
So, what is a colonoscopy? It’s a screening that finds and stops colon cancer. We’ll look into the procedure’s details, like how long it takes, to ease your worries.
Key Takeaways
- Colonoscopy is a key screening for colon cancer detection and prevention.
- Advances in sedation have made the procedure more comfortable.
- Regular screenings are essential for early detection.
- The procedure’s duration is typically relatively short.
- Patient-centered care enhances the overall experience.
What Exactly Is a Colonoscopy Procedure
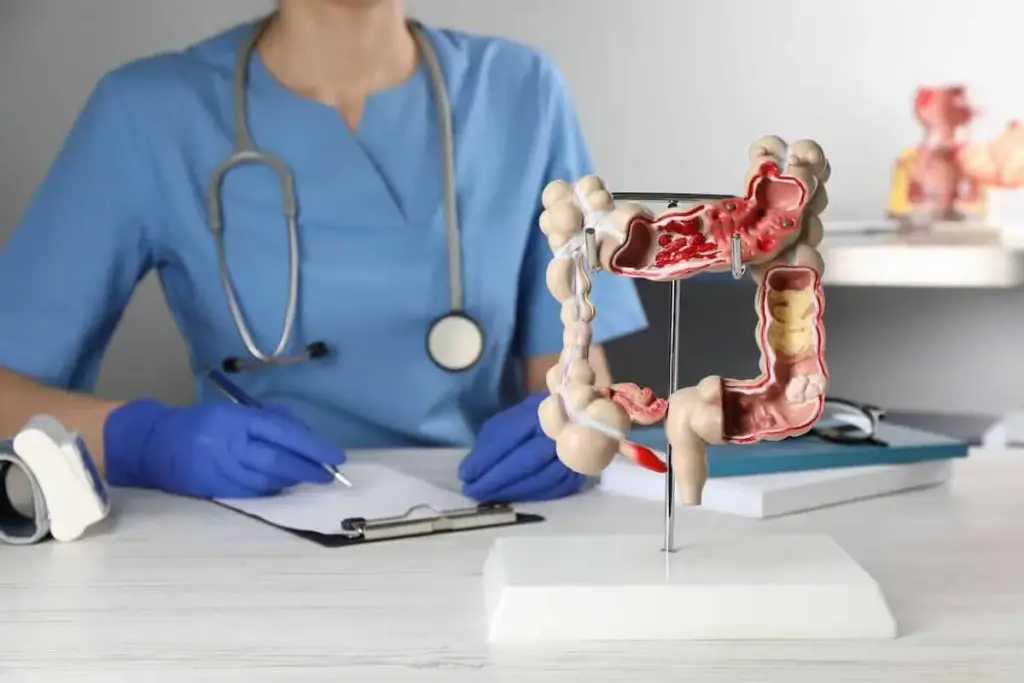
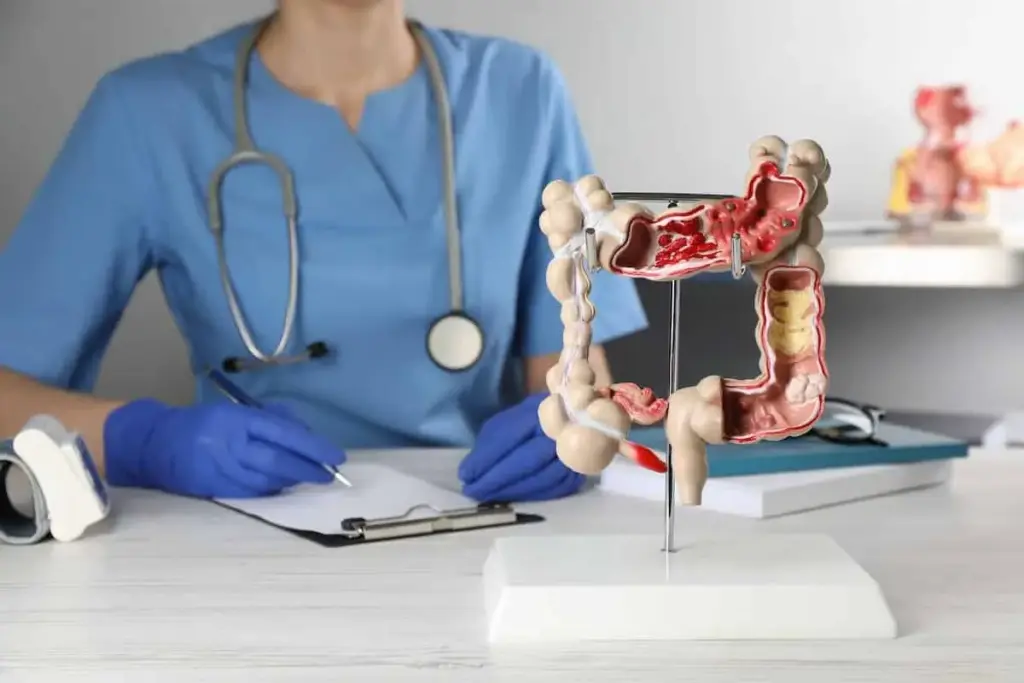
A colonoscopy is a medical test that lets doctors see inside the colon and rectum. It’s key for finding polyps, cancer, and other issues in the colon.
