Last Updated on November 20, 2025 by Ugurkan Demir

Pre-B acute lymphoblastic leukemia is a common cancer in kids, making up 75-85 percent of cases. At Liv Hospital, we know how tough it is for families when a child is diagnosed. Our care is all about supporting and guiding you through treatment.Get 7 key pre B acute lymphoblastic leukaemia facts. Learn about this serious B-Cell leukemia in children and its powerful impact.
We’re a top healthcare provider, dedicated to caring with compassion and understanding. In this article, we’ll share 7 key facts about B-cell leukemia in kids. This will help parents understand this complex condition better.
Key Takeaways
- Understanding the diagnosis of pre-B acute lymphoblastic leukemia
- The importance of timely and effective treatment
- Overview of the treatment process for B-cell leukemia
- Support services available for families
- Prognosis and long-term outcomes for children with B-cell leukemia
- The role of Liv Hospital in providing complete care
- Advances in medical research and treatment options
What is Pre-B Acute Lymphoblastic Leukaemia?
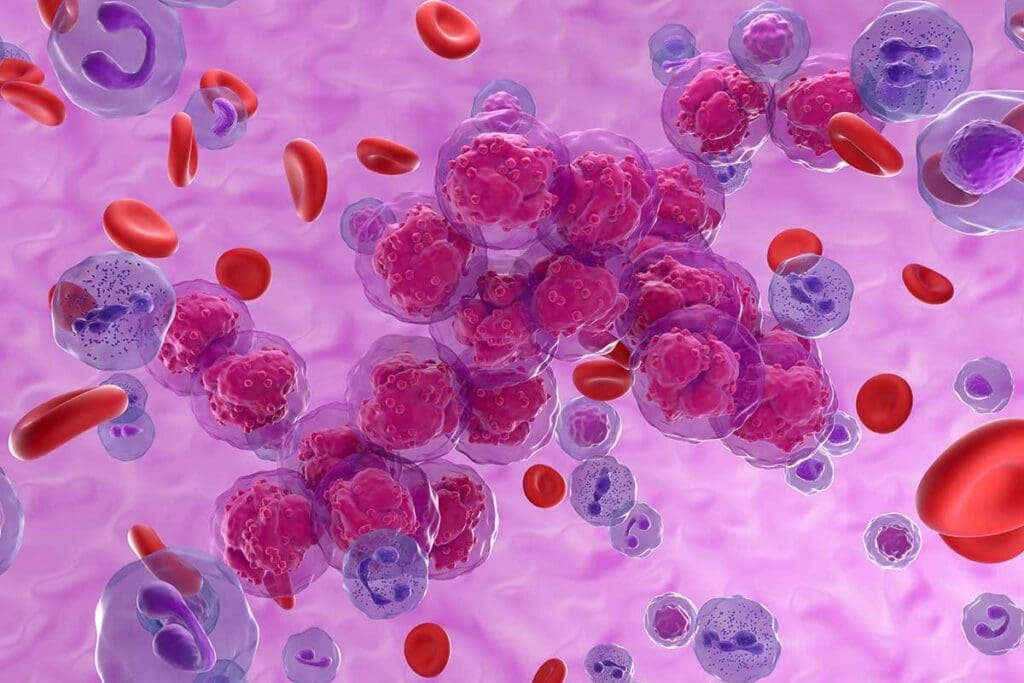
Pre-B Acute Lymphoblastic Leukaemia is a cancer that starts in B-cell precursors in the bone marrow. It affects the blood and bone marrow, causing too many abnormal white blood cells.
Definition and Classification of B-Cell ALL
B-cell Acute Lymphoblastic Leukemia (B-ALL) is a type of Acute Lymphoblastic Leukemia (ALL). It is divided based on the stage of lymphocyte development. B-ALL is characterized by the proliferation of malignant B lymphoblasts in the bone marrow, peripheral blood, or other organs.
The World Health Organization (WHO) classifies B-ALL into different subtypes. This is based on genetic and molecular features.
The Role of B Lymphocytes in the Body
B lymphocytes, or B cells, are key to the immune system. They produce antibodies to fight infections. B cells develop from hematopoietic stem cells in the bone marrow and mature into antibody-secreting plasma cells or memory B cells.
- B cells recognize and bind to specific antigens.
- They differentiate into plasma cells to produce antibodies.
- Some B cells become memory cells, providing long-term immunity.
How Malignant Transformation Occurs
Malignant transformation in B-ALL happens when B-cell precursors have genetic mutations. This leads to uncontrolled growth and a buildup of lymphoblasts in the bone marrow. It disrupts normal blood cell production, causing symptoms.
