iron Studies and Other Relevant Tests
Iron studies are also key in the full check-up. People with polycythemia vera often have less iron because their bodies make more red blood cells. Other tests, like vitamin B12 and folate levels, might also be done. These can help find other problems or issues with blood cell production.
In summary, more tests are vital for a complete look at polycythemia vera. They help doctors understand the disease better, make a correct diagnosis, and plan the best treatment.
Conclusion: Ensuring Accurate Diagnosis and Next Steps
Getting a correct diagnosis is key to treating polycythemia vera well. Doctors use blood tests and genetic tests to find the condition. This helps them make a treatment plan that fits each patient.
People with polycythemia vera need regular check-ups and treatment to avoid problems. They might need to get blood drawn, take medicine, or change their lifestyle. These steps help manage the condition and lower the risk of serious issues.
It’s very important to get a right diagnosis for polycythemia vera. Knowing the diagnosis and treatment options helps patients work with their doctors. Together, they can manage the condition and get the best results.
FAQ
What is polycythemia vera, and how is it diagnosed?
Polycythemia vera is a rare blood disorder. It’s caused by too many red blood cells. Doctors use a blood test to find this. They also look for a specific gene mutation.
What are the 2016 WHO diagnostic criteria for polycythemia vera?
The WHO has clear criteria for diagnosing polycythemia vera. These include high hemoglobin levels and a specific gene mutation. They also look at the bone marrow.
What is the role of JAK2 mutation in polycythemia vera?
The JAK2V617F mutation is found in most polycythemia vera patients. It turns on a pathway that leads to the disease.
How is polycythemia vera distinguished from secondary polycythemia?
Primary polycythemia vera is a genetic disorder. Secondary polycythemia is caused by other factors, like low oxygen. Knowing the difference is key for treatment.
What laboratory tests are used to diagnose polycythemia vera?
Doctors use a blood count to check for too many red blood cells. They also test for the JAK2 mutation. Other tests include checking white blood cells and platelets, and a bone marrow biopsy.
What is the significance of bone marrow biopsy in polycythemia vera diagnosis?
A bone marrow biopsy is important. It shows if the bone marrow is too busy making blood cells. This helps confirm the diagnosis.
How are genetic test results interpreted in polycythemia vera diagnosis?
Genetic test results need careful analysis. Doctors look at the JAK2 mutation and other genetic changes. They consider all the test results together.
What are the next steps after a polycythemia vera diagnosis?
After diagnosis, patients need regular check-ups and treatment. This helps prevent serious problems and improves their life quality. Treatment may include blood removal, medication, and lifestyle changes.
What are the common signs and symptoms of polycythemia vera?
Symptoms include headaches, weakness, dizziness, and sweating. A big spleen can also be a sign.
How is the complete polycythaemia diagnosis approach implemented?
The diagnosis process involves a detailed plan. It includes blood tests and a thorough examination. This ensures accurate diagnosis and treatment.
References:
- Arber, D. A., Orazi, A., Hasserjian, R., Thiele, J., Borowitz, M. J., Le Beau, M. M., … & Vardiman, J. W. (2016). The 2016 WHO classification and diagnostic criteria for myeloproliferative neoplasms: polycythemia vera, essential thrombocythemia, and primary myelofibrosis. Blood, 127(20), 2391-2405.https://pmc.ncbi.nlm.nih.gov/articles/PMC5807384/