Medical Definition and Purpose
A colonoscopy uses a flexible tube with a camera and light, called a colonoscope. It checks the inside of the colon and rectum. The main goal is to spot polyps, which can be removed to stop them from turning into cancer.
The colonoscope sends images to a screen, so doctors can see the colon closely.
When Doctors Recommend This Procedure
Doctors suggest colonoscopies for many reasons. These include screening for colorectal cancer, looking into symptoms like rectal bleeding, and checking after polyp removal. How often you need a colonoscopy depends on your risk factors, medical history, and past results.
The table below shows when doctors might suggest a colonoscopy:
|
Recommendation Basis |
Description |
Typical Frequency |
|---|---|---|
|
Screening for Colorectal Cancer |
Routine check for individuals with average risk starting at age 45 |
Every 10 years if normal |
|
Family History or Risk Factors |
Earlier screening for those with family history of colorectal cancer or other risk factors |
Varied, often more frequently than every 10 years |
|
Previous Polyp Removal |
Follow-up after removal of polyps to check for new growths |
Typically every 3-5 years, depending on polyp characteristics |
The Truth About Pain During Colonoscopies
>People’s feelings about pain during colonoscopies vary a lot. Some feel little discomfort, while others feel more pain. It’s important to understand these differences to help patients.
Pain Perception Statistics and Studies
Studies have given us important information about pain during colonoscopies. About 30% of patients say they feel mild discomfort or brief pain. Sedation has been a big help in making the procedure less painful.
A study in a well-known medical journal showed most patients with sedation felt no pain or only mild discomfort. This shows how well sedation works in reducing pain.
Factors That Influence Pain Experience
Many things can affect how much pain someone feels during a colonoscopy. These include the patient’s health, any bowel diseases, and the doctor’s skill.
Sedation options are key in managing pain. Moderate sedation helps patients relax and feel less discomfort. Sometimes, deep sedation or general anesthesia is needed for those who are very anxious or expect a lot of pain.
The quality of bowel preparation is also very important. Bad preparation can make the procedure longer and more uncomfortable. This is because more effort is needed to clean the bowel well.
How much pain someone feels can also depend on their pain tolerance and past experiences with medical procedures. It’s vital for patients to talk to their doctor about their concerns and medical history. This way, they can find the best solution for their needs.
How Long Does a Colonoscopy Take From Start to Finish
Many people wonder how long a colonoscopy takes, from start to finish. Knowing this helps plan and eases anxiety about the procedure.
Pre-Procedure Preparation Timeline
Preparation for a colonoscopy starts a day or two before. You’ll need to change your diet and use bowel prep to clean your colon. Start with a clear liquid diet and follow the bowel prep instructions carefully.
The Actual Examination Duration
The actual procedure lasts 30 to 60 minutes. It can vary based on the complexity and your health. The gastroenterologist uses a camera to examine your colon and might take biopsies or remove polyps.
Recovery Time in the Medical Facility
After the procedure, you’ll go to a recovery area. You’ll be there for 30 minutes to an hour. This lets staff check that you’re okay from the sedation and there are no immediate problems.
Total Time Commitment for Patients
Plan to spend 2 to 3 hours at the medical facility. This includes check-in, preparation, the procedure, and recovery. It’s best to have someone drive you home because sedation effects last for hours.