The exact reasons for these genetic mutations are not known. But both genetic predispositions and environmental factors are believed to play a role in B-ALL development.
Fact 1: Most Common Type of Childhood Leukemia

Pre-B Acute Lymphoblastic Leukaemia is the most common leukemia in kids. It’s a big deal in pediatric oncology. We’ll look at how common it is, compare it to other leukemias, and see when it usually happens.
Prevalence Among Pediatric Cancers
Pre-B Acute Lymphoblastic Leukaemia is a big part of pediatric cancers. It’s the top cancer in kids, making up about 80% of all childhood leukemia cases. This shows how important it is to keep studying it and finding better treatments.
Statistics on B-Cell ALL vs Other Leukemia Types
B-Cell ALL is a big deal in kids’ cancer. Here’s why:
- B-Cell ALL makes up about 85-90% of all Acute Lymphoblastic Leukaemia cases.
- Other leukemias, like Acute Myeloid Leukaemia (AML), are less common in kids.
- B-Cell ALL is way more common in kids than other leukemias.
Age Distribution and Peak Occurrence
Pre-B Acute Lymphoblastic Leukaemia is most often found in kids under 6. The most common time for diagnosis is between 2 and 5 years old. This age range is why we need to watch out for it more.
- The peak age range for diagnosis is between 2 and 5 years.
- Children under 1 year old have a different leukemia profile, often with different genetic traits.
- Older kids and teens can get it too, but it’s less common.
Fact 2: Unique Characteristics of Pre-B Acute Lymphoblastic Leukaemia
Pre-B Acute Lymphoblastic Leukaemia (ALL) has special traits that make it different from other leukemias. Knowing these traits is key to diagnosing and treating the disease.
Genetic and Molecular Features
Pre-B ALL has specific genetic and molecular changes. These changes affect how B lymphocytes develop and work. For example, the Philadelphia chromosome, caused by a chromosome swap, is a notable genetic feature in some cases.
Differences Between Childhood and Adult B-Cell ALL
B-Cell ALL in kids and adults has different traits and treatment responses. Kids with B-cell ALL usually do better because they respond well to chemotherapy. Adults with B-Cell ALL often face more aggressive disease and worse outcomes.
| Characteristics | Childhood B-Cell ALL | Adult B-Cell ALL |
| Prognosis | Favorable | Poor |
| Response to Chemotherapy | Highly sensitive | Less responsive |
| Genetic Features | Varied translocations and mutations | Often includes the Philadelphia chromosome |
Subtypes of B-Cell Lymphoblastic Leukemia
B-Cell Lymphoblastic Leukemia has subtypes based on genetic and molecular traits. These subtypes include those with specific chromosomal changes, like the MLL gene rearrangement or the ETV6-RUNX1 fusion. Knowing these subtypes helps doctors tailor treatments based on the patient’s risk level.
Understanding Pre B Acute Lymphoblastic Leukaemia’s unique traits helps doctors create better treatment plans. The genetic and molecular features, differences in kids and adults, and specific subtypes all guide treatment choices.
Fact 3: Risk Factors and Possible Causes
The exact causes of Pre-B Acute Lymphoblastic Leukaemia are being studied. Several risk factors have been found. Knowing these can help us understand who might get this disease.
Genetic Syndromes and Inherited Predispositions
Some genetic syndromes raise the risk of Pre-B Acute Lymphoblastic Leukaemia. For example, kids with Down syndrome are more likely to get B-cell ALL. Other conditions like Li-Fraumeni syndrome and ataxia-telangiectasia also increase the risk.
Environmental Exposures Including Radiation
Being exposed to ionizing radiation is a known risk factor. This includes radiation from medical treatments or nuclear accidents. Some studies also link certain chemicals and pesticides to increased risk.
Current Research on Causative Factors
Research is ongoing to understand genetic and environmental factors in Pre-B Acute Lymphoblastic Leukaemia. Recent studies look at genetic mutations and early-life exposures.
| Risk Factor | Description | Impact |
| Genetic Syndromes | Conditions like Down syndrome and Li-Fraumeni syndrome | Increased risk of developing B-Cell ALL |
| Radiation Exposure | Ionizing radiation from medical treatments or nuclear accidents | Known risk factor for Pre B Acute Lymphoblastic Leukaemia |
| Chemical Exposure | Exposure to certain chemicals and pesticides | Potential increased risk |
Understanding these risk factors helps us spot who might be at higher risk. This could lead to early detection and prevention strategies.