In summary, the procedure itself takes 30-60 minutes. But, the whole process, including preparation and recovery, takes about 2 to 3 hours. Knowing what to expect can help ease anxiety and make the experience smoother.
Sedation Options That Minimize Discomfort
Sedation is key in making colonoscopies more comfortable. The thought of a colonoscopy can be scary. But, the right sedation can make it much easier.
Moderate Sedation (Conscious Sedation)
Moderate sedation, or conscious sedation, is often used for colonoscopies. It helps patients relax and feel more at ease. Key benefits include:
- Relaxation without losing consciousness
- Ability to respond to verbal commands
- Reduced memory of the procedure
This sedation is given through a mix of drugs like midazolam and fentanyl. They help with relaxation and pain relief.
Deep Sedation and General Anesthesia
Some patients might need deep sedation or general anesthesia. Deep sedation makes patients unresponsive but they can breathe on their own. General anesthesia makes patients completely unconscious and often requires a breathing tube.
|
Sedation Type |
Level of Consciousness |
Breathing Assistance |
|---|---|---|
|
Moderate Sedation |
Conscious, relaxed |
No |
|
Deep Sedation |
Unconscious, responsive to painful stimuli |
Usually not required |
|
General Anesthesia |
Completely unconscious |
Yes, often with a breathing tube |
Unsedated Colonoscopies: Who Might Choose This Option
Though sedation is used in most colonoscopies, some choose to go without. This might be due to personal preference or the need to quickly return to normal activities. Others might worry about sedation side effects.
Talking to a healthcare provider about the risks and benefits is important to see if an unsedated colonoscopy is right for you.
How Sedation Affects Pain Perception
Sedation greatly reduces discomfort during colonoscopies. It helps lower anxiety and promotes relaxation, which changes how pain is felt. Research shows that those who get the right sedation have a better experience and feel less pain.
It’s vital to talk to your healthcare provider about sedation options. They can help find the best choice for you.
Comprehensive Preparation for Your Colonoscopy
Knowing how to prepare for a colonoscopy is important. It makes the procedure smoother and more accurate. It also affects how comfortable you’ll be during the test.
Dietary Restrictions Timeline
Before your colonoscopy, you’ll need to eat certain foods. You should avoid nuts, seeds, and raw veggies for 1-3 days. Then, you’ll eat only clear liquids the day before. This includes broths, juices, and gelatin. Following these rules helps make sure your colon is clean for the test.
Bowel Preparation Process and Products
Cleaning your colon is a big part of getting ready for a colonoscopy. You’ll use products like polyethylene glycol (PEG) solutions or sodium phosphate. Your doctor will pick the best one for you. It’s important to follow the prep instructions to clean your colon well.
You’ll start the bowel prep the day before or early in the morning. Drinking a lot of the prep solution can be hard. But, it’s essential to finish it to get good results.
Common Preparation Mistakes to Avoid
There are mistakes that can mess up your colonoscopy prep. Not sticking to the diet, not doing the bowel prep right, and not telling your doctor about all your meds are common ones. Talking openly with your healthcare team helps avoid these mistakes and makes the procedure go smoothly.
- Not following the diet plan
- Not doing the bowel prep correctly
- Not telling your doctor about all your meds
By following these guidelines, you can make your colonoscopy more effective and comfortable.
Step-by-Step Walkthrough of the Colonoscopy Procedure
Knowing what to expect during a colonoscopy can make the experience less intimidating for patients. We will walk you through the process, from arrival at the medical facility to the completion of the procedure and immediate recovery.
Arrival and Initial Setup
Upon arrival, patients are directed to a pre-procedure area. They will change into a hospital gown. Our medical staff will review the procedure, discuss any concerns, and answer questions.
An intravenous (IV) line is usually inserted. This is to administer sedation and any necessary medications during the procedure.
Sedation Administration
Sedation is a key part of the colonoscopy procedure. It helps patients relax and reduces discomfort. The type and amount of sedation depend on the patient’s health and the doctor’s recommendations.
Our medical team will monitor the patient’s vital signs. They will adjust the sedation as needed to ensure comfort throughout the examination.
The Examination Process
Once sedated, the patient is positioned on an examination table. They are usually on their left side with knees drawn towards their chest. The colonoscope, a flexible tube with a camera and light, is gently inserted into the rectum.
The colonoscope is guided through the colon. The colon is inflated with air to provide a clearer view. The camera transmits images to a monitor for the doctor to examine.
The examination process typically takes about 30 to 60 minutes. The doctor may take biopsies or remove polyps if necessary. The colonoscope is carefully maneuvered to ensure a thorough examination while minimizing discomfort.
Completion and Immediate Recovery
After the examination is complete, the colonoscope is carefully withdrawn. The patient is taken to a recovery area. The medical staff will monitor the patient’s recovery from the sedation.
Patients are typically kept in the recovery area for about 30 to 60 minutes. They are monitored until they are fully awake and ready to be discharged.
To illustrate the steps involved in a colonoscopy procedure, here is a summary table:
|
Procedure Step |
Description |
Typical Duration |
|---|---|---|
|
Arrival and Initial Setup |
Patient check-in, changing, and IV insertion |
15-30 minutes |
|
Sedation Administration |
Administering sedation through the IV line |
5-10 minutes |
|
The Examination Process |
Insertion of the colonoscope and examination of the colon |
30-60 minutes |
|
Completion and Immediate Recovery |
Recovery from sedation and initial monitoring |
30-60 minutes |
Understanding these steps can help patients feel more prepared and less anxious about their colonoscopy. Our medical team is committed to making the experience as comfortable and stress-free as possible.
Physical Sensations: What Patients Actually Experience
The sensations during a colonoscopy can change based on the sedation type. It’s key to know that everyone’s experience is different.
Common Sensations During Sedated Procedures
Patients on sedation often find the procedure comfortable and relaxing. Sedation reduces discomfort, keeping patients calm. Most feel little to no pain during the procedure.
“I was surprised at how easy the procedure was,” says one patient. “I didn’t feel anything out of the ordinary, and the sedation made me feel relaxed.” Many share this feeling, showing how well sedation works.
Experiences During Unsedated Colonoscopies
Patients who choose not to use sedation may experience mild discomfort or pressure in their abdomen, which is typically short-lived and manageable.
Unsedated colonoscopies let patients get back to normal activities right away. But, it’s important to talk to a healthcare provider about this option.
Post-Procedure Discomfort and Management
After the procedure, some might feel mild bloating or gas pains. These symptoms are usually short-lived and can be eased with gas relief meds or walking.
Those sedated should have someone take them home, as they might feel groggy. The healthcare team will give post-procedure instructions, including how to handle any discomfort and when to start normal activities again.
In summary, while experiences can vary, knowing what to expect can ease worries. Talking to a healthcare provider helps patients make the best choice for their care.
Managing Anxiety and Emotional Distress About Colonoscopies
Many people feel anxious about getting a colonoscopy. It’s a common worry that affects a lot of people. We know it’s important to tackle this anxiety for a better experience.
Prevalence of Pre-Procedure Anxiety
About 50% of patients feel anxious before or during a colonoscopy. This anxiety comes from many sources, like fear of the unknown or worries about pain. Knowing how common this is is the first step to dealing with it.
Impact of Anxiety on Pain Perception
Anxiety can make pain feel worse during medical procedures. Studies show that more anxiety means more pain sensitivity. By managing anxiety, patients might feel less pain during the colonoscopy.
|
Anxiety Level |
Impact on Pain Perception |
|---|---|
|
Low Anxiety |
Generally lower pain perception |
|
Moderate Anxiety |
Increased sensitivity to pain |
|
High Anxiety |
Significantly higher pain perception |
Effective Techniques to Reduce Procedure Anxiety
There are ways to lower anxiety about colonoscopies. These include:
- Learning about the procedure
- Using relaxation methods like deep breathing or meditation
- Talking about sedation with your doctor
- Having support from loved ones
Using these methods can help lower anxiety a lot.
Communicating Concerns with Your Healthcare Team
Talking openly with your healthcare team is key. They can offer personalized advice and support. This helps manage anxiety and makes the procedure smoother.
We urge patients to share their worries. Our team is here to support you and make the colonoscopy as comfortable as possible.
Recovery After Your Colonoscopy: What to Expect
Knowing what to expect after a colonoscopy can make you feel less anxious. It’s important to understand the care steps after the procedure. This helps you get back to your daily life comfortably and safely.
Immediate Post-Procedure Effects
After the colonoscopy, you’ll go to a recovery area. It’s common to feel groggy or disoriented from the sedation. Medical staff will watch your vital signs and look for any bad reactions. Most people stay here for 30 to 60 minutes.