Fact 4: Recognizing the Warning Signs
It’s key to spot the warning signs of Pre B Acute Lymphoblastic Leukaemia (B-ALL) early. This helps in getting the right treatment fast. Knowing the common symptoms is the first step.
Common Symptoms in Different Age Groups
The signs of B-cell acute lymphoid leukemia differ by age. Kids, who often get B-ALL, might show:
- Persistent fatigue and pallor due to anemia
- Frequent infections resulting from a compromised immune system
- Easy bruising or bleeding due to low platelet counts
- Bone pain or joint pain caused by the accumulation of malignant cells in the bone marrow
In babies and toddlers, these signs can be hard to spot. They might look like usual childhood sicknesses. Older kids and teens might show more obvious signs, like:
- Unexplained weight loss
- Swollen lymph nodes, liver, or spleen
- Shortness of breath or other signs of anemia
How Symptoms Develop and Progress
The symptoms of B-cell leukemia in kids get worse as the disease grows. The bone marrow can’t make normal blood cells anymore. This is because malignant lymphoblasts take over, reducing healthy cells.
This leads to anemia, infections, and bleeding. Without treatment, B-ALL can get very serious, very fast.
When to Seek Immediate Medical Attention
Get medical help right away if your child has:
- Severe bleeding that doesn’t stop
- Signs of infection, such as fever, chills, or difficulty breathing
- Severe anemia, indicated by pale skin, shortness of breath, or dizziness
Early treatment of B-ALL can greatly improve chances of recovery. If you think your child might have B-cell acute lymphoid leukemia, see a doctor fast.
Fact 5: Diagnosis and Classification Process
Diagnosing Pre B Acute Lymphoblastic Leukaemia is a detailed process. It starts with an initial check and includes various tests. Early detection is key to successful treatment.
Initial Assessment and Blood Tests
The journey to diagnose acute lymphoblastic leukemia type B starts with a detailed medical history and physical check. Doctors look for signs like swollen lymph nodes and an enlarged liver or spleen. They also check for anemia or bleeding.
Blood tests are done to see if there are abnormal white or red blood cells and platelets.
A complete blood count (CBC) is often the first test. It can show if there’s anemia, low platelets, or too many white blood cells. These signs might mean leukemia is present.
Bone Marrow Examination Procedures
A bone marrow biopsy and aspiration are key for diagnosing leukemia type B. These tests take a bone marrow sample from the hipbone or another big bone. The sample is then looked at under a microscope to find cancer cells.
This test helps figure out the type of ALL and how far it has spread. It’s important for planning the right treatment.
Advanced Testing for Risk Stratification
After confirming pre-B acute lymphocytic leukemia, more tests are done to understand the risk. These include cytogenetic analysis, molecular testing, and immunophenotyping.
Immunophenotyping, for example, finds specific markers on leukemia cells. This helps diagnose the ALL subtype and plan a targeted treatment.
| Diagnostic Test | Purpose |
| Complete Blood Count (CBC) | To check for abnormal blood cell counts |
| Bone Marrow Biopsy and Aspiration | To examine bone marrow for cancerous cells |
| Cytogenetic Analysis | To identify genetic abnormalities in leukemia cells |
| Immunophenotyping | To identify specific markers on leukemia cells |
The process to diagnose Pre-B Acute Lymphoblastic Leukaemia is detailed and involves many tests. Knowing these steps helps us understand how complex diagnosing this condition is. It also shows why accurate diagnosis is so important for effective treatment.
Fact 6: Modern Treatment Approaches
Modern treatments have changed how we manage B-Cell ALL. Almost 90 percent of young patients get long-term remission with today’s therapies. We will look at the new strategies that have made a big difference in patient care.
Chemotherapy and Beyond
Chemotherapy is key in treating Pre-B Acute Lymphoblastic Leukaemia. It uses a mix of drugs to fight leukemia cells well.
We adjust treatment based on the patient’s risk level. This makes sure each patient gets the right treatment.
Stem Cell Transplantation Indications
Stem cell transplantation is for high-risk patients or those who have relapsed. It replaces the bone marrow with healthy stem cells from the patient or a donor.
“Stem cell transplantation has become a critical part in treating high-risk B-Cell ALL. It offers a chance for a cure for patients facing poor outcomes.”
- Nature Reviews Clinical Oncology
Targeted Therapies and Immunotherapy Advances
Targeted therapies and immunotherapy are new hopes in B-Cell ALL treatment. They aim to hit leukemia cells without harming normal cells.