Some people might feel mild cramping or bloating as the air from the procedure leaves your colon. These feelings usually go away quickly. Our team will help you manage any discomfort and make sure you’re comfortable before you go home.
Going Home and First 24 Hours
We’ll give you specific instructions on how to care for yourself after the procedure. It’s recommended that you have someone accompany you home because sedation can affect your judgment and reaction times. For the first 24 hours, you should:
- Avoid driving or operating heavy machinery
- Refrain from making important decisions
- Rest and avoid strenuous activities
- Follow a light diet, gradually returning to your normal eating habits
Drinking plenty of fluids is key. If you have severe symptoms like heavy bleeding, severe abdominal pain, or fever, seek medical attention immediately.
When to Contact Your Doctor After the Procedure
Some discomfort is normal after a colonoscopy, but certain symptoms need medical attention. You should contact your doctor if you experience:
- Heavy or persistent bleeding
- Severe abdominal pain or cramping
- Fever or chills
- Signs of infection at the biopsy site
- Any other concerns or unusual symptoms
Our team is here to answer any questions or concerns. We want to make sure your recovery is as smooth and comfortable as possible.
Female Colonoscopy Procedure: Gender-Specific Considerations
Women thinking about a colonoscopy should know about the gender-specific parts of the process. The procedure is similar for men and women, but there are special things women should think about.
Addressing Women’s Unique Concerns
Women might worry about discomfort or the gender of the doctor during a colonoscopy. It’s important to talk about these worries to make sure the experience is comfortable and stress-free.
- Modesty and Comfort: Women can talk to their doctor about their concerns. The doctor can make sure they are comfortable and respected during the procedure.
- Gender Preference for Healthcare Providers: Some women might want a female doctor for their colonoscopy. We’ll look at how to ask for a female provider.
Options for Requesting Female Providers
Healthcare places often try to meet patient preferences, including who performs the procedure. Women who want a female doctor for their colonoscopy can:
- Ask Their Primary Care Physician: They can ask for a referral to a female gastroenterologist or a doctor experienced in colonoscopies.
- Contact the Healthcare Facility Directly: Many places let patients ask for a female doctor when they schedule the procedure.
By knowing about these gender-specific things and talking about their preferences, women can have a better colonoscopy experience.
When to Get a Colonoscopy: Age and Risk Guidelines
Deciding when to get a colonoscopy depends on age and risk factors. It’s important to know these guidelines to protect your health.
Current Screening Age Recommendations
The American Cancer Society suggests starting regular screenings at 45 for those at average risk. This advice is based on new research. It aims to catch colon cancer early, when it’s easier to treat.
“Regular screening starting at age 45 can significantly reduce the risk of colon cancer and its associated mortality.”
American Cancer Society
Early screenings can lead to better treatment results. The age for screenings might change based on your risk and family history.
Risk Factors That May Require Earlier Screening
Some risk factors mean you might need to start screenings before 45. These include:
- A family history of colon cancer or certain genetic syndromes
- A personal history of colon cancer or polyps
- A history of inflammatory bowel disease
|
Risk Factor |
Recommended Screening Age |
|---|---|
|
Family history of colon cancer |
10 years before the age of the relative’s diagnosis |
|
Personal history of colon cancer or polyps |
Following the removal of polyps or after colon cancer treatment |
|
History of inflammatory bowel disease |
8-10 years after diagnosis |
Talking to your doctor about your risk factors is key. They can help figure out the best screening plan for you.
Early detection through regular screenings can significantly improve treatment outcomes for colon cancer.
How Much is a Colonoscopy: Financial Considerations
Knowing the cost of a colonoscopy is key for those getting ready for it. The cost of medical tests can be scary, and colonoscopies are no different.
Several things can affect how much a colonoscopy costs. These include where you have the procedure, the doctor’s fees, and if you have insurance. We’ll look at each of these to help you understand what to expect.
Insurance Coverage for Preventive vs. Diagnostic Procedures
Insurance for colonoscopies can change a lot, depending on if it’s for prevention or diagnosis. Preventive colonoscopies, done as routine checks for people without symptoms, are often covered.
It’s important to talk to your insurance to know their rules and any costs you might face.
Options for Reducing Costs
If you don’t have good insurance or face high costs, there are ways to lower the cost of a colonoscopy:
- Negotiate with the provider: Some places might give discounts for paying cash upfront or negotiate prices.
- Seek out low-cost or free screening programs: Some groups and healthcare systems offer free or cheap colonoscopies. This is often for those at high risk of colon cancer or with little money.
- Consider outpatient facilities: Outpatient centers or ambulatory surgery centers might be cheaper than hospitals.
- Use generic or lower-cost alternatives for bowel prep: Using cheaper versions of bowel prep meds can help save money.
By knowing your insurance and looking into these cost-saving ideas, you can make a smart choice about your colonoscopy. This can help lessen the financial worry of this important health check.
Does a Colonoscopy Hurt: Addressing Common Fears
Many people worry about pain when they think about getting a colonoscopy. This fear is normal, given the procedure’s invasive nature. But, it’s important to know that today’s medical methods have greatly reduced any discomfort during and after the test.
Separating Myths from Facts About Pain
Some think colonoscopies are always painful. But, thanks to sedation, most patients don’t feel much pain. Sedation can range from light to deep, depending on the patient’s health and what they prefer.
Research shows that with the right sedation, most patients feel little to no pain. A study in the Journal of Clinical Gastroenterology found over 90% of sedated patients felt no pain or only mild discomfort.
|
Sedation Type |
Patient Experience |
|---|---|
|
Moderate Sedation |
Patients are relaxed and may remain awake or lightly sedated. |
|
Deep Sedation/General Anesthesia |
Patients are either deeply sedated or fully under anesthesia, feeling no pain. |
Real Patient Experiences and Testimonials
Patients who have had colonoscopies share their experiences. Many were nervous but felt little to no pain during the test.
“I was nervous about my colonoscopy, but the sedation made the whole experience painless. The medical staff were very reassuring and professional.” –
Anonymous Patient
These stories show how important it is to talk to your doctor and understand the role of sedation. By knowing the facts and hearing from others, you can feel more ready for your colonoscopy.
In summary, while pain is a big worry, modern sedation makes colonoscopies mostly pain-free. By learning the truth and hearing from others, you can face your colonoscopy with more confidence and less fear.
Alternatives to Traditional Colonoscopies
Not everyone may be comfortable with or suited for a traditional colonoscopy. This has led to the development of alternative screening methods. These options cater to different patient needs and preferences.
Virtual Colonoscopy: Benefits and Limitations
Virtual colonoscopy, also known as CT colonography, is a non-invasive imaging test. It uses X-rays and a CT scanner to produce detailed images of the colon. This method is great for patients who can’t have a traditional colonoscopy or prefer a less invasive option.
The benefits of virtual colonoscopy include:
- No need for sedation, reducing recovery time
- Less risk of complications compared to traditional colonoscopy
- Ability to visualize the colon without inserting a scope
But, virtual colonoscopy also has its limitations:
- Less sensitive for detecting small polyps or lesions
- If abnormalities are found, a traditional colonoscopy may be needed
- Exposure to radiation
A study in the Journal of the American Medical Association found virtual colonoscopy detected 90% of significant lesions. But, there were concerns about false positives needing additional testing (Source:
“CT Colonography in the National CT Colonography Trial: More False Positives Than Expected” –
Journal of the American Medical Association, 2008
).
Stool-Based Tests and Other Screening Options
Stool-based tests are another alternative to traditional colonoscopy. These tests detect hidden blood or DNA changes in the stool, which can be indicative of colon cancer. Examples include:
|
Test Type |
Description |
Frequency |
|---|---|---|
|
Fecal Occult Blood Test (FOBT) |
Detects hidden blood in the stool |
Annually |
|
Fecal Immunochemical Test (FIT) |
Detects antibodies to human hemoglobin |
Annually |
|
Stool DNA Test |
Detects DNA changes associated with colon cancer |
Every 3 years |
Stool-based tests are non-invasive and can be done at home. They are not as sensitive as colonoscopy or virtual colonoscopy for detecting polyps or early cancer. Yet, they are a valuable option for patients who are reluctant to undergo more invasive procedures or as a preliminary screening tool.
It’s essential to discuss these alternatives with your healthcare provider to determine the most appropriate screening method. This will depend on your individual risk factors, health status, and personal preferences.