Monoclonal antibodies and CAR-T cell therapy are showing great results in trials.
Managing Treatment Side Effects
It’s important to manage treatment side effects to improve patients’ quality of life. We use supportive care and adjust treatments as needed.
| Treatment Approach | Description | Indications |
| Multi-Agent Chemotherapy | A combination of drugs to target leukemia cells | First-line treatment for most patients |
| Stem Cell Transplantation | Replacing bone marrow with healthy stem cells | High-risk patients or those who have relapsed |
| Targeted Therapies and Immunotherapy | Selective targeting of leukemia cells | Patients with specific molecular characteristics |
In conclusion, modern treatments have greatly improved B-Cell ALL outcomes. Tailoring treatments and using new therapies are key to better patient care.
Fact 7: Promising Survival Rates and Outcomes
Medical treatments have greatly improved for kids with Pre-B Acute Lymphoblastic Leukaemia. This brings hope to families dealing with this condition.
Current Remission and Survival Statistics
Studies show a big jump in survival rates for kids with B-Cell Acute Lymphoblastic Leukemia. Now, over 90% of kids can get into complete remission. Many stay disease-free for a long time.
Factors That Influence Prognosis
Several things affect a child’s chances of beating Pre-B Acute Lymphoblastic Leukaemia. These include age at diagnosis, initial white blood cell count, how well they respond to treatment, and the leukemia’s genetic makeup.
Long-term Follow-up and Survivorship
With better survival rates, we focus more on long-term care. It’s key to watch for and manage treatment side effects. This ensures survivors get the care they need for life.
Recent Advances Improving Outcomes
Targeted therapies and immunotherapy are showing great promise. They’re being added to treatments, boosting survival chances and outcomes.
Conclusion
We’ve looked at 7 key facts about Pre-B Acute Lymphoblastic Leukaemia. This cancer affects B cells in kids. It’s the most common leukemia in children.
The facts showed us what makes this disease unique. We learned about its genetic and molecular features, risk factors, and symptoms. Knowing these is key to early diagnosis and treatment.
Modern treatments for B-cell leukemia in kids are showing great promise. Survival rates and outcomes have improved. We talked about how multi-agent chemotherapy, stem cell transplantation, and targeted therapies help manage this leukemia.
By sharing these facts, we aim to give a clear picture of Pre-B Acute Lymphoblastic Leukaemia and its treatments. This knowledge helps families and healthcare providers understand the disease better. It aids in making informed care decisions.
FAQ
What is Pre-B Acute Lymphoblastic Leukaemia?
Pre-B Acute Lymphoblastic Leukaemia is a blood and bone marrow cancer. It happens when immature B lymphocytes turn cancerous.
What are the symptoms of B-Cell ALL in children?
Kids with B-Cell ALL might feel tired, get sick easily, and bruise easily. Symptoms can differ by age.
How is Pre-B Acute Lymphoblastic Leukaemia diagnosed?
Doctors first check with blood tests and bone marrow exams. They also do advanced tests to figure out the risk level.
What are the treatment options for B-Cell Lymphoblastic Leukemia?
Treatments include chemotherapy, stem cell transplants, and new therapies. These aim to kill cancer cells and help the body fight back.
What is the prognosis for children with Pre-B Acute Lymphoblastic Leukaemia?
The outlook depends on age, how well the treatment works, and genetics. But most young patients can live long, healthy lives with today’s treatments.
Are there any risk factors associated with developing B-Cell ALL?
Yes, certain genetic syndromes, inherited traits, and radiation exposure can increase the risk.
How do treatment side effects get managed in patients with Pre-B Acute Lymphoblastic Leukaemia?
Doctors use a wide range of methods to help manage side effects. This includes supportive care and watching for any complications.
What is the role of B lymphocytes in the body?
B lymphocytes are key to our immune system. They make antibodies to fight off infections.
Can Pre-B Acute Lymphoblastic Leukaemia be cured?
Yes, with today’s treatments, many kids with Pre B Acute Lymphoblastic Leukaemia can live long, healthy lives. Some might even be considered cured.
References:
- Ding, F., et al. (2025). Analysis of global trends in acute lymphoblastic leukemia in children. BMC Pediatrics, 25, Article 123. https://pmc.ncbi.nlm.nih.gov/articles/PMC11966407/
- de Sousa, D. W. L. (2015). Acute lymphoblastic leukemia in children and adolescents. Revista Brasileira de Hematologia e Hemoterapia, 37(3), 244-247. https://pmc.ncbi.nlm.nih.gov/articles/PMC4519710/