Technological Advances Making Colonoscopies More Comfortable
Recent tech improvements have made colonoscopies more comfortable and effective. We’re in a new era in gastroenterology. Innovations are changing the colonoscopy experience for the better.
Improved Endoscopic Equipment
New endoscopic tools have made colonoscopies more comfortable. Modern colonoscopes are more flexible and smaller. This reduces discomfort during the procedure.
High-definition imaging also plays a big role. It helps doctors see better, making it easier to find and remove polyps.
Key advancements in endoscopic equipment include:
- High-definition imaging for clearer visuals
- Narrow-band imaging to enhance mucosal pattern visualization
- Improved flexibility for reduced discomfort
- Smaller diameter scopes for easier insertion
Enhanced Imaging and Computer-Assisted Technologies
New imaging and computer systems are changing colonoscopies. They help doctors find and remove polyps more accurately. This reduces risks and improves patient results.
|
Technology |
Description |
Benefits |
|---|---|---|
|
High-Definition Imaging |
Provides clear and detailed visuals of the colon |
Improved polyp detection, enhanced diagnostic accuracy |
|
Narrow-Band Imaging |
Enhances visualization of mucosal patterns and blood vessels |
Better characterization of polyps, improved diagnostic confidence |
|
Computer-Assisted Detection |
Uses AI to assist in detecting polyps during the procedure |
Increased adenoma detection rate, reduced miss rate |
These tech upgrades are making colonoscopies more comfortable and effective. As tech keeps improving, colonoscopies will get even better.
Conclusion: Balancing Concerns With Life-Saving Benefits
Colonoscopies are key in stopping colon cancer early. They remove polyps before they become cancer. Even though there might be some pain or discomfort, the benefits are much greater.
Getting regular colonoscopies can save lives. They help manage colon health in a proactive way. Knowing about the procedure, how to prepare, and sedation options helps patients make smart choices.
The benefits of colonoscopies are clear. Thanks to new technology, these tests are getting easier and more common. We urge everyone to talk to their doctors about their worries and options. This is the first step to a healthier life.
FAQ
What is a colonoscopy?
A colonoscopy is a way doctors look inside the colon. They use a flexible tube with a camera and light.
How long does a colonoscopy take?
The procedure itself takes 30-60 minutes. But, you should plan to spend 2-3 hours at the facility.
Does a colonoscopy hurt?
Some discomfort is possible, but most patients feel little to no pain. This is because of the sedation used.
What are the different sedation options for colonoscopies?
There are several sedation options. These include moderate sedation, deep sedation, and general anesthesia. The choice depends on your health and the doctor’s advice.
How do I prepare for a colonoscopy?
To prepare, you’ll need to follow dietary restrictions. You’ll also use a laxative or enema. Your healthcare provider will give you specific instructions.
What are the risks or complications of a colonoscopy?
Colonoscopies are generally safe. But, risks include bleeding and perforation of the colon. Rarely, there can be adverse reactions to sedation.
Can I request a female provider for my colonoscopy?
Yes, you can ask for a female provider if it makes you more comfortable. Many facilities will try to accommodate this request.
When should I get a colonoscopy?
Screening starts at age 45 for those at average risk. If you have a family history or other risk factors, you might need to start earlier.
How much does a colonoscopy cost?
The cost varies a lot. It depends on where you are, your insurance, and if it’s for prevention or diagnosis. Check with your insurance for details.
Are there alternatives to traditional colonoscopies?
Yes, there are alternatives. These include virtual colonoscopy and stool-based tests like FIT or Cologuard. Each has its own benefits and limitations.
How can I manage anxiety about getting a colonoscopy?
To reduce anxiety, try deep breathing and meditation. Talk to your healthcare team about your concerns. Understanding the procedure and its benefits can also help.
What should I expect during recovery from a colonoscopy?
After the procedure, you’ll be monitored for a short time. Then, you can go home. Make sure someone drives you and follow the post-procedure instructions carefully.
How long does it take to get the results of a colonoscopy?
Results are usually ready right after the procedure. But, if samples were taken, biopsy results might take a few days to a week.
References
[Unknown author]. (n.d.). Predictive model identifies painful sedation-free colonoscopy [Clinical trial listing]. Retrieved from https://www.centerwatch.com/clinical-trials/listings/NCT06635941/predictive-model-identifies-painful-sedation-free-colonoscopy










